Surgeons’ views on presbyopic lenses are just one facet of the lens topics tackled in this month’s e-survey on IOLs. The e-mail survey was opened by 1,699 of the 11,708 subscribers to Review’s electronic mail service (14.5 percent open rate) and, of those, 99 surgeons (6 percent) shared their responses.
Presbyopic IOLs
Surgeons are very interested in offering patients a lens solution to their presbyopia, with 72 percent saying they offer presbyopic lenses in their practice.
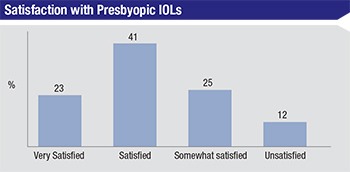
On this year’s survey, 23 percent of the surgeons say they’re very satisfied with the presbyopic lens they use the most, and 41 percent say they’re satisfied with it. On the other end, a quarter of surgeons say they’re only somewhat satisfied with their presbyopic lens of choice, with another 12 percent identifying as unsatisfied with their lens—this is up from 5 percent who said they were unsatisfied with their presbyopic lenses in last year’s survey. In terms of the lenses surgeons use most often, 41 percent say they use the Alcon ReSTOR, 32 percent use the Tecnis Multifocal and 27 percent reach for the Crystalens first.
Though many surgeons use these lenses, they note that there’s room for improvement in the designs. “Reading performance is good,” says George Walters, MD, of Port Arthur, Texas, who uses the Tecnis Multifocal most often. “But a newer model with a lower add would be beneficial.”
|
A vocal minority of doctors doesn’t like the qualitative vision issues that patients may experience with multifocal lenses. “I’m very happy with it,” says a surgeon from Pennsylvania. “I’d like to see a lens that has fewer halos at night.” Another surgeon from Pennsylvania thinks some new designs are in order. “There’s a diminished quality of vision and contrast sensitivity,” he says. “They should make a lens with optics like those in multifocal contact lenses.” An Iowa surgeon is on the fence about these lenses. “Some people just don’t see well and require an IOL exchange, and then they are happy,” he says. “I wish I could tell who this would be first. I’m almost thinking of stopping offering them. It just seems like it’s such a downer for them and for us.”
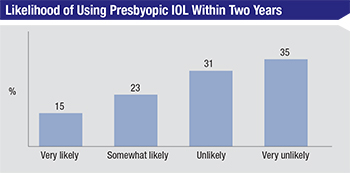
Looking ahead, 15 percent of surgeons who don’t currently use presbyopic IOLs say they’re very likely to use them within two years. Twenty-three percent are somewhat likely to do so. Thirty-one percent say they’re unlikely to begin using them (compared to 26 percent last year) and 35 percent say they’re very unlikely to start implanting them, which is a large increase from last year’s 11 percent. “I’ll use presbyopic IOLs if a truly accommodative lens becomes available,” says Luther Fry, MD, of Garden City, Kan. “I won’t use multifocals.” One surgeon doesn’t think the technology is there yet. “I am not satisfied with the results we can achieve with these lenses and I’m unsatisfied with the methods we have to correct things if and when a patient is not happy,” he says. “A lens exchange after a YAG is a risky procedure.”
 |
 |
 |
Toric Lenses
Toric IOLs remain one of the most popular types of premium lens, with 75 percent of the respondents saying they implant them. Most of the surgeons are very pleased with the outcomes torics achieve. Sixty-one percent of the surgeons say toric outcomes are excellent, 31 percent rate them as fair and only 9 percent call them poor.
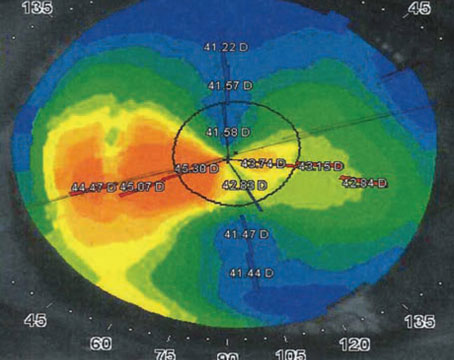
“In appropriate patients, the torics are excellent. If implanted properly, there is no downside to correcting corneal astigmatism,” says one surgeon who chose to remain anonymous. “In keratoconus patients who are stable over a few years with regular astigmatism, and don’t plan on using postoperative RGP lenses, I will consider a toric as well.” Robert Mobley, MD, of Clinton Township, Mich., also thinks they work well in the right patients, as well. “Toric lenses are highly recommended for greater than 1 D of against-the-rule astigmatism or greater than 1.25 D of with-the-rule astigmatism,” he says.
A surgeon from Indiana says torics are good lenses, but surgeons should undertake implanting them with their eyes open to possible challenges. “Toric IOLs work,” he says. “However, they present a challenging value proposition, because they require just as much, or more, surgeon acumen and diagnostic equipment savvy and more surgical work, as other IOLs do. Their cost is significant to patients because of that. Also, patients will still need glasses postop, so patient goals can’t be completely met with them, especially for the price.” A surgeon from Iowa agrees, saying, “You’ve got to get everything right—including posterior corneal astigmatism. This seems easy but is actually very demanding and requires regimentation and discipline.” Dr. Fry likes them, but thinks expense is an issue. “I recommend them for everyone with over 1 D of cylinder,” he says. “I provide free LRIs for 1 D or less. Unfortunately, [toric lenses] are too expensive and many patients can’t, or won’t, afford them. I wish they were around $200, so we could provide them to our patients affordably.”
A couple of surgeons lament that, despite torics’ popularity and overall good results, they’re not always completely accurate. “I still usually get 0.5 to 0.75 D of cylinder in patients’ refraction afterwards,” says a surgeon from California, “despite seemingly accurate measurements and good axis placement.”
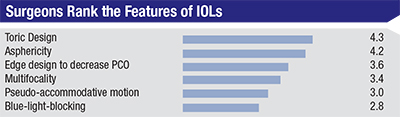
Lens Design
In terms of the monofocal lens surgeons use for most of their cases, 51 percent use the Alcon IQ Aspheric, 26 percent prefer the AMO Tecnis and 6 percent use the Bausch + Lomb Akreos MICS lens. The Lenstec Softec HD and B+L enVista are next with 3 percent of the vote each, and with 2 percent of the vote each are the B+L SofPort AO, the Hoya iSymm/iSert, the Rayner C-flex and the B+L Akreos AO.
A surgeon from Los Angeles says he likes using the IQ Aspheric. “It’s easy to implant, rotate and center,” he says. A Tecnis user from New Jersey says, “It has been reliable and the patients are happy,” while Texas’ Dr. Walters, who prefers the B+L Akreos MICS lens, says, “It centers well and the patient can get pseudo-accommodation. It’s very biocompatible with no discolorations or glistenings.”
Managing Problems
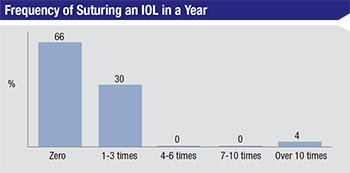
To get a handle on how often things go awry with IOLs, surgeons were also asked about times when they had to suture-fixate a lens or explant one. Two-thirds of the respondents say they never have to suture a lens in any given year, 30 percent say they have to suture one to three lenses and 4 percent say they do it more than 10 times.
Surgeons give a variety of reasons for suturing the lenses. “I’ll use iris suture fixation due to poor capsular support,” avers Juan Nieto, MD, of Dubuque, Iowa. Steven Safran, MD, of Lawrenceville, N.J., says he often gets referrals for lens fixation. “I do it for patients referred in with a dislocated lens or an anterior chamber IOL that needs to be exchanged,” he says. Some surgeons are even beginning to move away from sutures to a new method of fixation. “I’m tending toward a glue technique for PC-IOL fixation more often than sutures now,” says a surgeon from Illinois.
Surgeons say lenses sometimes need to be explanted, as well. The most common reasons for explantation cited are:
• incorrect lens power;
• dislocation;
• poor vision/glare from a multifocal lens;
• IOL damage; and
• trauma.
Kentucky’s Dr. Ballard recalls one instance when the implantation and explantation occurred the same day. “I implanted the wrong intraocular lens during surgery,” he says. “Two minutes after the patient’s transfer to the post-procedure care unit, I wheeled her back to the OR and explanted the lens and implanted the correct one.” REVIEW