By now, most surgeons are well-versed on how to use preop diagnostics, treatments and patient counseling to optimize premium IOL results. But few discuss what to do when a case doesn’t go as planned. Postop problems—so familiar in this age of targeting perfect vision—may include exacerbations of dry eye, residual refractive error and astigmatism, other forms of ocular surface disease, unexpected retinal issues and dysphotopsias—to name a few. In this review, surgeons explain how they’ve overcome many of these challenges and how they now safeguard against repeat episodes.
Not What You Think?
A study of 74 eyes of patients after the implantation of presbyopia-correcting intraocular lenses found that unreasonable expectations as a cause of postop dissatisfaction was a factor in only 8 percent of the surgeries evaluated.1 So much for the notion that patients are often dissatisfied with the results of premium cataract surgery because they have unreasonable expectations before reaching your table. The study was a retrospective review of the clinical records of patients who had reported one or more sources of postop dissatisfaction between January 2009 and December 2013 at the Bascom Palmer Eye Institute. A total of 57 percent of all cases involved residual refractive errors and 35 percent, dry eye, according to the study. (For other leading causes of dissatisfaction found in this study, see Figure 1 below.)
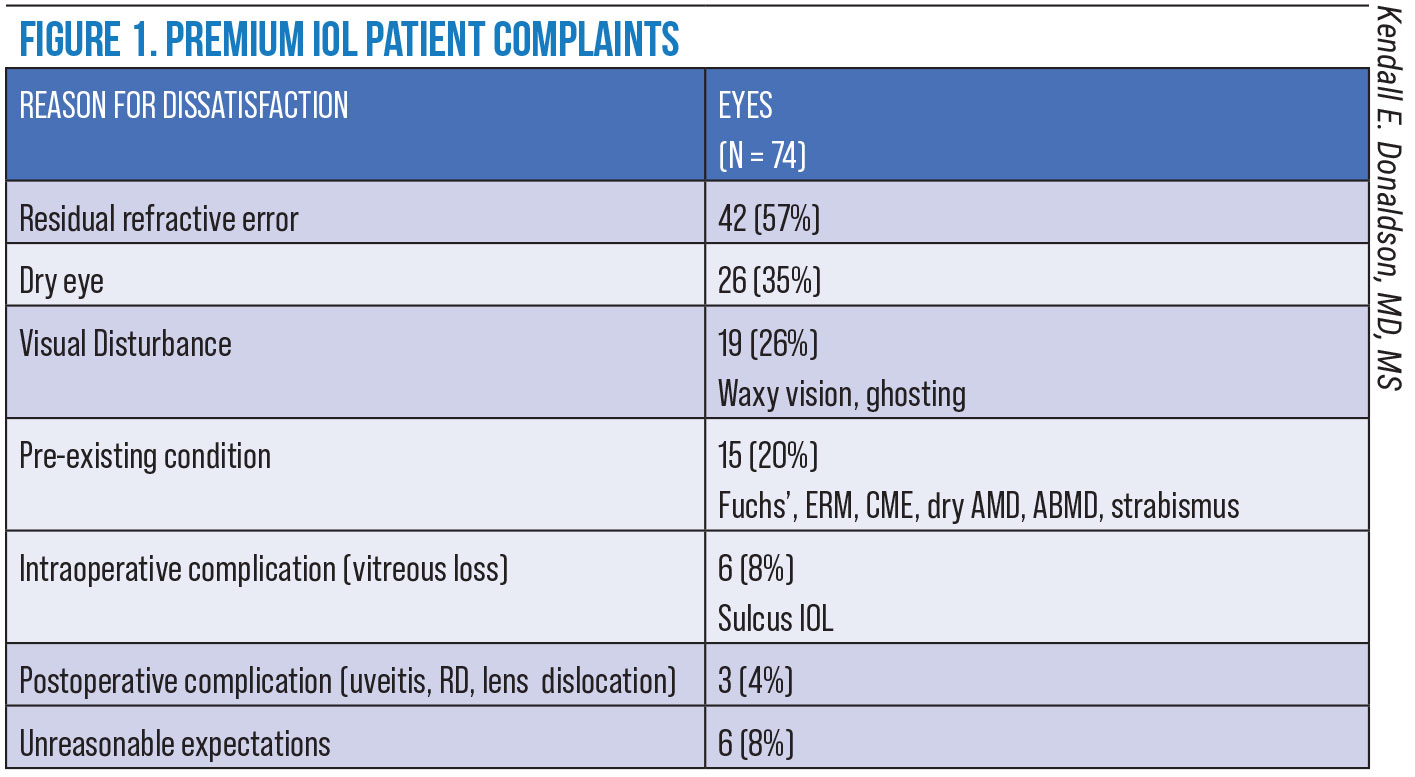 |
|
Residual refractive error after premium cataract surgery was surprisingly high, at 57 percent, in this study. Gibbons A, Ali TK, Waren DP, Donaldson KE. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol 2016;10:1965-1970. |
The most common symptom underlying all complaints was blurry or foggy vision, both for distance and near vision. A single treating physician determined probable causes of dissatisfaction and provided remedies that included glasses, contact lenses, dry-eye therapy, laser vision correction and IOL exchanges. Significantly, 23 percent of treated patients were only partially satisfied with their final results and 32 percent remained completely dissatisfied. The findings suggest a need for a deeper search for causes of patient unhappiness after implantation of premium IOLs, refinement of postop treatments and, of course, increased diagnostic vigilance before surgery to ensure that potential causes of dissatisfaction are identified and successfully resolved before they create postop problems, according to Kendall Donaldson, MD, MS, one of the authors of the study.
“We can do a better job of getting these patients to 20-happy,” says Dr. Donaldson, a professor of clinical ophthalmology at Bascom Palmer in Miami, Florida. “Our objective should be to end up within 0.5 D of our refractive target. How can we make sure we achieve this every time? That’s the key question that we must try to answer. Equally important is the emergent question we face in the context of this report: What can we do to reverse—or at least significantly mitigate—a negative patient outcome?”
Fixing Residual Refractive Errors
If the problem for your unhappy patient is a residual refractive error, Dr. Donaldson, also a professor of cornea/external disease, cataract and refractive surgery at Bascom Palmer, emphasizes the importance of identifying the cause and extent of the error.
“Is it the wrong IOL for that eye?” she asks. “Does the patient have an underlying condition that was missed, such as ocular surface disease, anterior basement membrane dystrophy, Salzmann’s nodular degeneration or an irregular eye that’s perhaps too long, short, or presenting with staphyloma? Was the problem anticipated and discussed with the patient preoperatively? Does the patient have a history of LASIK, PRK or RK that’s playing a role in his or her unexpected outcome? Is irregular astigmatism a factor?”
Other possibilities to consider, she continues, include less-than-adequate effective lens position, posterior corneal astigmatism and, sometimes, unknown reasons (when all testing appears normal but the patient is unhappy with the quality of vision).
“In all of these cases, we always check for ocular surface disease that might have been missed preoperatively and, if present, promptly treat it,” Dr. Donaldson says. “We can adequately treat some of these other conditions, such as AMBD with a superficial keratectomy, but some ocular surface conditions are chronic and can only be improved, not cured. Remember, though, that we sometimes need to wait for patients to neuroadapt to their new vision. When the time is right, providing laser vision correction as an enhancement can often be a good solution in many of these cases. If the residual refractive error is large, I’ll consider an IOL exchange, implantation of a piggyback IOL or again, if appropriate, laser vision correction.”
Of course, how you address a residual refractive error will be determined by the type of correction needed, Dr. Donaldson continues. “Myopes are typically easy to treat with LASIK, which the patient will usually find tolerable,” notes Dr. Donaldson. “Hyperopes can be more challenging to treat with LASIK or PRK and, as an alternative, may require an IOL exchange.”
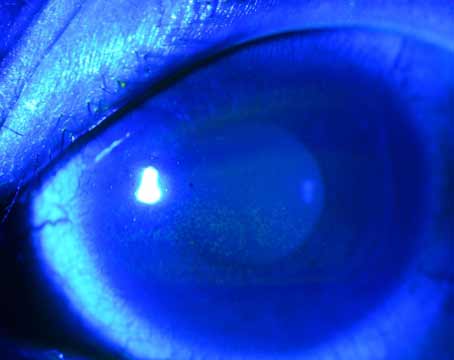
 |
|
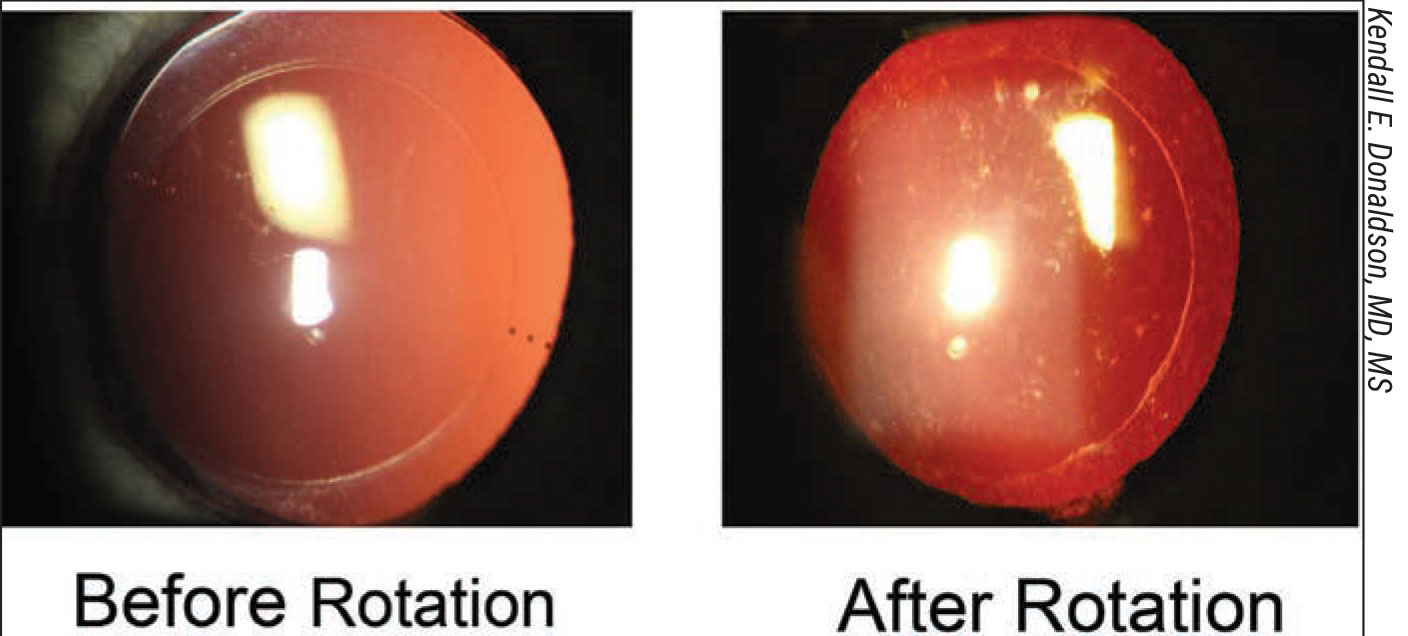
Figure 2. Significant residual astigmatism can seem like a devastating result for a postop patient who has paid a premium price for premium vision. (Click image to enlarge.) |
Dr. Donaldson notes that patients with low amounts of astigmatism are good candidates for almost any type of follow-up procedure. However, she points out that significant residual astigmatism can seem like a devastating result for a postop patient who has paid a premium price for premium vision. (See Figure 2, above.) “It’s important to zero in on the causes of residual astigmatism,” she says. “Surgically induced astigmatism can be related to poor preop measurements, poor calculations, posterior corneal irregularities that weren’t detected by keratometry, IOL rotation or poor IOL placement. Other factors could be related to the implantation of a wrong lens, which, of course, may also have resulted from poor measurements and inaccurate calculations. Additional considerations in this area: Could a rotational error of a toric IOL be a factor, either in multifocal or monofocal situations?”
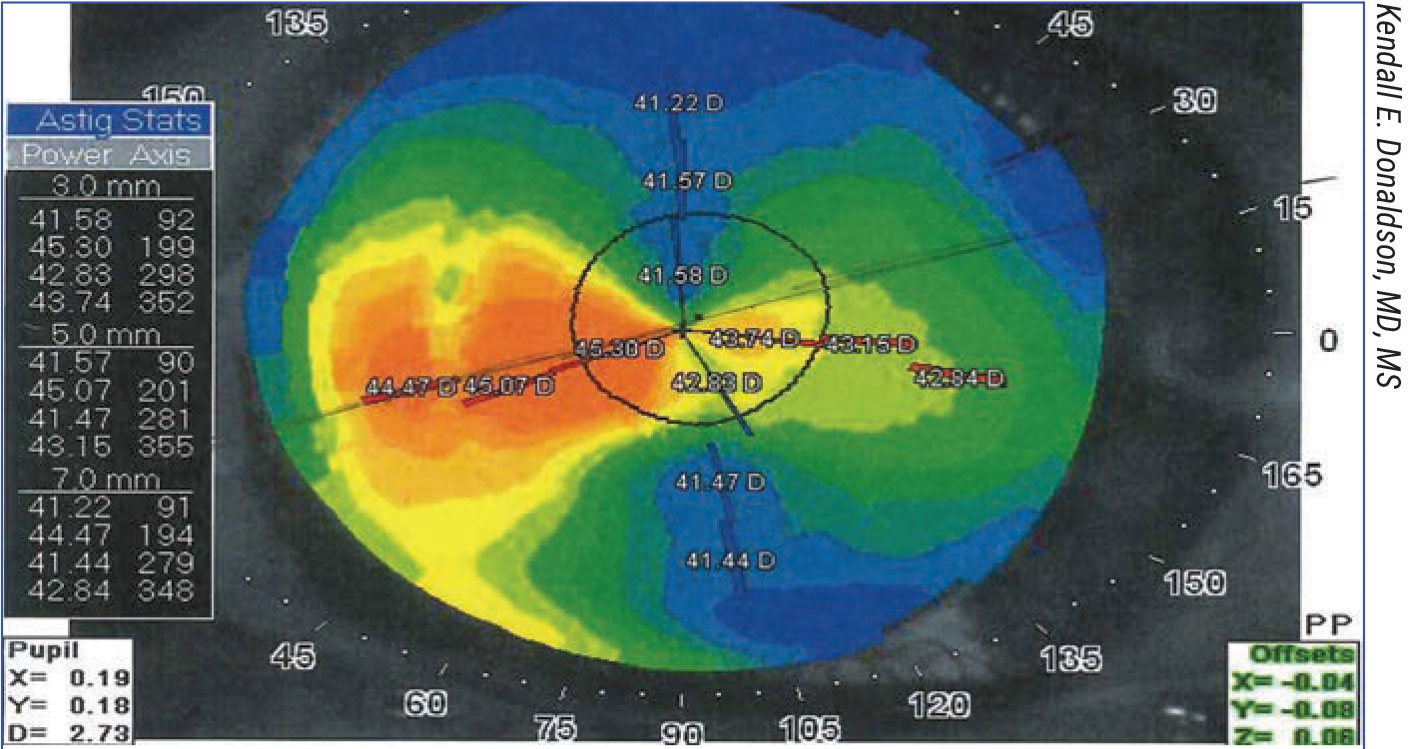
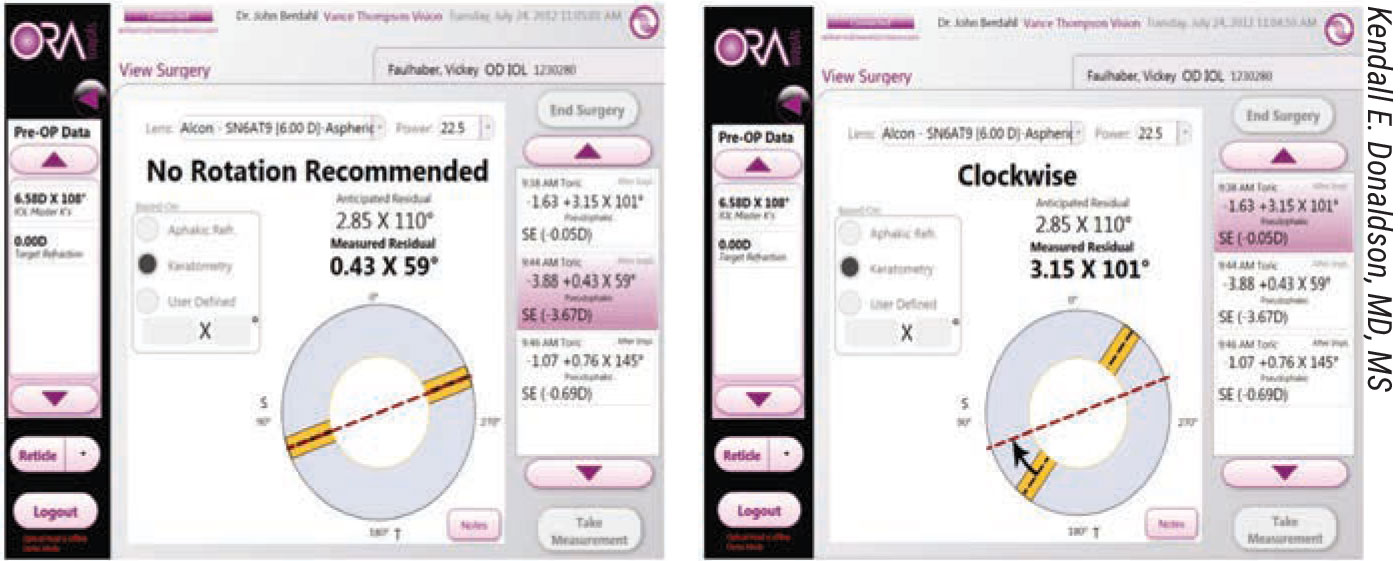
By pinpointing sources of postop astigmatic surprise, Dr. Donaldson continues, you can sometimes address causative factors with more precision than you might have been able to—for one reason or another—when planning the surgery. “As we know, specific technologies and formulas can be used to turn things around for these patients,” she says. “Formulas that can reveal the need for postop correction and alignment include Astigmatismfix.com and the Barrett Rx Formula [ascrs.org/tools/barrett-rx-formula].” She adds that Optiwave Refractive Analysis aberrometry (ORA, Alcon) and iTrace Visual Analyzer (Tracey Technologies, Houston, Texas), another wavefront aberrometer, can help guide alignment and realignment of a toric IOL—or even a non-toric IOL, such as an accommodating lens, in some cases.2 (See Figure 3 below.)
 |
| Figure 3. Intraoperative aberrometry can help determine if an IOL needs to be rotated. (Click image to enlarge.) |
In postop cases requiring an IOL rotation or adjustment, intraoperative aberrometers use Fourier calculations to determine the real-time readings of sphere, cylinder, axis, refractive error and IOL power.3 (See figure 4 below for an example of a successful postop rotation.) “Don’t forget that we can also use this technology during the initial surgery to make final selections of toric IOL powers and refine an IOL’s alignment, reducing the incidence of residual astigmatism,” she adds.
 |
|
Figure 4. Postop rotation of torics, made possible by today’s technology, can turn things around for some unhappy patients. |
A Systematic Approach
Tal Raviv, MD, founder and medical director of the Eye Center of New York in New York City, has organized a systematic approach to treating and preventing patient unhappiness after premium cataract surgery. “We’re focused on what we see as the top reasons for dissatisfaction, even among patients whose postop UCVA is 20/20,” says Dr. Raviv, who’s also an associate clinical professor of ophthalmology at Icahn School of Medicine at Mount Sinai. The top reasons for dissatisfaction that he cites include the following:
- glare, halos, starbursts;
- not enough near vision;
- poor distance vision and/or quality of vision; and
- generic IOL problems, such as negative dysphotopsias and dry eye.
Dr. Raviv says he responds to these forms of patient unhappiness with the following types of interventions:
- Non-surgical. His objectives include optimizing the ocular surface (with drops, dry-eye procedures and superficial keratectomy), performing a YAG capsulotomy, actively monitoring the patient and offering glasses or contact lenses.
- Surgical. The goal here, in the face of demonstrated need, is to provide PRK or LASIK, rotate IOLs and perform IOL exchanges that may involve monofocals, extended depth of focus lenses or multifocals. Rarely, he says, he needs to provide a piggyback IOL or recenter an IOL via a lasso suture.
- Refer for retinal surgery. These referrals could be for a pars plana vitrectomy with membrane peel for an epiretinal membrane or a PPV for floaters.
Another approach to postop unhappiness that Dr. Raviv will sometimes take is to defer possible follow-up treatment until after he implants an IOL in the unhappy patient’s second eye. He uses alternative IOLs in some cases. “I don’t automatically double down on the same technology for the second eye,” he says. “Many times, the second-eye surgery can compensate for the perceived deficiency of the first surgery. If that doesn’t prove to be the case, then an IOL exchange can be carried out.”
To ensure consistent delivery of care, Dr. Raviv follows what he calls the “Raviv Getting to Happy Post-IOL Algorithm.” (For a copy of the algorithm that you can use in your practice, see below.) The algorithm, informed by Dr. Raviv’s surgical experience, maps out responses to a variety of premium IOL postop challenges.
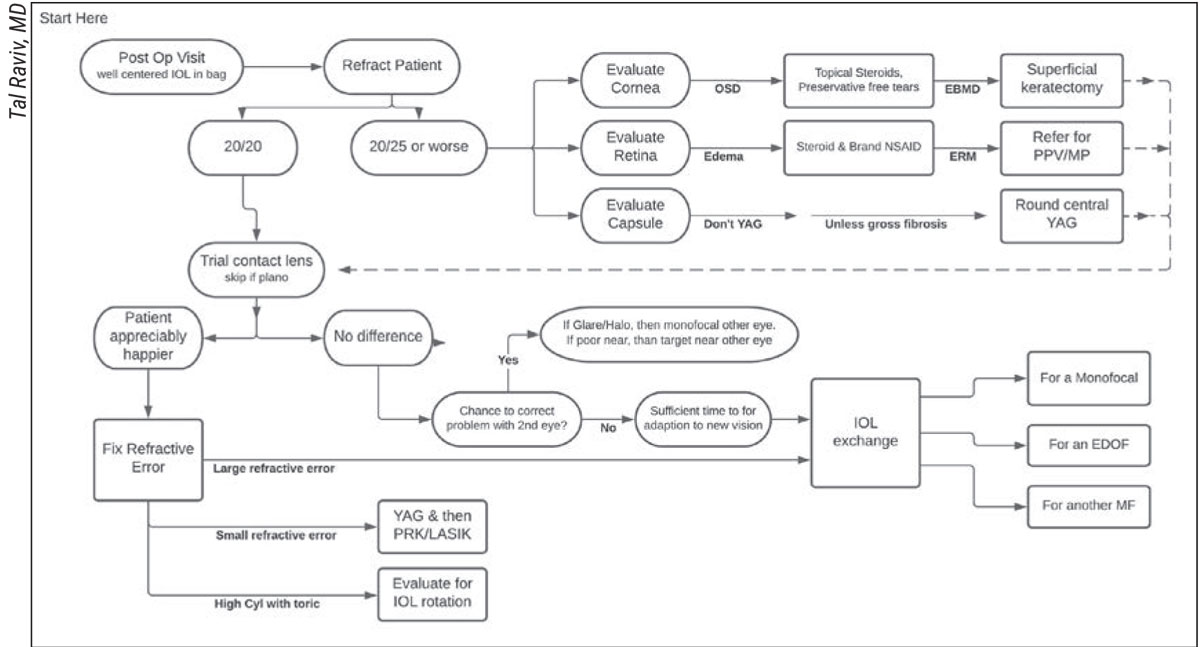 |
| Click image to enlarge. |
Considering Follow-up Surgery
Dr. Donaldson recommends the following strategies when deciding whether to offer follow-up surgery to unhappy premium IOL patients. “First, determine if the patient can tolerate waiting to see if his or her vision improves,” he says. “If not, exhaust less-invasive options and potentially seek a consultation with a colleague, when appropriate. If you become convinced a second surgery on the same eye is necessary, present a clear plan to the patient and make sure the patient understands your plan 100 percent, including the timing and possible outcomes of the intervention.” The next question is when to do the follow-up surgery. Generally, according to Dr. Donaldson, the following considerations should apply:
- Perform follow-up surgery sooner if a toric IOL is clearly off axis and needs to be repositioned, or if you find you’ve created an identifiable error in your original measurements that has led to an incorrect power calculation.
- Delay surgery (as long as it seems prudent for each patient), if:
– the patient has a small refractive error and may still neuroadapt; and
– the patient wants to wait. “I recommend three months before enhancing the postop patient who has a history of LASIK surgery, to avoid the suction effect on the cataract surgery wound,” says Dr. Donaldson. “A three-month wait is also best for a patient with a history of RK, due to postoperative refractive shifts.”
When debating which surgical modality to use on an unhappy postop premium IOL patient, Dr. Donaldson recommends avoiding laser vision correction if ocular surface disease has significantly contributed to the patient’s dissatisfaction. “I’d choose a repeat of intraocular surgery for these patients, when possible,” she adds. “In some cases, laser vision correction risks making the patient’s negative experience worse, even if you’ve moved them fairly far along on a diagnostic and treatment regimen for the dry eye. In patients without dry eye, laser vision correction is a great option for correction of residual refractive error. For correction of astigmatism, use the tools and formulas I mentioned earlier. If the need for correction is significant enough, I would, on a case-by-case basis, consider doing a lens exchange.”
Dr. Donaldson emphasizes that the overriding priority when providing premium cataract surgery should always be effective communication with patients. “Take the time to get to know your patient,” she says. “Set accurate expectations before surgery. Discuss the potential need for enhancements before surgery. Remember that insufficient or outright lack of treatment of residual refractive error is the number one reason for dissatisfaction among our patients after these types of procedures. I recommend taking every measure to correct errors resulting from the initial procedure. We have many options we can use to improve disappointing postop outcomes. Every step in the process is crucial to ensuring that we achieve our very best for the patient, starting long before surgery with accurate measurements, and effective management of patients to ensure that their expectations are realistic.”
 |
|
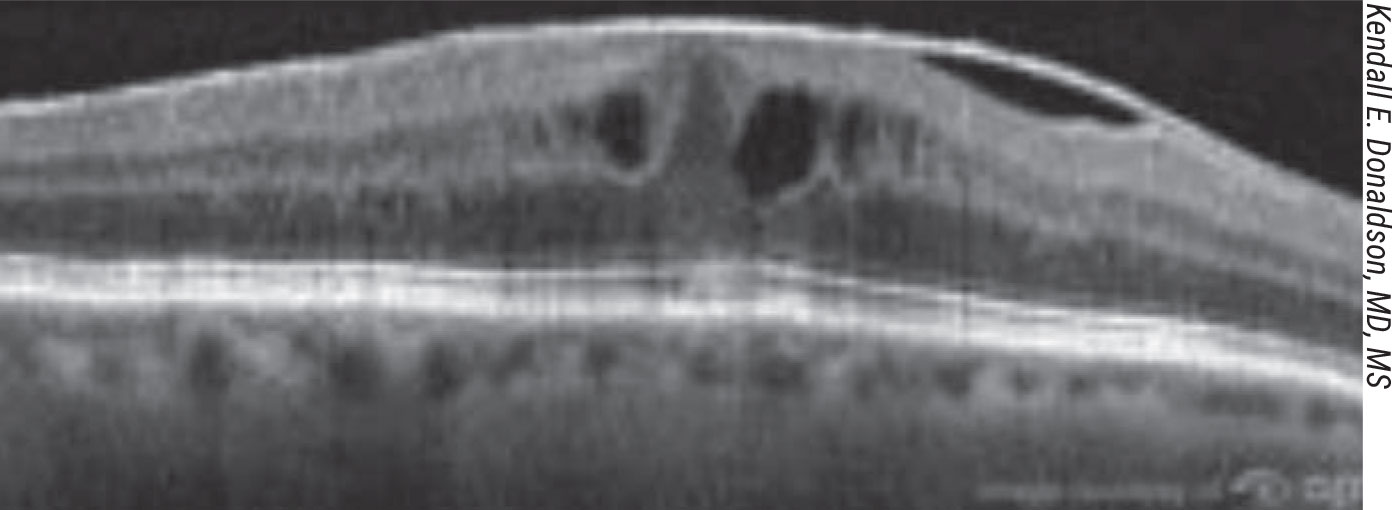
Figure 5. Many surgeons planning premium IOL surgery now rely on preop OCT scans to rule out retinal disorders. |
Eye on Refractive Enhancement
Zaina Al-Mohtaseb, MD, an associate professor and the associate residency director of the Cullen Eye Institute of the Baylor College of Medicine, discusses refractive enhancements when following up on unhappy premium IOL patients.
“Cataract surgery has become a refractive procedure,” she says. “High patient expectations and new lens technologies require correction of spherical error, astigmatic error and, in some cases, presbyopia.”
One of Dr. Al-Mohtaseb’s most important goals before even considering a refractive enhancement is to optimize the ocular surface. “Pre-existing dry eye is asymptomatic in many patients and it worsens after cataract surgery,” she says. “Besides increased dryness, the patient experiences decreased visual acuity and contrast sensitivity. That’s why diagnosing and treating any sign of ocular surface disease before cataract surgery is critical to achieving optimal surgical outcomes.”
She notes that the disease can negatively affect topography and biometry and, ultimately, surgical outcomes. “These negative effects decrease goblet cell density, tear breakup time and corneal sensitivity,” she says. “The end result is decreased quality of vision, fluctuating vision and decreased refractive outcomes.”4
Before determining if a post-cataract surgery patient is a refractive surgery candidate, Dr. Al-Mohtaseb waits on IOL stabilization and resolution of postop corneal edema. “The rate of refractive stabilization is proportional to incision size and may take longer in patients with prior keratorefractive surgery, such as radial keratotomy,” she points out. “We also want to make sure that the patient has enough tissue for a refractive enhancement and that we’ve considered all alternative treatment options.”
Finally, she says, she rules out other causes of patient dissatisfaction besides the premium IOLs, such as PCO or retinal pathology. In cases of residual astigmatism, Dr. Al-Mohtaseb says that:
- toric IOL repositioning is best performed in the early postop period;
- limbal relaxing incisions are effective in treating low amounts of residual astigmatism, especially in patients whose spherical equivalent is plano; and
- IOL-based surgery is best in the early postop period for poor corneal laser refractive candidates, high refractive errors and hyperopic errors.
“Furthermore,” she says, “lens-based enhancements appear superior for treating hyperopic errors because corneal-based hyperopic corrections require larger treatment zones, are less accurate and may regress over time. IOL exchange is indicated for correcting significant residual refractive error as well as IOL dislocation, malposition and multifocal IOL dissatisfaction.”
She adds: “Early exchange via the original wound is also ideal to avoid complications due to late capsular bag fibrosis. Late removal of an IOL may require cutting the IOL haptics or viscodissection to free the haptics and remove the IOL as one piece. Wound enlargement can also cause or worsen astigmatism after IOL exchange.” (For an in-depth look at IOL exchange, see this month’s cover story.)
New Kind of Partnership
Some surgeons say prevention of premium IOL surgery disappointment creates the need for a new kind of partnership between them and their patients. What’s envisioned, and practiced by some surgeons, is a relationship based on shared planning, rather than one that’s limited to boundaries imposed by informed consent and risk management. A successful, communicative relationship can provide the best means for identifying patients who aren’t good candidates for premium IOL surgery, these surgeons argue.
“Refractive cataract surgery is a transformational journey patients take with their surgeons,” says Dr. Raviv. “It’s the art and science of planning a customized visual solution, executing it perfectly and enhancing it as needed—and enhancing it is the critical part—during the postoperative period.”
Why, he asks, do premium IOLs represent less than 10 percent of the IOL market, even after 20 years into the development of high-technology lenses? “Today’s sixth- and seventh-generation PC-IOLs are more forgiving, have less photic effects and provide excellent ranges of vision,” he says. “We should be using a lot more of these. There are practices in the United States, successful refractive practices, that use these lenses on 40 to 50 percent or more of their patients. We certainly use a lot of them in my practice. But the reality is that if you have a budding refractive cataract practice, one unhappy multifocal IOL patient can really deflate your penchant for putting one in. So I posit that a refractive cataract surgeon have specific tools and techniques at the ready and know how to use them to treat unhappy multifocal IOL patients.”
Among the essential tools, he continues, is a contact lens trial set that includes torics. The contact lenses, available in many small steps away from plano, are superior to a manifest refraction and glasses when it comes to confirming the precise correction that will maximally satisfy an unhappy postop premium IOL patient, he says. “You also need the skill to perform IOL exchanges, and you need to have access to and the skilled ability to use an excimer laser for PRK, at the least. If you don’t offer these, you need to partner with someone in your practice or elsewhere who does.” He adds that you also need to establish a payment plan that frees patients of any obligations to shell out more cash for postop services that may be needed.
Dr. Raviv says managing patient expectations is essential for offering premium IOL services. “Add these seven words to your electronic health records—‘Discussed photic phenom, LVC, IOL exchange, glasses’—and briefly review each of these possibilities with every prospective multifocal IOL patient,” he says. “I tell my patients, ‘I’m not just going to correct the optical clarity of your eye. I’m also going to clear the focus of your eye. To accomplish that, we may also need to do a touch-up—if you heal out of focus, for example.’”
Under the terms of the payment agreement that waives additional fees, he explains the possible need for follow-up laser vision correction, a possible IOL exchange and, occasionally, the need to wear glasses for near vision. These situations crop up “less than 5 percent of the time, but this is something patients need to know,” he adds. “It’s critical because some patients say, ‘I don’t want another surgery.’ If they have absolute zero tolerance for a second procedure, then they’re really not candidates for a multifocal lens, in my book.”
Meanwhile, part of establishing realistic patient expectations means customizing patient education, providing your own brochures and video content to replace industry materials that make some information “a little too rosy,” according to Dr. Raviv. He discusses the possibility and likelihood of unwanted visual symptoms that are specific to each brand of IOL. These symptoms may include glare, halos, starbursts, occasional decreased BCVA, blurry near vision and refractive errors.
Identifying Pre-Existing Conditions
Some surgeons are finding they can improve outcomes by increasing their testing and screening efforts before surgery. Many now rely on preop OCT scans to screen for retinal disorders and preop topography to help detect ocular surface disease, corneal dystrophies and degenerations.
“As we institute treatment (before surgery), we track patients’ progress, and we have found tear osmolarity (TearLab Osmolarity System) to be a very helpful tool in doing this when used in conjunction with a thorough slit lamp exam and symptom assessment,” says Dr. Donaldson. “We’ve always used the OSDI (Ocular Surface Disease Index) because, of course, we want to know how the patient is feeling.” Another helpful screening tool is Inflammadry (Quidel), which aids in detection of inflammation that may need to be treated preoperatively to ensure more accurate preop measurements and a better visual outcome.
Hyperosmolarity is also associated with variability in K measurements, a situation that requires increased diagnostic vigilance when evaluating patients for premium IOL surgery.5 “If the patient’s topography is less than optimal, we determine if the tear film needs to be addressed,” says Dr. Donaldson. “If necessary, we postpone surgery and reassess the patient at a later date. I recommend that you not operate until you’re certain all symptoms are controlled. Measure before any eye drops are administered and repeat on eyes with unusual and inconsistent findings.
When Dysphotopsias Occur Dr. Donaldson recommends you consider the following treatment strategies for dysphotopsias:
|
“If we determine the postop error has resulted from preop measurements, we need to determine if it was our fault, possibly based a technician’s error, or perhaps an instrument error,” Dr. Donaldson adds, saying that she typically obtains keratometry readings on several devices and compares her findings to identify potential inconsistencies. She’ll also rely on a select few technicians for this testing to ensure more consistency.
One other important issue is a patient’s history of having LASIK surgery.
“We know that patients with a history of LASIK surgery have already lost some contrast sensitivity, so we need to be mindful of that when deciding if a patient is a good candidate for premium lens technology,” Dr. Donaldson says.
Traits of Challenge, Togetherness
Patient personality has also emerged as a consideration in premium IOL surgery. In 2020, a study found that multifocal IOLs helped ensure better postop visual acuity, but that some patients were also unhappy with their outcomes.6 Patients with a dominant personality trait of neuroticism were the least happy with their postop outcomes, the research found. Conscientious and agreeable patients were the most satisfied with their postop outcomes. The study suggested that a preop psychological exam and a careful surgical selection process may be in order for patients with neurotic personality traits. Dr. Donaldson also emphasizes always ensuring that you keep patient expectations realistic. “Offer available options but don’t promise perfect outcomes,” she adds.
Above all, according to Dr. Raviv, the right kind of doctor-patient relationship must be maintained to ensure success for all. “To take our patients through this journey, we must offer empathy, availability and compassion,” he says. “Patients need to know that we’re there for them—and committed to taking every step with them that’s needed."
Dr. Donaldson discloses financial relationships with Alcon, Johnson & Johnson Vision and Bausch + Lomb. Dr. Raviv reports financial relationships with Cassini Technologies, Johnson & Johnson Vision, Ocular Therapeutix and Zeiss. Dr. Al-Mohtaseb reports financial relationships with Alcon, Bausch + Lomb, Johnson & Johnson Vision, Ocular Therapeutix, Zeiss, CorneaGen and Allergan.
1. Gibbons A, Ali TK, Waren DP, Donaldson KE. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol 2016;10:1965-1970.
2. Page TP. Intraoperative wavefront aberrometery to determine planar endpoint for the repositioning of vaulted accommodative IOLs. J Refract Surg 2021:4:47:542-546.
3. Sarver EJ, Van Heugten TY, Padrick TD, et al. Astigmatic refraction using peaks of the interferogram Fourier transform for a Talbot Moire’ interferometer. J Refract Surg 2007:23:972-977.
4. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract patients’ Ocular surface (PHACO) study: The effect of dry eye. Clin Ophthalmol 2017;11:1423-1430.
5. Epitropoloulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg 2015;41:1672-1677.
6. Rudelevicius P, Lekaviciene R, Auffarth GU, et al. Relations between patient personality and patients’ dissatisfaction after multifocal intraocular lens implantation: Clinical study based on the five factor inventory personality evaluaton. Eye (Lond) 2020;4:717-7245.