The creation of a continuous circular capsulorhexis is key to any cataract surgery, and although surgeons can master this technique, there are some patient presentations that make it more tricky. White cataracts are one such situation. However, not all white cataracts are created equal, so a thorough understanding of the etiology will influence how to proceed with the surgery. We spoke with some experienced cataract surgeons who shared tips on techniques and tools that could make removal of white cataracts go more smoothly.
Approaching a White Cataract
White cataracts are often age-related and develop due to delayed treatment. They can also be caused by trauma to the eye. Studies have found traumatic white cataracts can contribute to the dysfunction of the epithelium, therefore leading to an increased risk of capsular breaks during surgery.1
“The term white cataract by name simply describes what it looks like,” says Richard Davidson, MD, a professor of ophthalmology at the University of Colorado Sue Anschutz-Rodgers Eye Center. “It’s a very dense lens inside the eye. It could be from a regular age-related cataract becoming too mature over time and therefore becoming more dense. It could be from trauma, prior surgery such as a retinal detachment repair or an injection that accidentally broke the lens capsule—all of those things can lead to white cataracts.”
The approach will be a little bit different based on the etiology of the cataract. “You must determine the etiology and properly identify it,” says Marjan Farid, MD, the director of cornea, cataract and refractive surgery at the University of California - Irvine School of Medicine. “Ask yourself: Is this a hypermature and centrally dense cataract that’s been around a long time? These cataracts appear white and have a significant cortical component and centrally they may be very mature and dense.
“Or is it a young cataract that developed after a trauma?” Dr. Farid continues. “If there was some kind of recent trauma to the eye, those cataracts can turn white very quickly, but those will often be very soft with milky, liquified protein built up within the capsule, forming an intumescent cataract. As the lens doesn’t like to be touched, even subtle trauma to the eye or another ocular surgery can cause a rapid whitening of the cataract.”
A significant amount of pre-surgical planning is necessary.
“The first thing you want to do is perform a complete eye exam and you really want to get a feel for what caused this cataract and what the vision potential is for the eye,” says Dr. Davidson. “Does the eye have the ability to see? Sometimes that involves doing an ultrasound to see if the retina is detached and checking old records to see what the previous vision was just to try and figure out what was their best vision previously, and is there a chance of getting that vision back again.”
Dr. Davidson says the surgery planning process should include a conversation with the patient. “I explain that this isn’t a routine case and there’s likely going to be a longer surgery, it’s going to be something that’s a little bit more complicated, and there’s a chance that we might have to get a retina specialist involved,” he says.
Dr. Farid also counsels her patients and tempers their expectations. “Anytime we have one of these very complex cataracts, especially if it’s trauma related, I make sure to tell patients that we’re going to do our best to remove their cataract safely, however, due to the uncertainty of capsule stability they may require a subsequent surgery,” she says.
“Make sure that you’ve explained to the patient that this isn’t what their next-door neighbor or family member had where they’re in and out in 10 minutes,” adds Dr. Davidson. “It could be 10 minutes, but it could be an hour, so you want to make sure that they understand that the chances of complications are higher. You want to document that conversation because that’s really important.”
Discussing IOL options takes some additional consideration. “IOL offerings depend on what you think the vision potential is for the eye,” says Dr. Davidson. “Believe it or not, when I was a resident white cataracts usually meant poor vision potential—nowadays, there’s some patients coming in with white cataracts who actually want multifocal lenses or other ‘premium’ options. They have good vision potential in the eye and you really have to sit and counsel them carefully, and sometimes it’s hard to do because you don’t know exactly what that vision is going to be.”
Dr. Farid avoids multifocals if the cataract is trauma related and she’s worried about zonular stability. “I’ll also avoid toric lenses due to concerns about lining up the lens appropriately with the visual axis,” she says.
 |
|
Experts say staining the capsule with trypan blue is essential for visualization with white cataracts and will help surgeons through the capsulorhexis step. |
Managing the Surgery
Now that the surgeon is ready to go to the OR, the available resources also play a role in how they proceed, adds Dr. Davidson. “Not every surgeon has a femtosecond laser or a Zepto device. You may be operating in a place that has just you and your hands and some basic instruments,” he says.
No matter what’s available, achieving a complete capsulotomy matters. “Complications can happen anywhere along the way and it starts with the capsulotomy. If you get a bad capsulotomy the case automatically becomes more difficult for yourself,” Dr. Davidson says.
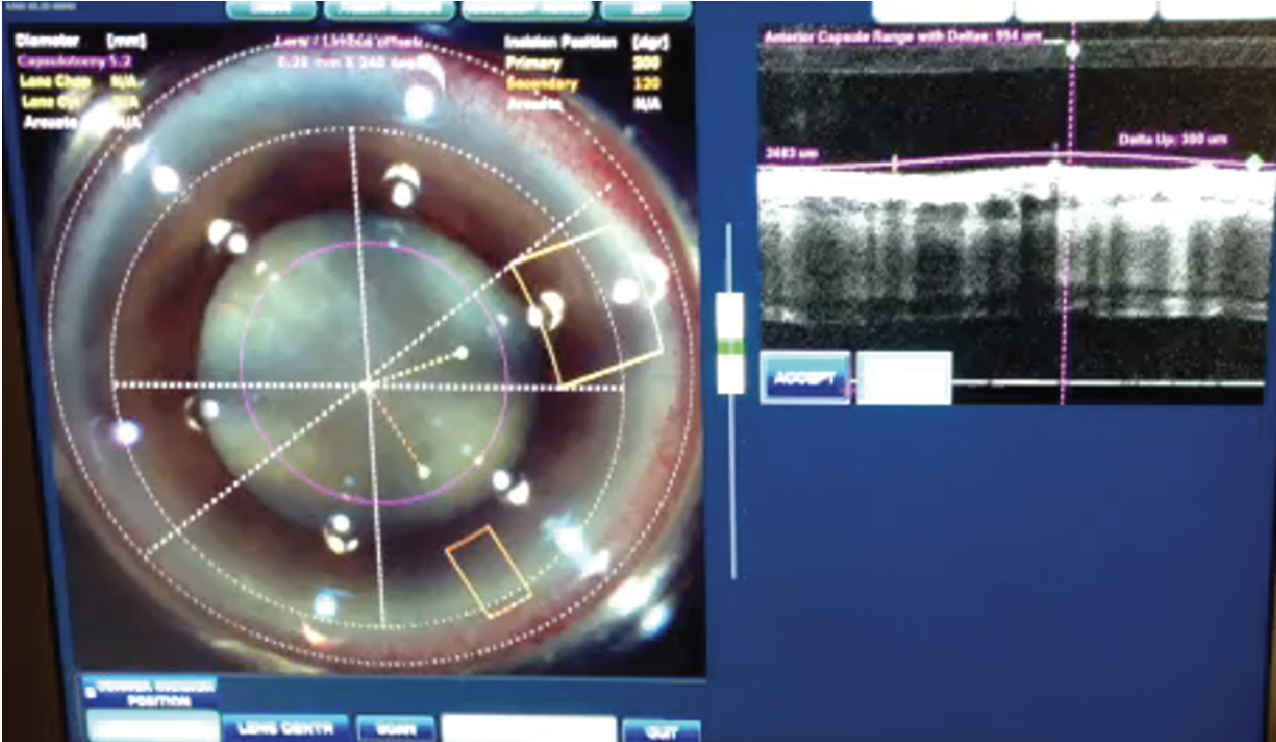
“If it’s a white cataract, the longer it takes can be a little bit of a risk,” he continues. “A femtosecond laser can be helpful to make the capsulotomy. From a capsulotomy standpoint, I do like the femtosecond laser. The problem is that some femtosecond lasers are faster than others. There are lasers that can do a capsulotomy in one second, and there are some that take four, six, seven seconds.”
Dr. Farid says femto can help reduce one of the most notorious complications with white cataracts: the Argentinian flag sign. The Argentinian flag sign was named by Daniel Mario Perrone, MD, upon observation of a radial anterior capsule tear after it had been stained with trypan blue, giving it the appearance of blue and white stripes.2
“It’s nice to use an ultra-fast laser because you potentially avoid the risk of capsular radialization and an Argentinian flag sign, which a manual capsulotomy can cause,” she says. “If approaching the rhexis manually, you want to stain the capsule with trypan blue for better visualization. If it’s a hyper-mature cataract and there’s a lot of pressurized liquification of the cortical material within, then the original incision into the capsule can create a rapid radialization. To avoid this, you can go in with a needle on a syringe and as you enter into the capsule, you also withdraw the fluid to deflate that pressure rapidly and to prevent the radialization of the capsule. Once you deflate that capsular bag, then you can carry on with your capsulotomy.”
 |
|
Some surgeons favor using a femtosecond laser when presented with a white cataract due to its speed and accuracy in creating a capsulotomy. |
Recovery from the Argentinian flag sign is possible, continues Dr. Farid. “If a capsular radialization is encountered, usually the tear doesn’t go completely around the lens and therefore a gentle approach to removing the nuclear material is imperative,” she says. “A gentle hydrodissection, minimizing any stress on the remaining capsule is critical. Chop techniques become very important. You want to direct all your forces centrally rather than outwardly where you can put stress on the zonules or put more extension on that radialization. If you can keep your forces central and gently bring out those nuclear segments into the anterior chamber and away from that capsular bag, then you can successfully complete a case of an Argentinian flag and even successfully put a three-piece lens into the sulcus.”
Technologies continue to evolve to assist with the capsulotomy step of cataract surgery. Dr. Davidson says the Zepto device (Centricity), which creates a ‘precision pulse capsulotomy’ (PPC) in only 4 milliseconds, can be a helpful tool. “That can be really helpful in white cataracts specifically because the problem with white cataracts is that often the capsule is under pressure from fluid beneath the capsule, and the capsulotomy can be very challenging,” he says. “With devices like Zepto, which deliver pretty much instantaneous bursts of energy, you can get a nice capsulotomy very quickly and in a safe manner.”
One retrospective study,3 which was authored by co-founder/consultants for Centricity, compared manual capsulorhexis in 15 cases with white cataract to 20 cases of PPC with white cataract. It showed PPC created a complete capsulotomy without tags or tears in all 20 cases. It also reduced the use of trypan blue and OVD, resulting in shorter overall surgery time.
|
|
The last thing a surgeon wants to see when removing a white cataract is an Argentinian Flag sign. Not to worry, experts say the surgery can be successfully recovered when this happens. |
Challenges to Expect
Depending on how dense the lens is, lens disassembly can be challenging. “These lenses tend to be very dense, very fibrotic, and you have to learn how to chop a lens and be very good about breaking up this fibrotic-type lens,” says Dr. Davidson.
Both Dr. Farid and Dr. Davidson reference the Zeiss miLoop. “It’s a nitinol ring that goes around the lens that then cuts the lens into two or more pieces,” Dr. Davidson says. “It saves a lot of energy or phaco time when you’re trying to get these lenses out or disassembled because it cuts through and you don’t have to exert as much force or use as much phaco to get the lens broken into smaller pieces.”
Another thing to keep in mind is that sometimes these lenses are so dense, phaco isn’t always the best option, he continues. “Sometimes it’s better to do an extracapsular cataract extraction either through MSICS or traditional extracapsular cataract extraction,” Dr. Davidson says. “Sometimes in the right hands, that’s a better procedure than trying to phaco and use a lot of phaco energy. In these cases you really have to think about your own experience, what you’re most comfortable doing and what works best for you because different surgeons are going to have different strengths.”
Dr. Farid emphasizes the importance of keeping any forces central. “Directing the manipulative forces central will minimize zonular stress, especially if it’s a trauma-related white cataract, is important for stability of the capsule and zonules,” she says.
Zonulopathy is something to be on the lookout for in white cataracts.
“One problem when you’re taking out these lenses, is that they can be super mobile in the capsular bag and you can’t always tell if it’s just mobile or if there’s actually zonulopathy, too,” Dr. Davidson says. “I personally always assume there’s zonulopathy and try to get the lens out of the bag as quickly as possible and work with it out of the bag, assuming the patient has a deep enough anterior chamber. You just don’t know what these zonules are like and until you have more of the cataract out and until you can see better, you can’t tell very well if there’s zonulopathy.
“Once you have more of the lens out it’s nice to be able to put a capsular tension ring in if you need to,” he continues. “That’s really where having experience helps because you can see the subtle things that a more novice surgeon may not be able to notice, such as the way the capsule moves, that may suggest that a zonulopathy is present.”
At this stage, capsule stability can influence the IOL selection. “In some cases you may feel more comfortable putting in a three-piece lens,” Dr. Davidson says. “If you’re not sure about whether there’s a hole in the capsule, sometimes people will put a lens in the sulcus and capture the optic. It depends on the integrity of your capsule and how you assess the zonules. We always want to take a step back for a second once the cataract’s out and really get a good look. When you put viscoelastic in you can kind of get a feel for how the capsule is holding up—is it collapsing on itself or not—and then make a decision. You don’t know exactly what you’re going to get until you put the lens in and until the patient heals a bit.”
Postop Care
Oftentimes, these patients need more aggressive steroids or nonsteroidals afterwards. “Depending on the length of the surgery and the amount of phacoemulsification energy used, I do put patients on steroids, nonsteroidal anti-inflammatories and antibiotics,” says Dr. Farid. “If there’s more inflammation in the postop period, we might extend their postoperative drop regimen.”
“Certainly once you have the cataract out, you want to get a good look at the retina during the postop period and make sure everything looks good,” says Dr. Davidson.
Dr. Chayet is considered a pioneer in refractive and cataract surgery, and is the medical director of the Codet Vision Institute in Tijuana, Mexico. He is a clinical investigator for RxSight, LensGen and ForSight Vision6.
1. Okoye GS, Gurnani B. Traumatic cataract. StatPearls 2023 Jan (Online publication) Updated 2023 Aug 2. https://www.ncbi.nlm.nih.gov/books/NBK594251/
2. Perrone DM. Argentinean flag sign is the most common complication for intumescent cataracts. CAO Library Catalog. Accessed September 22, 2023. https://www.oftalmologos.org.ar/catalogo/items/show/5961.
3. Ifantides C, Sretavan D. Automated precision pulse capsulotomy vs manual capsulorhexis in white cataracts: Reduction in procedural time and resource utilization. J Cataract Refract Surg 2023;1:49:4:392-399.