It’s likely no physician entered the field of medicine for the business aspect. However, health-care professionals are increasingly expected to apply business acumen if they want to meet patient expectations and turn a profit, a task made more challenging by the structure of a health-care system that sets up roadblocks at every turn. Ophthalmologists are no stranger to the challenges and cataract surgeons are at particular risk as they perform the most prevalent procedure in the world, and also the most common among Medicare patients.
Medicare cuts are down 2 percent across the board in 2023, and cataract surgeons feel targeted for their own efficiencies. A recently published comparative study1 looked at the differences in day-of-surgery costs and net earnings between simple and complex cataract surgery and found the costs were $1,486.24 for simple and $2,205.83 for complex, a mean difference of $719.59. Yet, incremental reimbursement for complex cataract surgery was $231.01.
The consensus in the field is that cost-cutting has run its course. Providers have to try new things, whether it’s introducing new services and products to patients, or finding procedural efficiencies within their practice.
“Physicians have been dealing with this forever in their practices and they’re striving to be as efficient as possible while remaining compliant, and that’s no small feat,” says Laurie K. Brown, MBA, a senior consultant at BSM Consulting in Arizona. “New compliance regulations are being added every year, and they require time and energy to implement and monitor. Practices also must be as productive as possible to effectively absorb the cost of all these efforts in addition to rising practice expenses, so it’s definitely a continual challenge and people are looking for ways to become as efficient as possible.”
Nicole Fram, MD, managing partner of Advanced Vision Care and a clinical instructor of ophthalmology at the Stein Eye Institute, UCLA, says the declining reimbursement issue has two aspects. “One is having to see more patients to earn the same revenue, and the other is feeling undervalued,” she says. “Those two things can lead to burnout. I think that a lot of practices have tried to streamline to work smarter, not harder.”
Cataract surgeons have a few options to consider if they’re interested in additional patient-pay services that may offset declining reimbursements, however they have to present these delicately, without coming off in a bad light.
“From a financial perspective, it makes the most sense for surgeons to gain when patients gain,” says Daniel H. Chang, MD, a cataract and refractive surgeon at Empire Eye & Laser Center in Bakersfield, California. “My goal is to put patients’ medical needs first and my practice’s financial needs second. However, I’m also aware that if I can’t meet my practice’s financial needs, there will be no practice for me to meet any of my patients’ medical needs.”
 |
| Spending time on patient education about presbyopia-correcting lenses or dry-eye treatment can go a long way in their conversion rate. (Courtesy Getty Images) |
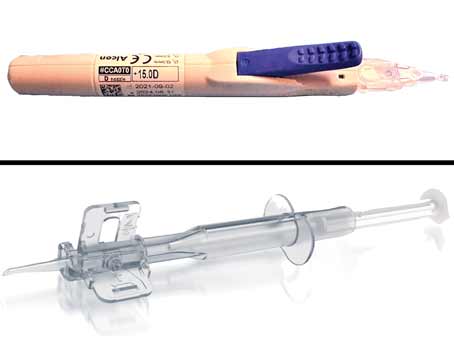
Premium IOLs
Among the first products they may begin offering to patients are premium IOLs.
Dr. Fram says the timing of these new technologies is a benefit to cataract surgeons. “Fortunately, innovation has kept up with the pace of declining reimbursements so that the extended-depth-of-focus lenses, the toric lens options and the trifocal options have been advanced to the point where they’re more tolerable, and they deliver on the expectation of the patient,” she says. “In the past, if we gave someone a multifocal they could see distance or near but they couldn’t see intermediate. Or if we put in an extended-depth-of-focus lens, they could see distance but they didn’t get their intermediate, and so the technology in the past wasn’t delivering, which made it very difficult to take that gamble on which patients to use this technology on. Now, you can offset some of the decreased reimbursements with more flexibility in the vision and presbyopia correction and at the same time, compensate for the declining valuation from insurance companies and Medicare on the value of cataract surgery.”
Dr. Chang says, when thinking about the correction of presbyopia, surgeons should consider economic values from a patient perspective and also from a health-care system perspective.
“Although there’s an upfront cost to the surgical correction of presbyopia, alternative treatments for presbyopia such as multifocal spectacles (bifocals, trifocals and PALs) can more than double the risk of tripping and falling, with one in three falls attributable to the use of these glasses,”2 he says. “In the U.S. alone, there were over 12 million fall injuries in 2017,3 and the treatment of these injuries cost the health-care system more than $9,000 per non-fatal fall.4
“Ultimately, from a patient safety, convenience and financial standpoint, it makes a lot of sense to treat presbyopia and astigmatism at the time of cataract surgery,” Dr. Chang continues. “Fall risk increases with age; and it’s common for typical cataract patients in their 60s and 70s to have experienced declines in their balance, dexterity and reaction time, thus leading to these increased risks. That’s a big deal.”
In order for patients to buy into this technology, it’s all in how you frame the conversation. “If a patient likes the idea of not wearing glasses, then we suggest the technology that will get them to that outcome,” says Dr. Fram. “It’s a conversation, a partnership—it’s not a sales pitch. That’s a big turnoff to patients and I don’t think it’s an effective way to really build a presbyopia correcting or refractive-cataract surgery practice.”
Spending time in the chair with the patient is important, continues Dr. Fram. “I spend a lot of time in the room and I show patients a schematic of the eye from [patient-education company] Rendia and explain how the different parts function,” she says. “Then we’ll show them simulations of what their vision would be like if we correct their astigmatism vs. if we don’t.”
Before leaving the room, Dr. Fram makes notes in the patient’s chart about which lens she recommends and the surgical plan, noting if there may be challenges during the surgery.
“When the biometry tech looks at their chart, they see which lens I had a conversation about and they reinforce and talk about only that lens with the patient,” says Dr. Fram. “If the patient says they don’t want to pay out of pocket, we schedule a telemedicine call to discuss.”
Dr. Fram tries to make these calls personally. “I see this as an important medical call,” she says. “I tell them I respect what they’re saying, but I want to ensure they understand what it means if they don’t go with that lens or don’t have any astigmatism correction, because sometimes they don’t understand or they hear their friend didn’t have to pay anything. If they still decide not to go with that premium IOL, I am comfortable going forward with a standard surgery because we had this conversation. It doesn’t happen often because our counseling is so strong.”
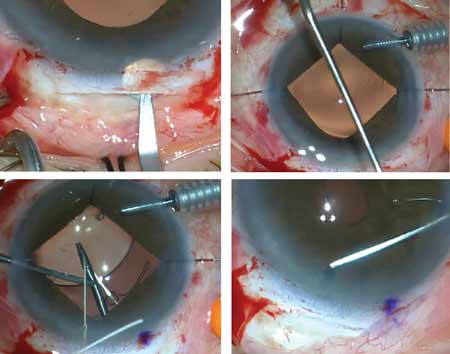
There are some caveats associated with offering these services, Dr. Fram points out. “If you’re getting into refractive cataract surgery and presbyopia correcting lenses, you need to know how to take them out and you need to know how to refine residual refractive errors,” she says.
“Some people put the lens in and if the patient is unhappy, they’re told it’s too dangerous to take out. Another scenario is if the capsule gets cloudy and the patient is upset, the surgeon lasers the capsule and then says it’s too dangerous to take the lens out,” says Dr. Fram. “You need experience with vitrectomy and different fixation techniques if things get complex.”
Surgeons must also understand the causes and treatments of residual astigmatism. “Whether it’s a small amount of myopia or a rotation of a toric lens, you need to know how to refine that either with LASIK or PRK, or exchanging the lens if you have a hyperopic outcome,” she continues. “Lastly, stay up to date with advanced IOL formulas. There are wonderful webinars on the ASCRS site that are ongoing. If you’re going to be in the game, you’ve got to stay current.”
Dr. Fram says the premium refractive option of lenses are delivering in a time of uncertainty for cataract surgeons. “It’s serendipitous that we have these technologies as reimbursements are going down,” she says. “It’s been a big boost to our practice. If we look at presbyopia-correcting options in our practice, we’re over 50 percent, and that’s happened in the last four or five years, especially with the addition of the light adjustable lens, which is great for the post-LASIK patient population.”
Dr. Fram does recognize that practicing in Los Angeles likely contributes to the higher-than-average adoption rate. Dr. Chang says the uptake nationwide hasn’t been as swift.
“Throughout the history of range of vision (presbyopia-correcting) and toric lenses, industry has assumed that the promise of financial reward will drive surgeon behavior,” he says. “There’s been an underlying assumption that declining insurance reimbursements for cataract surgery can be countered with patient balance billing to preserve or even increase profitability. Nevertheless, in spite of the promise of financial gain, so-called ‘premium lenses’ still represent only a small proportion of the cataract surgery market.”
Dr. Chang comes back to the importance of mindset. “As it turns out, our ability to charge for procedures that don’t just provide a convenience—and a lot of surgeons think about presbyopia and astigmatism correction simply as a convenience—but that can improve safety is certainly worth changing the way we think and approach the opportunity,” he says. “We should treat presbyopia and astigmatism not because it’s convenient or makes us money, we should do it because it’s the right thing for the patient.”
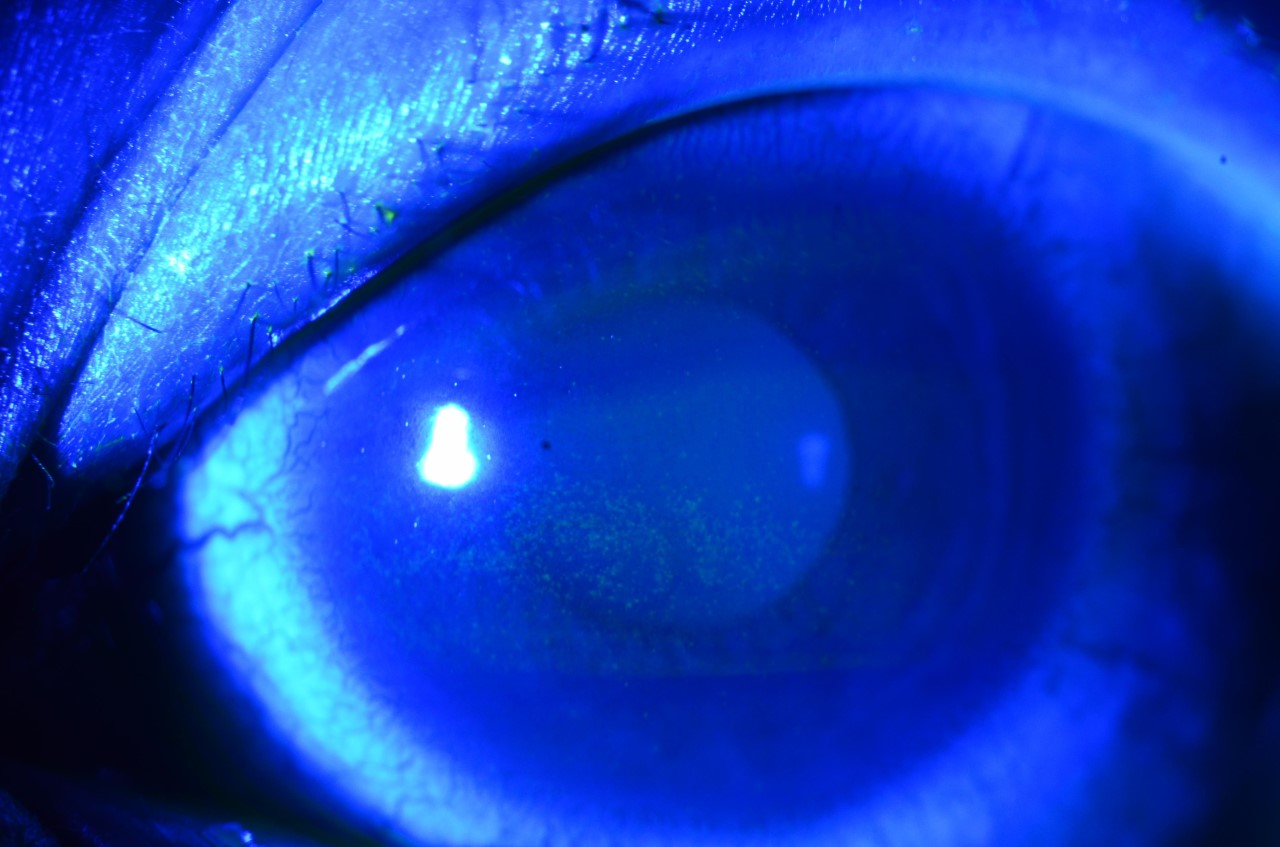 |
| Fluorescein staining can reveal dry-eye disease, which should be addressed prior to cataract surgery. Many surgeons have invested in adding dry-eye clinics to their practices as a way to add revenue. (Courtesy Christopher Rapuano, MD) |
Dry-Eye Treatment and Other Elective Services
“Elective services assist practices greatly to increase revenue,” says Ms. Brown. “Some practices have been very successful in treating dry eye before cataract surgery and expanding into cosmetic services. Fees still need to be reasonable and substantiated, but there’s definitely opportunity to be paid fair reimbursement for elective services.”
She’s noticed an increased interest in fundus photos among the cataract practice clients she’s worked with. “We’re seeing a lot of fundus photos as screening tests. There are compliance issues around that for Medicare patients and we’ve been helping clients understand compliance,” Ms. Brown says. “When you’re doing a test as a screening that’s a ‘sometimes-covered’ test when there’s a medical necessity, the advanced beneficiary notice (ABN) needs to be executed for Medicare patients (other payers may have other waivers). It’s important to set up protocols to support compliance. There are a lot of diagnostic tests like OCT, topography, etc., that are done in a cataract practice and sometimes they’re just blanketly done, when that could be more targeted for your premium-pay patients where you can actually recover revenue for work performed. Essentially, it’s less efficient to use the shotgun approach; Do you need that data 100 percent of the time, or do you just need it on patients who are candidates?”
As for dry-eye disease, addressing a patient’s ocular surface goes hand-in-hand with cataract surgery, and may even create more candidates for premium lenses.
“I think having a dry eye center of excellence in your practice is really important,” says Dr. Fram. “Dry eye is the low back pain of ophthalmology—if you treat it well and systematically, you can have a really thriving department.”
Michael A. Farbowitz, MD, who practices at Short Hills Ophthalmology in New Jersey, has seen firsthand how dry-eye screening and treatment have impacted his bottom line. They began screening every patient who walked through the door back in 2017 after investing in a LipiFlow (Johnson & Johnson).
“We screened all patients, whether they were coming in for checkups, cataract surgery or routine eye exams, and we picked up a lot of patients who unknowingly had meibomian gland atrophy,” Dr. Farbowitz says. “We were treating patients who weren’t even aware they had dry eye, and word got out and patients started seeking us out because treatments they had tried in the past were unsuccessful.”
Dr. Farbowitz sees dry-eye screening as an important role for ophthalmologists. “Our job isn’t only about removing their cataract to help them see better, but we’re obligated to pick up on things they don’t know about. That’s why we do glaucoma screenings. We pick up on things before they have symptoms and when it’s easier to treat. I’ve really embraced the preventative care model over the last six years or so and it’s borne fruit financially, but also in word of mouth.”
As with premium lenses, the conversation with the patient regarding dry eye is an education. “Almost two-thirds of patients who come in for cataract evaluation have dry eyes, and half of those patients don’t know they have it,” he says. “And we also know that biometry changes dramatically after an eye is treated with thermal pulsation, which influences the lens choice. So I tell the patient that there’s a chance their lens calculations will change or may be inaccurate if we don’t treat the dry eye ahead of time. I also explain that dry eye is a chronic disease and that cataract surgery may exacerbate it, therefore it’s better to treat beforehand.”
He sometimes uses an analogy with patients: “ ‘Before you drive a prize sports car across the country, you’re going to make sure the tires are filled and the fluids are topped off,’ ” says Dr. Farbowitz. “You don’t want to rush into anything.”
Dr. Farbowitz has also added OptiLight (Lumenis) to his practice, and he says this does add to the patient’s surgery timeline. “You do run the risk of losing a patient who wants their surgery sooner or at a specific time because the OptiLight treatments are spaced apart,” he says. “Patients can probably find another surgeon who isn’t going to treat their dry eye and can operate next week if that’s what they really want, but I think results matter and most patients get that.”
For dry-eye treatment, Dr. Farbowitz tackles the pricing with patients himself, as opposed to handing it off to a surgical coordinator. “It’s not as involved as explaining the pricing of premium lenses, and it actually turns out to be quicker if I handle it so the patient isn’t waiting to meet with the coordinator,” he says. “I lay it all out and tell them this is a procedure that isn’t covered by insurance and here’s how much it costs. I don’t apologize or get into justifications about why it’s that price. I’m just matter-of-fact about it.”
Initially, Dr. Farbowitz offered a discount on premium lenses if the patient had LipiFlow, but he put a stop to that. “I used to think charging for dry-eye treatments before surgery was going to cannibalize my premium lens conversion, but then it also felt like I was cheapening the value of the premium lens,” he says. “Patients are smart and they understand that cataract surgery is a one-shot deal.”
Treating dry eye has a greater return on investment than cataract surgery, he continues. “When you look at cataract surgery, you’ve got to leave your office and go to the surgical center, subject yourself to medical liability, back and neck strain, potentially stressful surgical experiences and unhappy patients, then you take into account the times you see the patient pre- and postop, and for a simple cataract you’re getting reimbursed maybe $500.
“A dry-eye treatment, whether it’s intense pulsed light or LipiFlow, that’s done in the office, and depending on what state you’re in, you can delegate these treatments to a technician or other providers in your office,” Dr. Farbowitz continues. “Dedicating a portion of your practice to dry eye is going to increase your surgical volume, your results will be better and you’ll have a better reputation in the community.”
The Business Perspective
As Dr. Fram said earlier: “Work smarter, not harder.” Evaluating the nuts and bolts of your business can be advantageous and could discover areas where money or time is being wasted.
An outside perspective can be beneficial, Ms. Brown explains. “We often go at it through a revenue cycle management assessment,” she says. “We collaborate with the team to look for opportunities to maximize processes and revenue while increasing their efficiencies wherever we can. Now is not the time for practices to leave any money on the table, or leave any wasted steps in their processes. They really can’t afford to do that. We also perform flow and efficiency operational assessments to maximize clinic productivity and the patient experience, as well as the staff and provider experience. We look at where their hurdles and frustrations are; we have open give-and-take discussions. During the assessments, we look at each step of processes, and the tools and the resources used and their effectiveness.”
Ms. Brown sees common issues in physicians’ offices. “Many people don’t have an organized way to work their accounts receivable or they have a process written down but there isn’t accountability,” she says. “This may be because they’re spending time doing something manually that could be automated, such as eligibility checking for example. The same occurs with the clinic flow. If we have a routine process of using standardized procedures which make a clinic click along and go very smoothly, then when you need that extra time for the unusual patient you have it, without throwing off your entire schedule.”
Standardized processes allow you to add more patients in the day and increase the productivity of the practice, Ms. Brown continues. “Often the tools and resources are in your practice already, maybe just not being used or maximized in the best way. Look at what you’re doing systematically, and remember, working to improve processes will give you more time in the day, which gives you an improved patient experience. When you can improve the practice flow and things are clicking along better, you can be much more effective.”
Dr. Chang (www.empireeyeandlaser.com) is a consultant to Allergan and Johnson & Johnson Vision. Dr. Farbowitz is a consultant for Lumenis. Dr. Fram reports no relevant disclosures.
1. Portney DS, Berkowitz ST, Garner DC, Qalieh A, Tiwari V, Friedman S, Patel S, Parikh R, Mian SI. Comparison of incremental costs and medicare reimbursement for simple vs complex cataract surgery using time-driven activity-based costing. JAMA Ophthalmol 2023 Mar 9:e230091. Epub ahead of print.
2. Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc 2002;50:11:1760-6.
3. James SL, et al. The global burden of falls: Global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 2020;26:Supp 1:i3-i11.
4. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res 2016;58:99-103.