The AMO Verisyse
A common theme with both phakic lenses approved in the United States is the importance of preop biometry.
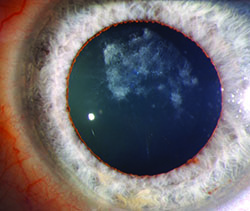
Jeffersonville, Ind., surgeon Asim Piracha says the first things surgeons should focus on are endothelial cell counts, anterior chamber depth and iris anatomy.
“The new FDA guidelines are strict regarding cell counts,” Dr. Piracha says. “The minimum density, based on patient age, is listed on the Verisyse product insert. You want to see a good, dense cell pattern with no guttata.
The second consideration is anterior chamber depth,” he continues. “For the Verisyse, you want at least 3.2 mm from the endothelium to the anterior lens capsule. If your device calculates anterior chamber depth and includes the epithelial surface, you have to subtract that corneal thickness amount from the measurement.”
The third factor to consider is the iris anatomy. “If the patient has a flat or concave iris, I feel better about implanting the lens,” Dr. Piracha says. “If, however, it’s convex, raised up anteriorly or has a little elevation to it, there’s more risk for posterior synechiae. You can evaluate the iris using a Pentacam or an OCT. Undesirable iris anatomy is more of an issue for hyperopes, however; you hardly ever see convexity in high myopes.”
Two unique aspects of the actual surgery are that the Verisyse, which is non-foldable, requires a relatively large incision and is fixated using a special iris enclavation technique that is as much art as it isscience. “You make an incision that’s a little bigger than 6 mm so you’re not squeezing the lens into the wound,” Dr. Piracha explains. “If you squeeze it in, you can inadvertently pop it in and ding the capsule. The sideport incisions are about 10 mm apart, which means they’re about 2 mm from the lateral edge of the main incision on each side. The key to creating the sideports is to point your blade toward the enclavation site. This is different from the way surgeons usually do it, which is to point the blade toward the pupillary center.”
The enclavation of the Verisyse, which roots it in place, involves using special claws on either side of the lens to grab a small piece of iris. “After inserting the lens I rotate it 90 degrees and enclavate the nasal haptic first, because it’s a tighter space,” Dr. Piracha explains. “There’s something of an art to enclavation. First, you grab the IOL. For this step I recommend using an Artisan/Verisyse forceps because it has a kind of platform to it that prevents the lens from flipping like a tiddlywink. Next, I use an enclavation needle on the iris with a motion similar to the rubbing motion you’d use to bunch up a piece of rug. If you’re enclavating at 3 and 9 o’clock, start a little superior with the needle then push it inferiorly. This causes a wrinkle in the iris that you then use to enclavate. As to how much iris to enclavate, taking too much will cause ovalization of the pupil, but taking just a little wisp can result in the lens being dislocated with any trauma. The ideal amount is probably about 1 mm; you want it just overlapping the claw port. As in the story of Goldilocks, the best amount is not too much and not too little.”
The Staar Visian ICL
As with the Verisyse, preop measurements are crucial to the success of Visian ICL implantation.
|
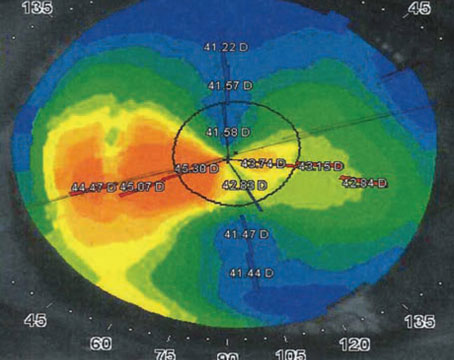
The problem with inaccurate sizing is it can lead to postoperative issues. “I like the space between the anterior crystalline lens capsule and the Visian ICL to be between 100 and 400 µm,” says Dr. Moshirfar. “If you undersize, the vault will be less, and the space between the lens and the ICL will be small, around 50 to 90 µm. If you oversize it, however, it creates a huge vault and, as a result, the space can be 700 to 1,000 µm. In this condition, the iris is pushed forward and the patient can go into a form of angle-closure glaucoma that can cause pressure spikes, corneal edema, atonic pupil and, in some cases, optic nerve damage if the pressure is high for several weeks.”
The first aspect, the width measurement, is best done using ultrasound. “We concluded that calipers and a white-to-white measurement wasn’t the best way to do it,” says Dr. Moshirfar. “Now, the standard is ultrasound biomicroscopy. The Sonomed machine, which scans between 35 and 50 MHz, gives a good sulcus-to-sulcus measurement. It’s OK for a tech to measure it, but either you or someone else who’s competent in reading ultrasound should interpret it.
“Over the past four years,” Dr. Moshirfar continues, “I’ve also learned that it’s not just the sulcus-to-sulcus measurement that’s important, but also the shape of the anterior curvature of the crystalline lens. I’ve seen some eyes in which the curvature of the anterior surface of the crystalline lens has a high rise to it, and they look almost spherical. Then, in other cases, you have myopes in whom the crystalline lens’s anterior capsule is instead very flat-looking. Ultrasound or even the Visante OCT can show you the curvature of the anterior surface of the lens to some degree, with UBM being the better choice. Based on the sulcus-to-sulcus measurement and the rise of the anterior capsule, every Visian ICL surgeon has developed a nomogram that gives us less risk of being surprised after surgery. If the rise is steep, I will usually oversize the lens. If it’s flat then I will undersize it.”
The third aspect of sizing to take into account is the amount of myopia being corrected. “If the power of the ICL is 7 D or less—such as in a forme fruste keratoconus patient on whom I don’t want to perform PRK—I usually try to oversize my ICL. So, if my nomogram says to put in a 12.1-mm lens, I put in a 12.6. On the other hand, if I have a correction that’s greater than -10 D, I usually try to undersize my ICL; if my nomogram says to implant a 12.6-mm lens, for example, I’ll put in the 12.1-mm lens. If someone were to ask which of the factors was most important, I’d say the number one is the sulcus-to-sulcus measurement, as it comprises 90 percent of my decision. Next in importance is the rise of the anterior capsule. Following that, the refractive error would be weighted a few percentage points.”
In terms of handling the procedure, Dr. Moshirfar says, for one, he doesn’t think the size of the peripheral iridectomy is important, but the location is. “I’ve had patients do perfectly fine with small peripheral iridectomies,” he says. “I think the ones who end up needing a large PI are the patients in whom the sizing wasn’t done properly; their vault is too much so the surgeon has to go back and do additional PIs or try to increase the PI’s size. I create two YAG PIs two weeks before the surgery. I’m meticulous about the PIs being peripheral and not mid-peripheral. Two weeks later, when I’m in the OR and have completed the lens implantation, I’ll bring down the pupil and use an angled Sinksey hook to gently stretch each PI to ensure patency.”
Managing the viscoelastic is another step during which surgeons can get into trouble. “I use OcuCoat and don’t try to overinflate the anterior chamber, because the more it’s inflated, the more I have to take out afterward,” Dr. Moshirfar says. “At the end, I remove the viscoelastic with passive irrigation. If you use a coaxial or bimanual I/A system, and the pupil is still dilated, you can cause transient capsular opacification.”
Dr. Moshirfar feels that if there are no problems early on with the ICL, that’s a good sign. “I’d say if you can properly figure out the lens sizing and the patient doesn’t have an issue in the first two weeks postop, you’re home free,” he says. REVIEW