The Perfect Candidate
In an ideal world, all patients could get the procedures they want. For presbyopic IOLs, however, the perfect patient can be difficult to come by. Zaina Al-Mohtaseb, MD, an assistant professor of ophthalmology at Baylor College of Medicine, discusses her ideal candidate. “Patients with excellent ocular surfaces are the first indication of a great candidate,” she says. “They should also have no co-existing ocular pathology and would like to be glasses-independent for most things, but understand they might need glasses for small print.
“Even if a patient is a good candidate, the most important thing is the preoperative discussion,” she continues. “If the surgeon and his team take the time to discuss realistic expectations for the presbyopia-correcting lens, then most patients are happy regardless of their personality.”
James Loden, MD, an ophthalmologist based in Nashville, Tenn., also discusses the importance of managing expectations preoperatively. “Sometimes, you’re going to have patients who set the bar so high that even with a perfect surgery and implant, they’ll be disappointed with their visual results,” he says. “So it’s important to manage these expectations preoperatively so they know what they’re getting themselves into. It’s a big-time management of expectations if pathology is present.”
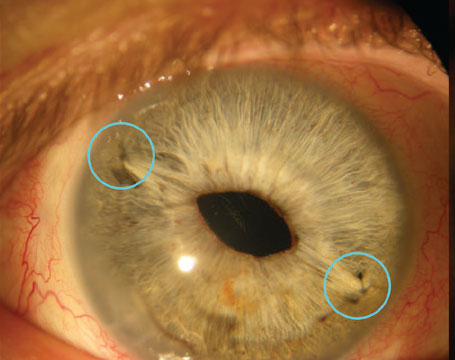
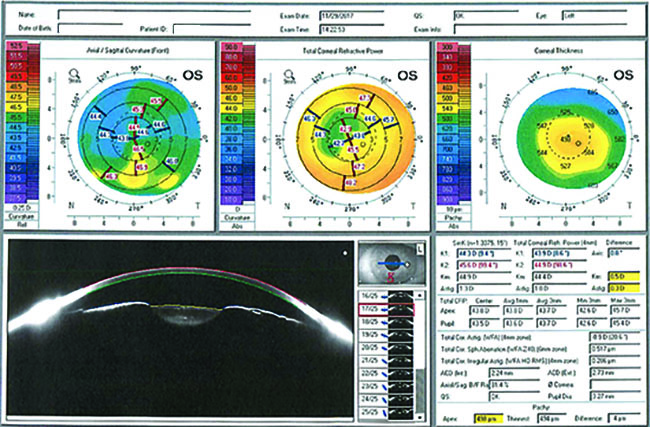 |
| A 71-year old man presented with a history of cataract. Scans showed dry eye, and the physician prescribed Xiidra before considering IOL implantation. |
Dr. Loden also describes his ideal candidate for these premium IOLs. “In terms of personality type, you’re going to want to look for someone who can manage their expectations—they’re a realist. There is likely going to be some follow-up that they’ll have to be on board for, and that’s important to identify from the get-go.
“You can’t be too careful,” he continues. “With age, dry eye becomes more and more prevalent, which absolutely needs to be addressed before surgery. And this is true with both a standard and premium IOL. You need to make sure the ocular surface is pristine. As with most surgeries, this will help with faster visual recovery and better postop results.” (For specific tips on matching a lens to a patient’s visual needs, see “Presbyopic IOLs: Choosing Wisely,” on pg. 30.)
Medical Pathology
Because not every patient will be an ideal candidate for these premium lenses, surgeons describe who might not be a great fit for the lenses and why. The most obvious indication that a patient will not be a great candidate comes from any medical pathology. Here are a few indications of a bad candidate to look out for:
• Fuchs’ dystrophy. “Most patients with co-existing corneal pathology won’t be an ideal candidate,” Dr. Mohtaseb says.
• Advanced dry eye. “Any pre-existing conditions need to be treated prior to surgery to ensure good outcomes,” she adds.
• Advanced macular degeneration. “These patients would also not be good candidates since this would result in decreased contrast sensitivity, decreased visual acuity, and glare/halos,” she continues. “You should take at look at the retina with a slit lamp or OCT. The lens might actually make the patient’s vision worse because of their AMD.”
• Anterior basement membrane dystrophy. “This will just kill you on chair time,” Dr. Loden notes, because of the necessity to address the ABMD as well as the cataract. “You’ll spend more time operating, even though these patients with anterior membrane dystrophy won’t see well with the lenses implanted. They won’t be satisfied with their outcomes, and you’ll have to bring them back in to either correct the lens or explant it.”
• Post-refractive surgery patients. “Any patient who has had prior refractive surgeries is likely not going to get great results,” Dr. Loden claims. “If they’ve had previous surgeries that have altered their refraction, there can be residual refractive errors. The patient might be left with blurry vision and dysphotopsias.”
• Weak zonules. “There’s also an issue with implanting lenses in eyes with weak zonular support because they could dislocate,” Dr. Loden continues. “If you’re dead set on implanting though, you can put in a capsular tension ring, which should make it a bit easier to reposition the IOL. It just might be a pain for the patient to have issues with decentration, but that’s something you should be transparent about preop.”
• Glaucoma. “The earlier the disease, the more options you can explore regarding some multifocal, premium IOLs,” Dr. Loden says. “However, there are ocular refractive changes that occur after glaucoma surgery which would be a good reason to advise against these lenses. It’s especially bad to implant one of these lenses if the patient’s glaucoma is progressing or poorly controlled.”
To help catch patients such as those described above, Dr. Mohtaseb recommends, “getting topography (look at the mires) and macular OCT on patients to evaluate if a patient is a good candidate or not.”
“Ignoring these signs of bad candidates will cost you too much chair time for suboptimal results,” according to Dr. Loden. “Any ocular surface disease has to be corrected preoperatively. These patients won’t be satisfied with their outcomes otherwise, no matter how perfect the surgery and implantation is. You have to be cautious and judicious with those outcomes.
“It doesn’t matter if you’re charging them $500 or $1,000,” Dr. Loden continues. “Once you charge them, they expect perfection, and they don’t always understand that pathology is a limiting factor, so they’re dissatisfied with their
results even if you do a perfect procedure. We need to make sure we talk about these things preop. With pathology present, you have to manage expectations.”
Psychological Mismatch
Along with the obvious medical signs of a bad candidate for these premium IOLs, there are other red flags that visual tests won’t detect. The personality types of your patients can also be a good indication of whether or not a premium IOL is right for them.
“I recommend avoiding the older-generation, high-add models in obsessive/compulsive people or very particular people, given the risk for postop glares and halos,” Dr. Mohtaseb says. “More often than not, they’ll be back to have the lens explanted. There are plenty of alternatives to these high-add premium IOLs, and I am much more comfortable placing the low-add multifocals and extended-depth-of-focus lenses in these patients now. I think the most difficult patient is still the low myope (-2 D) who had crisp reading vision for years, because they’ll take a long time to adjust to their vision and probably won’t be satisfied postoperatively. It all goes back to managing expectations and your instinct about whether or not they’ll adjust to the lens.”
Dr. Loden also shares his experiences with evaluating the personalities of his patients to see if they’ll be a fit for these lenses. “There are definitely some psychological signs to keep an eye out for, and you’ll learn most of it from just talking with your patients. Evaluate their visual needs. Ask if they mind wearing glasses. Do they consider themselves to be obsessive or a perfectionist? What are they hoping to gain from this procedure in terms of visual acuity? Would they prefer distance or near visual acuity? It’s also important to evaluate their state of mind as best you can, too. If you have a depressed patient, you probably shouldn’t implant one of these lenses, as adjusting to the new, imperfect visual acuity might be stressful. It’s important to take the time to talk with them, and use your gut to make the call. There are plenty of other options that might better suit your patient. It’s okay to go in a different direction,” he says.
Careers
Along with a patient’s psychological makeup, his or her career should also be taken into account when looking at implanting a premium IOL. For example, say your patient is an editor who needs closer visual acuity to edit his work. You’ll definitely want to keep that in mind while evaluating whether or not to implant a premium IOL.
“In the older models of presbyopia-correcting lenses with significant add-power, some patients in certain occupations were not happy with the results of the lenses,” Dr. Mohtaseb says. “For example, night drivers or patients who required excellent and crisp distance vision, such as pilots, were not good candidates because of the compromise of the distance vision. We looked at our surgical indications for removing these presbyopia-correcting IOLs and found that distance vision and glare, halos and dysphotopsias were the most common issues that patients had. I would also recommend avoiding implanting these lenses in very particular people, such as an engineer who asks how the optics of the lens work.”
“There are definitely some obvious indications for these lenses based on patient careers,” Dr. Loden says, “but as I said, you can figure all this out if you talk to your patients and evaluate their needs based on their lifestyles, and make a judgment call. If the patient has a profession that calls for distance visual acuity, then you’re probably best served looking elsewhere for a nonpremium lens.”
Looking Ahead
Despite the many benefits of premium IOLs, there are plenty of patients who just aren’t suited for them. Surgeons advise exploring other lens options. Even with perfect surgery and implantation, a patient not fit for these lenses will still be dissatisfied, leaving you and him frustrated. Beyond the medical contraindications, make sure your patient’s psychological makeup can adapt to these lenses.
“Taking the time to understand your patient’s needs makes the difference between a satisfied patient and a frustrated one,” Dr. Loden says. “It’s on you to recommend the lenses that are best for them.” REVIEW
Dr. Loden is a consultant for LENSAR, J & J vision and Lenstec. Dr. Mohtaseb is a consultant for Alcon and Allergan.