 |
In addition to presbyopic lenses, surgeons responding to this month’s intraocular lens survey also weighed in on topics such as their favorite lens material, their opinions on IOL features and how they deal with lens complications. This month, the e-mail survey was opened by 1,259 of 8,743 subscribers to Review’s electronic mail service (14.4 percent open rate) and, of those, 80 surgeons shared their responses. See how your opinions on IOLs compare with theirs.
Presbyopic Opinions
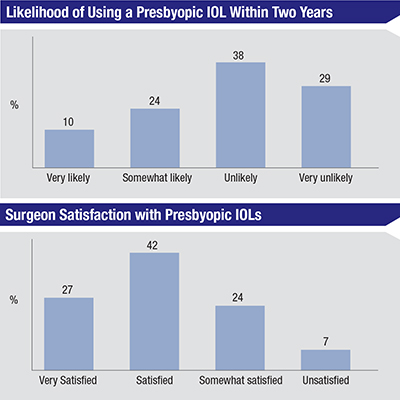
Three quarters of the surgeons say they use presbyopic IOLs, and they’re generally satisfied with the results they get with them.
On the survey, 27 percent say they’re very satisfied with presbyopic lenses and 42 percent say they’re satisfied. Twenty-four percent say they’re somewhat satisfied with the technology and only 7 percent are unsatisfied. Forty percent of the surgeons say they use the ReSTOR most often, 40 percent use the Tecnis multifocal the most and 20 percent primarily use the Crystalens AO.
A cataract surgeon from Indiana says he’s enjoying the benefits of the new 2.75-D multifocal Tecnis. “The aberration profile is much better with the lower-add multifocal,” he says. “It is substantially improved. However, any further improvements would be welcome, too.” Bruce Cohen, MD, of St. Louis also sees potential in the newer lenses. “The new Tecnis multifocals have been good thus far,” he says. “There is minimal glare and the intermediate add of the ZLB00 works well. I’ve had happy patients so far.” Dubuque, Iowa’s Juan Nieto, MD, feels the lenses have been a benefit to his practice. “I have had nice success with both the Alcon ReSTOR +3 and the Tecnis +4 multifocal,” he says. “I’ve recently started to use the Tecnis +2.75 multifocal, but I still haven’t made up my mind on that lens. I would love to have access to a toric multifocal.”
A surgeon from Tennessee says that, though he’s satisfied with his presbyopic IOL, things could be better. “Presbyopic IOLs are still a work in progress,” he says. “Nothing is very close to what we have naturally.” R. Wayne Bowman, MD, of Dallas feels similarly. “They are all a compromise,” says Dr. Bowman. “They have less-than-ideal side effect profiles and could be improved in every way.”
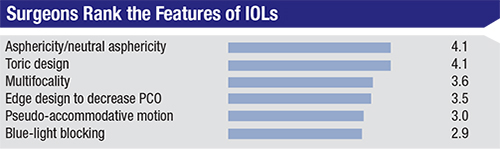 |
| Surgeons on the survey ranked IOL features in terms of their usefulness using a numerical scale that ran from 1 (least useful) to 6 (most useful). The average scores are shown. |
 |
Lens Material and Design
Surgeons also held forth on the various design elements in today’s IOLs, saying which ones have merit and which don’t have as much of an impact.
For monofocal IOLs, 52 percent of the surgeons say they most often use the AcrySof IQ Aspheric lens, 30 percent use the Tecnis one-piece lens and 8 percent use the B + L enVista lens. The other options were chosen by less than 5 percent of respondents. Eighty-six percent think acrylic is the best material, and 7 percent like silicone.
The surgeons gave their opinions on specific lens features by ranking popular IOL design elements, such as asphericity and multifocality, on a scale from one to six, with six being the most important to them. (The ranking results appear in the graph on p. 38.) Toric design and asphericity/neutral asphericity were the most popular features on the survey, each with an average score of 4.1. “Asphericity gives excellent optics and improves night vision,” avers Dr. Cohen. Dr. Bowman’s top two mirror the survey’s: “Correction of astigmatism and optical quality are the two most important issues,” he says. A surgeon from Maryland feels that special edge designs that decrease posterior capsular opacification can make a big difference postop. “The rate of posterior capsular fibrosis is important,” he says. “It can change the patient’s refractive error in the first few months postop when I would prefer not to perform a YAG capsulotomy. Centration and stability in the bag are very important to promote less shifting.” On the low end of the scale were blue-light blocking (2.9) and pseudo-accommodative motion (3.0).
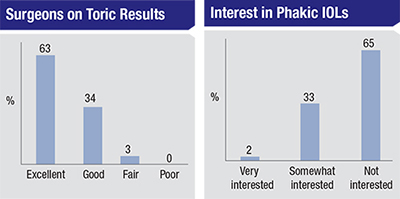
As surgeons’ rankings show, toric IOLs are very popular; 73 percent of the respondents say they use them and most are happy with their outcomes. Sixty-three percent of the surgeons say their toric IOL results are excellent and 34 percent rate them as good. Only 3 percent of the surgeons call their outcomes fair. “I get excellent visual results with toric IOLs, and very happy patients,” says a surgeon from Utah. “These IOLs provide significant improvements in vision with no visual compromises.” Dr. Nieto also values torics. “I’ve had excellent results with the Alcon toric IOLs,” he says. “It’s a wonderful lens option.” A doctor from Texas says he likes the ability to “adjust the Tecnis toric IOL forward and backward easily.”
 |
Lens Complications
Surgeons also weighed in on what they do when things don’t go as planned with their lens implantations.
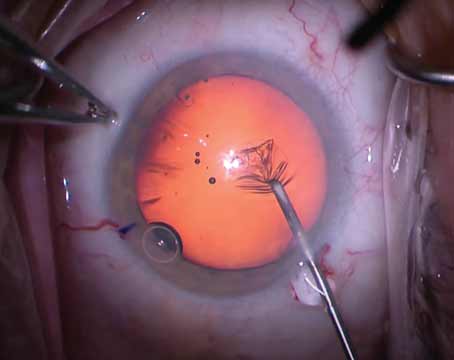
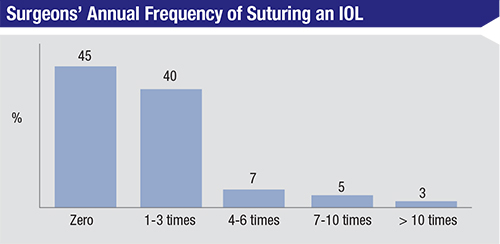
When asked about instances when they need to suture-fixate an IOL, 45 percent say they haven’t had to suture a lens in the past year, 40 percent had to do it one to three times, 7 percent sutured a lens four to six times, 5 percent did it seven to 10 times and 3 percent of the surgeons had to suture a lens more than 10 times. Surgeons give various reasons for having to do this, chief among them being capsular instability. “I’ve done it for either a dislocated IOL postop or no capsular support during initial surgery,” says a Utah surgeon. “I suture it either to the iris or the ciliary sulcus.”
Forty-four percent of surgeons had to explant at least one lens in the past year. Here are some of the most common reasons they gave for the explantation:
• wrong power;
• decentration;
• late dislocation of lens in the bag;
• poor tolerance of a multifocal IOL; and
• uveitis/glaucoma/hyphema syndrome.
One surgeon from Washington state no doubt speaks for many of his colleagues when he says that his main reason for suturing an IOL is, “So I can sleep better.” REVIEW