In addition to being a sophisticated, highly efficient way to restore a patient’s sight, cataract surgery can also work its magic on certain glaucoma patients by lowering their intraocular pressure without the need for an adjunctive glaucoma procedure. Glaucoma experts say, however, that the key is discerning which glaucoma patients will benefit from cataract surgery alone and which will require a combined procedure. Telling the two groups apart isn’t always easy, but if you’re able to, you can spare these patients the risks of a second procedure while still enjoying the benefits of lower pressures. In this article, surgeons share their techniques for identifying the patients most likely to benefit from cataract surgery alone.
Cataract Surgery’s Benefits
Surgeons say that studies have found a very real benefit from cataract surgery in certain fortunate glaucoma patients.
In one study with 10 years of follow-up, surgeons analyzed the final intraocular pressure reduction in five groups of cataract-surgery patients (124 eyes), segmented by preop IOP levels. They found that the higher the preop IOP, the more pronounced the postop IOP decrease was. The final mean IOP reduction was 8.5 mmHg (34 percent) in the 29 to 23 mmHg preop IOP group, 4.6 mm Hg (22 percent) in the 22 to 20 mmHg group, 3.4 mmHg (18 percent) in the 19 to 18 mmHg group, and 1.1 mmHg (10 percent) in the 17 to 15 mmHg group. In the 14 to 5 mmHg preop IOP group, IOP actually increased by 1.7 mmHg (15 percent). Though other studies have found varying durations of this IOP decrease, usually a couple of years, in this particular study the one-year IOP reductions persisted for 10 years and didn’t differ by age. The researchers concluded that the aging crystalline lens may be a significant cause of ocular hypertension and glaucoma, and that phaco may help prevent and treat glaucoma.1
In a more recent, retrospective study of 60 primary angle-closure glaucoma patients, the researchers looked at the effect of phaco. They found that the mean IOP after cataract surgery decreased significantly (4.5 mmHg, p<0.01). Also, 20 percent of the patients were able to discontinue anti-glaucoma medication after surgery. They say the change in IOP didn’t correlate with lens thickness or anterior chamber depth.2
In addition to direct health benefits, performing cataract surgery alone may have clinical benefits, as well. “I’m a proponent of doing cataract surgery, because it makes all of our diagnostic testing better postoperatively,” explains Fairfield, Conn., glaucoma specialist Robert Noecker. “Sometimes, when the cataract is in the way, you can get a bad signal and you can’t always take things at face value. For example, visual fields may be unsatisfactory because of the interference of the cataract. But when the cataract is out, it helps your future evaluation of the patient.”
Choosing Patients Wisely
|
• Number of medications. “Those patients on zero, one or maybe even two glaucoma medications are likely to do better with cataract surgery alone than someone on maximum medical therapy,” says Yale glaucoma specialist James Tsai, MD. “If a patient is on three or four classes of glaucoma medications—and I count Combigan or Cosopt each as two classes—I’ll consider combined surgery instead.”
• Examine the angle. Gonioscopy, which some surgeons say is a lost art, reveals a lot of pertinent information, surgeons say. “Gonioscopy shows us that, if the patient has already had a laser iridotomy and his angle is very narrow or almost closed despite the iridotomy, there’s a good chance that his cataract is contributing to the glaucoma,” says Duke University glaucoma specialist Sanjay Asrani, MD. Surgeons recommend using a four-mirror handheld lens so compression can be performed. “When I do gonioscopy, I note whether I’m able to compress the eye easily to open the angle with the goniolens,” Dr. Asrani says. “If I’m unable to compress easily, it’s likely that the agent that’s not allowing me to compress is actually the cataract. If I’m able to compress easily, then most likely the narrow angle is from pupillary block—meaning a fluid cushion that I’m able to easily compress and open up the angle. Note that if a patient has already had a laser iridotomy, he shouldn’t have pupillary block.
“The other feature I examine is the pigmentation in the trabecular meshwork,” Dr. Asrani continues. “If the pigmentation is pockmarked, then it’s likely that the iris has butted up against the trabecular meshwork and left extra pigmentation in those areas, leading to spotty pigmentation. Many patients with coexisting cataract and glaucoma have a narrow-angle component, so the challenge is to identify it, doing gonioscopy carefully in a low level of light, not crossing the pupil and understanding that you shouldn’t assess the angle as soon as you put on the goniolens, but instead 10 to 15 seconds later. You have to wait for pupillary block to recur during gonioscopy in order to assess the true nature of the angle.”
|
If synechiae are present, it doesn’t bode well. “If there are areas of synechiae between the iris and trabecular meshwork, that tells me that the apposition between the trabecular meshwork and the iris has been present for quite some time,” explains Dr. Asrani. “The meshwork in those areas is not functioning. Large areas of synechiae lead me to believe that the cataract surgery alone won’t have a significant effect by itself.”
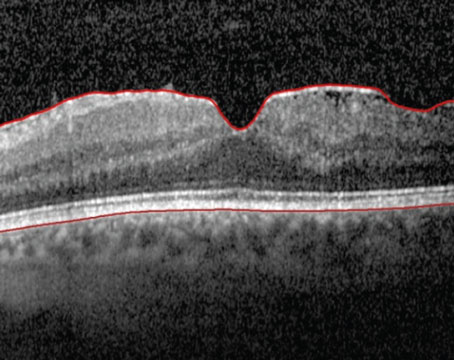
Dr. Noecker says ultrasound can be very helpful when assessing the anterior segment. “I think it’s definitive,” he says. “Though anterior segment OCT is less-invasive, and can give you an idea of the angle contour, it’s limited by the front side of the iris. With UBM, you can see behind the iris, where you might see something like plateau iris.”
• Assess the IOP, nerve and visual fields. Surgeons say that, though patients with higher pressures preop tended to get more pressure lowering in studies, it doesn’t mean all severe glaucoma patients should just get cataract surgery. “I think, in general, it’s better to be doing cataract surgery alone on mild to moderate glaucoma patients and those without a very high pressure,” says Atlanta glaucoma and cataract surgeon Reay Brown. “So it would be better to operate on someone who doesn’t have split fixation visual fields or pressures that are already far too high. It’s best to select patients who are maybe controlled on a couple of medications, or have pressures that are maybe a little higher than you’d like on medical therapy and do the cataract surgery alone on them. Then, afterward, you can regroup and see whether a further glaucoma operation is even needed.”
In addition to IOP, the other two keys to assessing the severity of a patient’s glaucomatous damage are visual fields and the state of the optic nerve. Dr. Noecker says a mix of imaging and microscopic examination can tell most of the story. “The optic nerve is the biggest factor,” he says. “The more damaged the nerve is, the more likely we’ll do a combined procedure, because we don’t want that optic nerve to get any worse. If they have a great-looking optic nerve and a pressure problem, cataract surgery alone is an attractive alternative. It’s the ones with these precarious optic nerves—really thinned out, big cups, thinning of the rim, maybe peripapillary atrophy, a disc hemorrhage on the nerve or a retinal nerve fiber layer defect—those are all high-risk characteristics. We’ll certainly think about doing something more in those patients, since they’re more diseased.” OCT of the optic nerve can also be useful, says Dr. Noecker. “Here, again, you’re looking for thinning of the nerve fiber layer. The important locations are superior and inferior, with the most important, most localized areas being infero-temporal and supero-temporal. The OCT correlates with our nerve exam and visual fields, and will help guide us. The more red we see on the test, the more we worry about it.”
With visual fields, also, the worse they are, the less-inclined surgeons are to rely on cataract surgery alone. “Anyone with a visual field defect getting close to fixation which will impair his vision or who has a central island will need a combined procedure,” says Dr. Noecker. “If he’s at high risk we don’t want his defect to get worse and move into the middle of his vision. I think severe disease with visual field loss above and below the horizontal meridian is a high-risk characteristic, as well.”
Dr. Asrani feels similarly, saying, “I consider a combined procedure if the patient has a paracentral visual field defect, especially in the inferior paracentral area. If that’s the case, a postoperative pressure spike—which is a risk that’s quite high in any cataract procedure—might cause him to have significant worsening of the visual field damage. In those cases, if I’m unable to use oral Diamox in the postop period, such as for the first couple of days, I’ll consider a combined surgery.
“The other scenario where I’d consider a combined procedure,” Dr. Asrani continues, “is if the person is allergic to a variety of medications and the optic nerve has already been compromised to a fair extent. In that case, it makes sense to do a combined procedure for the sake of convenience. Since we’re going to remove the cataract anyway, we might as well do a combined surgery at that time. Here the decision is being driven by the fact that the patient is allergic to a lot of medications, so you don’t have a lot of options to treat the worsening glaucoma. Of course, this would be in the setting of moderate to severe glaucoma, but not mild. If the patient had mild glaucoma and it was controlled before the glaucoma surgery, there’s a good chance he or she will be controlled after surgery, too.”
Beneficial Maneuvers
There is a small gray area between cataract surgery alone and combined procedures in which some surgeons say you can boost your odds of getting a good result from cataract surgery. This area consists of performing a procedure preop, or a surgical maneuver during the actual cataract surgery.
|
Dr. Brown says that an additional maneuver during the cataract surgery can help increase the odds of decreasing the pressure in certain patients. “If the angle is closed with PAS, then that might be a case where you perform goniosynechialysis during the cataract surgery,” Dr. Brown avers. “You grasp the iris with forceps and pull it out of the angle, removing the iris from the surface of the trabecular meshwork. The idea is to give the aqueous access to the meshwork.”
The Specter of the Spike
Even though a glaucoma patient may appear to be well-suited to have an IOP decrease with cataract surgery alone, surgeons say you have to be wary of postop IOP spikes.
“The postop IOP spike is one of the concerns of doing cataract surgery alone,” says Dr. Tsai. “As a surgeon, you assume that the trabecular meshwork isn’t functioning normally since the patient already has glaucoma. They’re more at risk for a pressure spike. To decrease the risk, you will have to pay close attention to not overfilling the eye with viscoelastic during the cataract surgery, and to make sure to remove all the viscoelastic at the end of surgery. We’re getting better with modern cataract surgery, however, since we currently use less viscoelastic and remove it more completely afterward.
“One thing to consider is that a substantial number of glaucoma patients have exfoliative syndrome that’s either diagnosed or undiagnosed,” he continues. “Exfoliative syndrome tends to pose a higher risk of vitreous loss and/or zonular dehiscence/instability, and the glaucoma tends to be more aggressive. If you have a patient with exfoliative glaucoma, you have to be confident that you’ll be able to control his or her IOP postoperatively, and this is one of the reasons why we used to perform a lot more combined procedures some years ago. Now, with smaller incision surgery, the tendency for glaucoma surgeons is to perform cataract surgery alone, which does lower IOP by itself, in patients with mild to moderate glaucoma, thereby not subjecting them to the risks and the longer postoperative recovery period of a combined procedure.”
Glaucoma medication at the time of surgery can be crucial to blunting a spike. “My partner gives everyone Diamox at the time of cataract surgery,” says Dr. Brown. “I give timolol at the end of surgery, though many of the glaucoma patients are already taking it. I also make sure that the patients use their glaucoma drops the day of surgery so they don’t miss a round or two of doses, which I think is very important. You don’t want to get off on the wrong foot, because if you look back at the patients who do poorly, you’ll see that the patients with the pressure spike on the first day after surgery are at much higher risk for having problems with prolonged pressure elevation.”
Dr. Brown says that, if you select the patients correctly and they achieve a postop IOP benefit after cataract surgery, it’s a great feeling because it was relatively easily acquired compared to other surgeries or interventions. “That’s the best thing about it: There’s not much drama involved with it,” he says. “There’s enough drama in glaucoma treatment already.” REVIEW
1. Poley BJ, Lindstrom RL, Samuelson TW, et al. Intraocular pressure reduction after phacoemulsification with intraocular lens implantation in glaucomatous and nonglaucomatous eyes: Evaluation of a causal relationship between the natural lens and open-angle glaucoma. J Cataract Refract Surg 2009;35:11:1946.
2. Yudhasompop N, Wangsupadilok N. Effects of phacoemulsification and intraocular lens implantation on intraocular pressure in primary angle closure glaucoma (PACG) patients. J Med Assoc Thai 2012;95:4:557-60.