Presentation
A 62-year-old male was referred to Wills Eye Hospital for hypotony and decreased vision in the left eye after routine cataract surgery and iStent placement 18 months prior by an outside ophthalmologist. Ocular history was notable for primary open angle glaucoma in both eyes, managed with latanoprost in the right eye only.
After the cataract surgery, although vision was 20/25, intraocular pressure had fallen to 8 mmHg without evidence of hypotony maculopathy. Initial gonioscopy showed a well-positioned iStent implant in the trabecular meshwork, and the patient was monitored without intervention. Over the next several months, the patient’s visual acuity and IOP remained unchanged as postoperative medications were tapered.
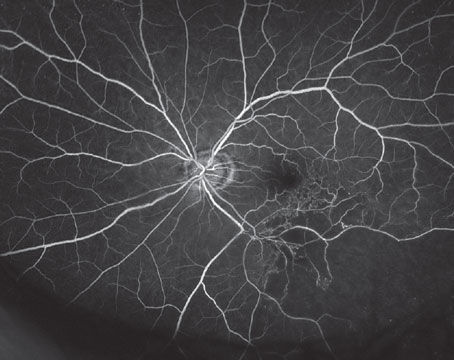
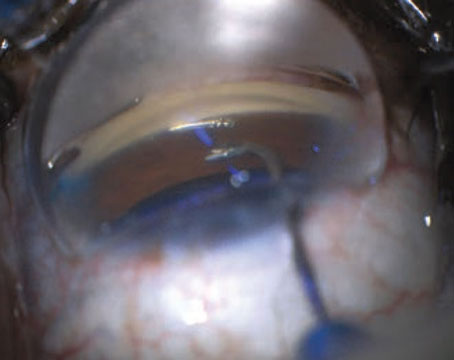
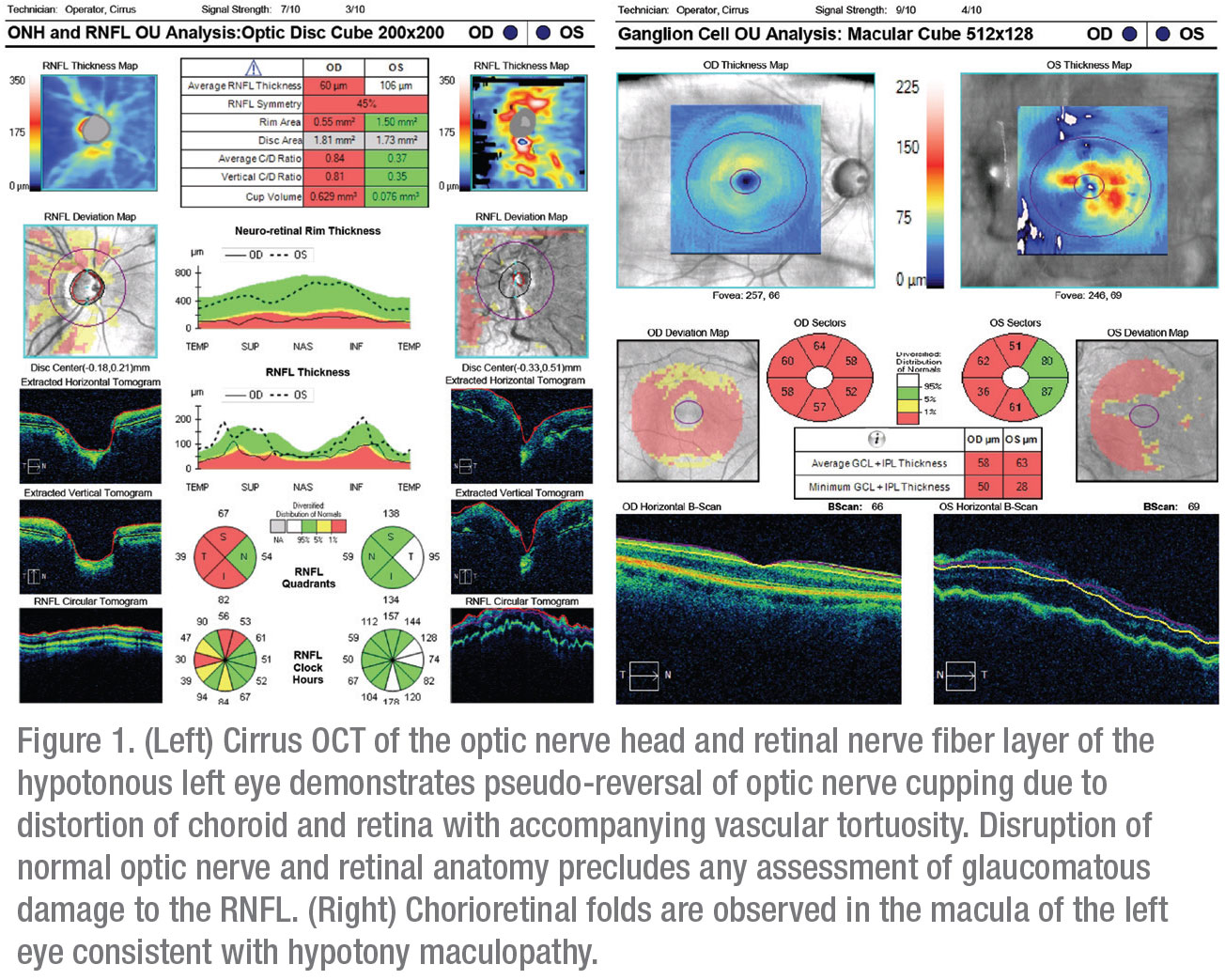
Five months after surgery, the patient’s vision suddenly declined to 20/200 despite no meaningful change in IOP. He denied associated headaches, eye pain, photopsias or floaters. He was referred to a local retina specialist after an optical coherence tomograph of the optic nerve and macula demonstrated changes consistent with hypotony maculopathy (Figure 1). His low IOP was attributed to the iStent, and he was scheduled to have it explanted. Despite successful removal of the stent several days later, his postop IOP remained between 6 and 8 mmHg, and his vision failed to improve. He was subsequently referred to the Wills Eye Hospital Glaucoma Service for further management.
Medical History
Past medical history included gastroesophageal reflux disease, Crohn’s disease and attention-deficit hyperactivity syndrome. His past surgical history was notable for cataract extraction and intraocular lens placement in the right eye several years prior, in addition to the recent CE/iStent procedure in the left eye. Family and social histories were noncontributory, and he reported no drug allergies. Oral drugs included dexlansoprazole, adalimumab, escitalopram and atomoxetine. At the time of his presentation, his only ocular medication was latanoprost in the right eye.
 |
Examination
Ophthalmologic examination revealed a best-corrected visual acuity of 20/20 OD and 20/400 OS. The patient’s pupils were equal, round and reactive to light without an afferent pupillary defect. IOPs were 14 mmHg OD and 8 mmHg OS. Extraocular motility was full in both eyes, but the patient was unable to perform confrontation visual fields and color plates OS. Slit lamp exam demonstrated a moderately deep and quiet anterior chamber bilaterally, with well-centered intraocular lenses in the capsular bag OU. Surgical wounds were Seidel negative in both eyes. Funduscopic exam of the right eye demonstrated previously known optic nerve cupping with an otherwise normal macula and retinal periphery. The left eye demonstrated diffuse, horizontally-oriented chorioretinal folds, tortuous and enlarged retinal vessels, and optic nerve head swelling.
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.