Here, surgeons discuss new advances in phaco, as well as technologies that, if they can’t overthrow the king, can maybe make cataract surgery a little safer in softer nuclei by avoiding the use of ultrasonic energy for every cataract.
Alcon’s Centurion System
In the fall of 2013, Alcon introduced a new phaco system designed to give surgeons more control over the phaco environment within the eye and help make the procedure safer and more efficient.
|
• Active Fluidics. One of the primary features introduced with the new system is the ability for the surgeon to set a target intraocular pressure for the eye and have the system automatically modulate flow to maintain that IOP throughout the case. “Traditionally, phaco machines have used a bottle height at a level that the surgeon desired to create flow into the eye,” says Robert Cionni, MD, of the Cincinnati Eye Institute. “That’s a static system and, typically during quadrant removal or removal of cortex or viscoelastic, surgeons usually ran a bottle height of 100 cc. There wasn’t a really good understanding of what that’s doing to pressure or flow in the eye, however, and we’d kind of titrate our vacuum to a certain bottle height. That kind of system is good and has worked for years, but it tends not to be very responsive to changes to the pressure in the eye, specifically with regard to occlusion breaks.
“For example, say a nuclear chip is occluding the tip,” Dr. Cionni continues. “The vacuum goes up to 350, 400 or whatever the surgeon had the maximum vacuum set at, and when phaco breaks up the chip, the occlusion goes away very quickly and suddenly you have a tremendous influx of fluid into the tip. This influx causes a fluctuation in the chamber, or a chamber collapse, in which the iris and posterior capsule come toward the tip. This sets up a dangerous situation and limits the vacuum level we can use during phaco. The lower the vacuum level, the less efficient phaco is, while the higher the vacuum level, the more efficiently material moves into the tip and the cataract can be removed with less ultrasound time and fluid being used. However, the ultrasound time, the amount of energy delivered to the eye and the amount of fluid that goes into the eye correlate with the amount of edema you see postoperatively.
“The active fluidics system works differently,” Dr. Cionni adds. “You don’t hang a bottle. Instead, inside the machine there’s a collapsible plastic bag of infusion BSS that is compressed by pressure plates. In order to maintain a specific pressure in the eye, the pressure plates can squeeze the bag or relax their pressure on it. For instance, take the case of a myopic patient who has had a vitrectomy. If the pressure goes from zero to whatever the bottle was hung at, then you can have a sudden pressure change in the eye and a severe pupillary block—a very painful situation for the patient. With Centurion, we can tell it to bring the pressure up to
60 mmHg, but to do it over a period of a couple of seconds rather than immediately. This more gradual pressure rise is more manageable by the surgeon and there’s less pain. Likewise, when you get an occlusion break, the pressure sensors can squeeze the bag very quickly to give an instant influx of fluid so you have less of a chamber collapse.” Several years ago, B + L instituted a similar system in its Stellaris phaco machine to achieve gas-forced infusion to help keep chambers deep during occlusion break situations.
To give a sense of how this compares during surgery to Alcon’s previous system, the Infiniti, Dr. Cionni provides some numbers. “With Infiniti, with a bottle height of 100 cc and an IOP of 84 mmHg, the max vacuum pressure I’d recommend for surgery would be 350 mmHg, controlled linearly,” he says. “So, this means that the farther down on the pedal you push, the more vacuum you get. With Centurion, I can go to a vacuum level of 600 mmHg—almost double—to give a more efficient procedure, but set the IOP at 60, which would be equivalent to a bottle height of 84 cc. So, we’d have a lower pressure in the eye, a more stable chamber and more efficient phacoemulsification.”
• Separate control over flow and vacuum. University of Utah surgeon Alan Crandall says the system’s functions allow it to somewhat mimic a venturi-based system in different situations. “For your average cases, you probably won’t notice a difference with it,” he says.
|
Nano Laser Phaco
When faced with the prospect of battling such an efficient, entrenched procedure as phaco, some companies have taken the approach of “if you can’t beat them, join them.” It’s with this thought in mind that Germany’s A.R.C. Laser company developed its nano laser phaco system, Cetus.
Rather than existing as a standalone box with all the irrigation/aspiration equipment of a phaco machine, Cetus is designed to be hooked up to a surgeon’s existing phaco machine to help emulsify relatively soft nuclei—grade 3 and below—using less energy than regular phacoemulsification and without the use of a sharp phaco tip in the eye. “The philosophy is that we only provide a machine for energy delivery, but instead of using ultrasound energy we use a laser,” explains Rudolf Walker, PhD, A.R.C. Laser’s head of applications. “The inflow and outflow we take from the surgeon’s ultrasound machine. We instead deliver a module. So, to use the nano laser, you take the I/A of your original phaco machine and combine it with our system. We also don’t replace manual surgical steps such as the capsulorhexis and the incision.” To accomplish these steps, surgeons still need to use a manual technique or a femtosecond laser.
The Cetus operates by using a YAG laser inside its tip to create a shockwave that emulsifies material. “Instead of a large, bulky ultrasound handpiece, we use a small, disposable plastic handpiece,” Dr. Walker explains. “The handpiece works by the laser striking a titanium target at the tip—so the laser doesn’t interact with any tissue. It’s the laser hitting the target that causes the emulsification.”
|
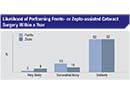
One of the limitations of the technology, though, is that it doesn’t work for all cataracts, so surgeons’ phaco handpieces should be waiting in the wings for patients with greater than 3+ nuclei. “When the nucleus gets very hard, the efficiency with our nano laser isn’t as good as our ultrasound system,” he says. “We can’t replace ultrasound completely. So, with nuclei graded 4 or harder, you’re better off using ultrasound. However, Cetus can replace ultrasound for 50 to 70 percent of a surgeons’ patients, depending on his patient cohort, of course.” Dr. Walker says studies are currently under way to analyze the system’s energy usage and its effect on endothelial cell counts.
In terms of approval status, the Cetus is available in Europe, but not in the United States. “The techniques and basic operation of the laser come from the old Dodick laser system that was approved by the Food and Drug Administration in 1999,” says Dr. Walker. “We changed the handpiece to a coaxial one from a bimanual, which was big step forward. So, we will see if we can get a quick approval because the Dodick system is already approved.”
Catapulse
The Med-Logics Catapulse system is also designed to do away with ultrasound energy, at least for softer cataracts. However, instead of using a laser, the Catapulse uses pulsating vacuum power. The Catapulse is currently in development, and isn’t available for sale.
“As IOL technology gets better, cataract surgery is moving toward the refractive end of the spectrum,” says Antonio Mendez Noble, MD, a surgeon from Tijuana, Mexico, who has helped study the Catapulse for Med-Logics. “Because of this refractive emphasis, the cataracts we’re removing now often aren’t very hard; instead they’re soft and don’t require that much energy. So, we started working with vacuum rather than ultrasound energy, and found that by turning the vacuum on and off very quickly when the nuclear fragment hits the tip an energy is produced that will break up almost anything.”
The Catapulse uses its own irrigation/aspiration unit and uses a plastic, 0.9-mm rounded tip. “The tip doesn’t have a sharp edge or produce heat,” says Dr. Mendez Noble. “For the Catapulse procedure, it’s important to pre-fracture the nucleus, because the tip can’t burrow into it. Any type of nucleus fracturing technique works. I use the Akahoshi pre-chopper instrument for this, though, of course, the system also works well with the femtosecond laser for segmenting the nucleus.”
To provide irrigation during the surgery, Dr. Mendez Noble says the current Catapulse technique involves a bimanual approach. “Right now, the second instrument I use is an irrigator,” he says. “I can add any type of tip or manipulator to the irrigator, as well, but right now I just use irrigation.” He says the Catapulse machine currently uses a duty cycle that the surgeon sets in order to control the device’s vacuum pulsations, but neither he nor the company have hit on what the ideal pulsation rate is. “We’re playing around with that right now,” he says.
As to where the Catapulse device may fit into the cataract surgery spectrum, and what it brings to the table, Dr. Mendez Noble says the machine’s primary benefit is safety. “There’s no assembly, the handpiece comes complete with the tubes and the cassette, and you just hook up the cassette to the machine,” he explains. He says this avoids some difficult situations that can occur with conventional phacoemulsification. “In phaco, I’ve experienced situations where for some reason the tubing isn’t seated well on the back of the handpiece and I subsequently get into trouble. Or, the tip of the phacoemulsifier isn’t tight enough and you have problems with phacoemulsification. Other times, you may put the sleeve over the tip and find that the sleeve ruptures or has a small hole in it for some reason. All these potential problems are avoided with Catapulse because it’s just one piece that you hook up and begin using. Also, again, there’s no heat or energy released from the tip. Though there is the possibility of maybe catching the capsule and rupturing it, at the times when we’ve gotten into iris or capsule, we haven’t had any ruptures or iris burns.”
However, even though Catapulse may theoretically make the procedure safer for some cataracts, as with Cetus, surgeons can’t throw away their ultrasound phaco equipment. “Anything over grade 3, you’ll need ultrasonic phaco,” says Dr. Mendez Noble, who adds that though he’d like to do away with using ultrasound energy for cataracts, it may always have a place in ophthalmology. “Everything we do now is to try to avoid using ultrasound [in cataract surgery]. We know phaco works and is especially great for hard cataracts, and maybe developing countries will still need phaco for the cataracts there, which tend to be harder. There, it’s still the ideal procedure.” REVIEW