When compared to adult refractive surgery, the field of pediatric refractive surgery has remained relatively limited, with slower growth. Indeed, refractive surgery has a limited scope in the pediatric population; however, in certain cases, it can be a crucial treatment for high refractive error and anisometropia. Addressing these conditions in young children is critical to healthy visual maturation. High refractive errors that go uncorrected are almost certain to have a significant negative impact on a child’s intellectual and social development. When conservative methods such as glasses and contact lenses fail, surgical correction of refractive error is the most reasonable solution. In this article, I’ll describe the best applications for refractive surgery in this unique population.
Why Refractive Surgery?
Glasses, contact lenses and occlusion therapy can fail in children for a number of reasons. Developmental delay in conditions such as autism, cerebral palsy and Down syndrome can make patient compliance with these methods of correction extremely difficult. Many of these children don’t like the sensation of glasses touching their face. In cases of high ametropia, spectacles can be difficult to wear due to prismatic aberration, reduced field of vision through the lenses and cosmetic appearance. Contact lens placement is challenging in all children, whether developmentally appropriate or not. Even when children seemingly comply with glasses, there’s a good chance that they may be favoring their good eye without their parents’ knowledge. Finally, the efficacy of occlusion therapy is highly dependent on the patient’s and family’s compliance with the regimen. Regardless of the treatment modality, in all cases of conservative management there’s a small window of time for optimal visual development, so consistency and adherence to therapy is essential for success.
The main indications for refractive surgery in the pediatric population are anisometropic amblyopia and bilateral high ametropia. There have also been some studies of the role of refractive surgery for high accommodative esotropia. Elimination or drastic reduction of anisometropia equalizes the visual input of the two eyes and prevents favoring one eye over the other. Similarly, correction of the high refractive error improves the quality of visual input to both eyes. As stated previously, spectacles for high myopia and hyperopia can reduce image quality, which can compromise visual input to the eyes. Therefore, refractive surgery is an important consideration in such cases.
Refractive surgery has also been considered for refractive accommodative esotropia, though studies have been limited to adults and young adults. PRK has been the treatment of choice for this condition and it has been particularly successful in adults by reducing the amount of esotropia. Limitations for surgical correction in this setting do exist, however. PRK for accommodative esotropia may be best in young adults or older patients because of instability in the refractive error. Hyperopia decreases with age and the amount of hyperopia in accommodative esotropia can exceed the limits of laser ablation.
Several of the treatment modalities used in adults for refractive correction can be applied to pediatric cases. Laser vision correction, phakic intraocular lenses, clear lens extraction and limbal relaxing incisions can all be employed to improve children’s vision for the goals mentioned earlier. Correction of moderate to high refractive error significantly increases the chances of developing optimal binocular vision by first achieving a refractive equilibrium and, second, by eliminating aniseikonia due to anisometropia. Both high myopia and hyperopia can be treated surgically.
Laser Vision Correction
Laser vision correction options for children include PRK, laser-assisted subepithelial keratectomy and LASIK. PRK and LASEK have been commonly favored over LASIK to eliminate the risk of flap complications, namely dislocation and striae, and because of the difficulty of examining the LASIK flap postoperatively in children. It’s for this reason that we’ll focus on those procedures in this discussion.
The goals of pediatric laser refractive surgery are different from those in adult refractive surgery. Because spectacle independence isn’t the main concern for children, full correction of a child’s refractive error isn’t critical. What’s most important is that the refractive error is corrected enough to allow proper visual development and prevent visual isolation of one or both eyes. Surgery isn’t an option to be considered for cosmetic appearance or convenience, and parents should be reminded that their child’s eyes are growing and changing. Therefore, while pediatric patients may be emmetropic and not require glasses immediately after surgery, they will ultimately stabilize in a more myopic range and spectacles will likely be needed.
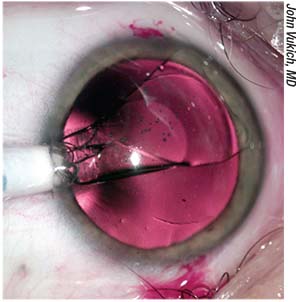 |
| A posterior-chamber phakic intraocular lens such as the Visian ICL can be an option in some pediatric cases. |
There are differences in the postoperative course of children compared to adults after PRK. The epithelial healing process is much more rapid and the duration of postoperative discomfort is much shorter in children. In one study, mean healing time was 3.5 days, with more than half of the patients healed as early as postoperative day three and all healed by day five.1 Overall, PRK can be quite successful in reducing high myopia and hyperopia in children.
Astigmatism correction can be challenging in children due to the general anesthesia that’s necessary in these patients. When under general anesthesia, the resulting cyclotorsion makes it difficult to identify the steep axis during treatment. With general anesthesia, surgeons have to make a concerted effort to fixate and center the child’s eye during treatment.
In addition to the procedural adaptations, performing laser vision correction in children requires more logistical planning than in adults. Most laser centers don’t have the capacity to perform monitored anesthesia, especially in the pediatric population. Therefore, in most cases, the excimer laser apparatus must be transported to a surgical center where general anesthesia can be performed. This is both labor-intensive and expensive.
Calgary’s William Astle, MD, and colleagues conducted a study of 56 eyes in 39 patients. The mean age of the patients was 6.5 years, with a range of 1 to 17.4 years. Inclusion criteria included patients who had more than 3 D of anisometropic myopia or more than -5 D of bilateral myopia and were unable to tolerate glasses or contact lenses. Refractive error ranged from +1.75 to -27 D. The surgeons performed either PRK or LASEK.
Postop, the mean spherical equivalent in all patients was -1.73 D. Most important, 49 percent demonstrated measurable stereopsis after surgery compared with just 18 percent before the procedure. There were no patients who experienced a reduction in best-corrected visual acuity or a loss of fusion. Investigators didn’t find significant differences in outcomes between PRK and LASEK, but did note slightly better preoperative and postoperative spherical equivalents in the LASEK group.2
Houston’s Evelyn A. Paysse, MD, and her fellow researchers looked at outcomes of PRK in 11 children with anisometropic amblyopia who were unable to comply with glasses or contact lenses. The mean preoperative refractive errors were -13.70 D in the myopic population and +4.75 D in the hyperopes. After PRK, mean refractive errors improved to -3.55 D in the myopes and +1.41 D in the hyperopes. Additionally, cycloplegic refraction confirmed that the two eyes of each patient were within 3 D of each other postoperatively. Uncorrected and best-corrected visual acuity improved by at least two lines in two-thirds of the patients.3
The primary risk after surface ablation in children is the development of corneal haze and ectasia. Noncompliance with a longer duration of postoperative steroid use is the principal risk factor for the development of corneal haze. In the Astle study, patients who underwent LASEK instead of PRK didn’t develop haze. The investigators favored LASEK over PRK both for this reason and because LASEK has less postoperative discomfort.2
Parents of children who are candidates for laser refractive surgery also should be counseled regarding the risk of keratoconus. Most pediatric patients won’t exhibit any subclinical or overt signs of keratoconus at such a young age. Therefore, at-risk candidates can’t be identified in the same way that adult refractive patients can. It’s important for parents to understand this risk and the possibility of accelerating or uncovering a corneal ectatic disorder down the road.
While there are drawbacks to laser refractive surgery in children, surface ablation remains a strong option for correcting refractive error in this young population. Even though LASEK has dropped in popularity for adult patients, it can still have a solid role in children given the absence of flap complications, enhanced postoperative comfort and healing, and a lower risk of haze formation.
Phakic IOL Implantation
Phakic IOLs can be considered for children with high refractive errors and amblyopia. There are three varieties of these types of lenses: iris-fixated; sulcus-supported; and angle-supported. Both iris-fixated and posterior chamber lenses have shown promise in correcting refractive error, providing binocular fusion and preventing amblyopia. Iris-fixated lenses, such as the Artisan/Verisyse, have been considered the lens of choice based on several studies. The first iris claw lens was implanted in a pediatric patient in 1997.
• Phakic IOL advantages. Phakic IOLs offer several benefits over other refractive surgery alternatives. They can correct a wider range of refractive error than laser surgery and their outcomes are more predictable. Also, there’s no risk of corneal haze, corneal thinning or future corneal ectasia with these IOLs. Phakic lenses are much less risky than refractive lens exchange, which can lead to glaucoma and retinal detachment. Posterior capsule fibrosis is not a concern with phakic intraocular lenses, and postop visual recovery and rehabilitation is much faster. Additionally, phakic IOLs can be removed relatively easily compared to IOLs placed after clear lens extraction. The logistical obstacles that come with pediatric laser refractive surgery are also avoided.
• Phakic IOL disadvantages. The disadvantages of phakic intraocular lenses include risks of endothelial cell loss, IOL dislocation, pigment dispersion, cataract formation and shallowing of the anterior chamber. Posterior chamber phakic lenses can cause anterior subcapsular cataracts if they are not adequately spaced from the natural lens. Complications associated with phakic intraocular lenses in adults have not been observed in children; however, this is likely secondary to a smaller number of cases performed and the need for longer-term follow-up. A caveat with iris-fixated lenses is that they shouldn’t be placed in anterior chambers that are smaller than
3.2 mm, to permit safe insertion and minimize the risk of long-term endothelial cell loss.4
• Data on phakic lenses. In 2011, Jorge Alio, MD, of Alicante, Spain, and his colleagues conducted a small retrospective study of 10 eyes in 10 children over five years. Nine had placement of an iris-fixated pIOL and one had a posterior chamber pIOL. At the time of implantation, patients ranged from 5 to 15 years old. All the patients with iris-fixated pIOLs had visual improvement of more than three lines of logMAR visual acuity. The patient with a posterior chamber pIOL had one line of improvement. Endothelial cell count in all patients remained over 2,000 cells/cm2.5
Lawrence Tychsen, MD, of St. Louis Children’s Hospital at the Washington University School of Medicine, studied 20 eyes after anterior chamber phakic IOL implantation to correct high myopia or hyperopia in the setting of neurobehavioral disorders. In the study, myopia ranged from -10 D to -22.75 D, and hyperopia ranged from +10.25 to +10.75 D. The patients’ ages ran from 4 to 17 years. Eighty-six percent of eyes were corrected to within 1 D of emmetropia. The remaining eyes were within 2 D of plano. Mean uncorrected visual acuity improved from 20/3,400 to 20/57. The residual visual acuity deficits were secondary to comorbid ocular conditions, including amblyopia, nystagmus, albinism and regressed retinopathy of prematurity.6
Andrea Ryan and her co-workers at Children’s University Hospital in Dublin, Ireland, looked at the results of 11 eyes in six children who couldn’t tolerate contact lens or spectacle correction due to neurobehavioral disorders and who underwent implantation of the foldable Artiflex iris-fixated pIOL (not available in the United States). Refractive indications included high bilateral myopia, anisometropia and myopic astigmatism. Mean spherical equivalent improved from -14.6 D to -2.4 D. Mean logMAR vision improved from 0.84 to 0.67 (a little better than 20/160 to just worse than 20/80).7 Residual visual deficit was secondary to amblyopia and ocular comorbidities. No complications were reported. The foldable design of the Artiflex lens means that it can be implanted through smaller incisions and requires fewer corneal sutures than the Artisan lens—an advantage in the pediatric population.
Posterior-chamber IOLs have shown promise in children as well. Talal Abdulrahman Althomali, MD, of Taif, Saudi Arabia, studied the placement of the toric Visian ICL in children aged 5 to 15 years with anisometropic amblyopia. Mean spherical equivalent improved from -10.21 D to -0.42 D. Five of six eyes gained more than three lines of visual acuity. No patient lost lines of vision and no intraocular complications were reported. All patients maintained proper alignment and positioning of the lens.8 Phakic PC-IOLs can be effective treatment options for significant astigmatism in children, possibly offering a better, more predictable and more precise alternative to laser correction of astigmatism.
CLE/RLE
Lensectomy with or without intraocular lens implantation is another surgical refractive option for children with high ametropia or anisometropia; however, it has several potential drawbacks. Posterior capsule fibrosis and the question of IOL implantation are the most immediate concerns. Some surgeons advocate primary posterior capsulectomy while others prefer YAG laser capsulotomy at a later time. Intraocular lenses are not as easily removed as phakic IOLs. Because these patients are so young and the eyes are still growing, future refractive error is unpredictable. As mentioned earlier, lensectomy also carries the risk of retinal detachment, which is greater in highly myopic patients, and glaucoma. Also, trauma can dislocate an IOL.
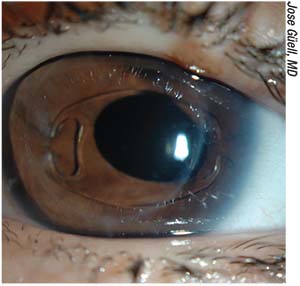 |
| Many surgeons say the foldable Artiflex phakic lens is a good option in children. |
In another study, Washington University’s Dr. Tyschen studied clear lens extraction in 13 children with neurobehavioral disorders, high myopia and noncompliance with glasses. The refractive goal was +1 D. Ten patients required only lens extraction and three required extraction with IOL implantation. Eleven eyes underwent primary posterior capsulectomy and subtotal vitrectomy. Eighty-one percent of eyes were within 2 D of the goal and 19 percent were within 4 D. Uncorrected visual acuity was significantly improved in all eyes. Thirteen eyes required vitrector or YAG-laser membranectomy due to capsular regrowth or opacification. Myopic regression was -0.15 D per year.9
Another study looked at seven children and adolescents who underwent lensectomy with a refractive goal of 0 to +4 D. Five eyes had lensectomy alone and two had lensectomy with intraocular lens implantation. Five eyes underwent primary posterior capsulectomy and subtotal vitrectomy. Eighty-six percent (six eyes) were within 3 D of the target. Uncorrected visual acuity improved in all patients, from a mean of 20/2,550 to 20/130. Myopic regression occurred at the rate of -0.43 D per year. The two eyes that didn’t undergo primary posterior capsulectomy had to undergo YAG-laser membranectomy. There were no retinal detachments.10
While lensectomy remains an option in pediatric cases, the long-term safety of this approach is still under study. Debate remains regarding whether an intraocular lens should be placed at the time of surgery or in the future. Additionally, with other, less-risky therapeutic options available, CLE is likely to remain a secondary choice for refractive correction in children.
In conclusion, although pediatric refractive surgery has limited applications, it offers several useful options for patients who are unable to comply with conservative methods of treating high ametropia, anisometropia and amblyopia. PRK, LASEK and phakic IOLs have shown great promise in the management of these refractive errors. Despite tremendous advances in adult refractive surgery, the use of these techniques in children remains infrequently studied, and we need more data on their long-term outcomes. More investigation is required to identify the most effective and safest approaches for pediatric conditions, and to tailor these procedures to this unique patient population. REVIEW
Dr. Balakrishnan is in private practice.
1. Paysse EA, Hamill MB, Koch DD, et al. Epithelial healing and ocular discomfort after photorefractive keratectomy in children. J Cataract Refract Surg 2003;29:3:478-481.
2. Astle WF, Fawcett SL, Huang PT, Alewaenah O, et al. Long-term outcomes of photorefractive keratectomy and laser-assisted subepithelial keratectomy in children. J Cataract Refract Surg 2008;34:3:411-6.
3. Paysse EA, Coats DK, Hussein MA, et al. Long-term outcomes of photorefractive keratectomy for anisometropic amblyopia in children. Ophthalmology 2006;113:169-176.
4. Moran S, O’Keefe M. The role of phakic intraocular lens implants in treatment of high refractive errors and amblyopia in children. Ophthalmol Ther 2013;2:1: 3-9.
5. Alio JL, Toffaha BT, Laria C, Pinero DP. Phakic intraocular lens implantation for treatment of anisometropia and amblyopia in children: 5-year follow-up. J Refract Surg 2011;27:7:494-501.
6. Tychsen L, Hoekel J, Ghasia F, Yoon-Huang G. Phakic intraocular lens correction of high ametropia in children with neurobehavioral disorders. J AAPOS 2008;12:3:282-289.
7. Ryan A, Hartnett C, Lanigan B, O’Keefe M. Foldable iris-fixated intraocular lens implantation in children. Acta Ophthalmol 2012;90:6:458-462.
8. Althomall TA. Posterior chamber toric phakic IOL implantation for the management of pediatric anisometropic amblyopia. J Refract Surg 2013;29:6:396-400.
9. Tychsen L, Packwood E, Hoekel J, Lueder G. Refractive surgery for high bilateral myopia in children with neurobehavioral disorders: Clear lens extraction and refractive lens exchange. J AAPOS 2006;10:4:357-363.
10. Ali A, Packwood E, Lueder G, Tychsen L. Unilateral lens extraction for high anisometropic myopia in children and adolescents. J AAPOS 2007;11:2:153-158.







