Thoughts on Centration
Surgeons center their multifocal IOLs based on a variety of factors, ultimately falling back on the process that works best for them.
Des Moines, Iowa, ophthalmologist James Davison bases his centration approach on the pupil and the capsulorhexis. “I don’t think you can use any one factor and hope that you’ll get it perfect,” he says. “And I’m not sure that it really matters to get it perfect. The manufacturers have built in a tolerance so the modulation transfer function of the lens isn’t affected even if it’s decentered almost up to a millimeter on the bench. Having said that, I’ll try to center the lens so that it looks right to me with respect to the dilated pupil at the time of surgery and the capsulorhexis that we made so that it’s overlapped completely. I’ll rotate the lens so that it sits properly and most of the time I end up leaving [the haptics] superior-temporal and inferior-nasal, with the AcrySof single-piece IOL, at least. I have no data for that at all; it’s just that seems to be a good spot for centering that lens in most people. But, if it doesn’t look perfect, I’ll rotate the haptics to a different location.”
Bakersfield, Calif., surgeon Daniel Chang has been working with Charleston, S.C., ophthalmologist George Waring IV on the concept that an effective centration point would be what they term the subject-fixated, coaxially sighted, corneal light reflex.
|
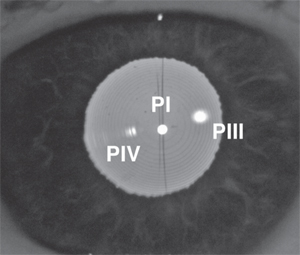
“Recently, I co-authored a paper with George Waring IV that’s now accepted for publication,” Dr. Chang continues. “And in it we advocate that the surgeon consider what we call the subject-fixated, coaxially sighted corneal light reflex. That’s a mouthful to say, but here’s how to understand it: The surgeon looks at the patient’s eye through a light such that the surgeon’s view is coaxial with the beam path of the fixation light. Then, if the patient’s eye is fixated on that same light source, the surgeon sees the reflection of the fixation light as the subject-fixated, coaxially sighted corneal light reflex—everything is lined up. It’s a unique lighting situation, and can be seen in various devices already in our practices. The SF-CSCLR is reproducible because it is related to the anterior corneal surface, and it doesn’t move around with implant position. Also, though this reflex is actually visualized at the iris/IOL plane, which eliminates parallax, the tricky part is having the patient fixate and using a light that’s coaxial with your viewing axis.”
At his practice, Dr. Chang did a small retrospective study of 117 Tecnis Multifocal IOL cases centered on the SF-CSCLR with an average follow-up of 100 days. “I looked at the uncorrected and best-corrected vision correlated to centering on the SF-CSCLR vs. centering on the pupil. Though there were trends that showed better vision from SF-CSCLR centration, there were too many other variables and factors for the results to reach statistical significance. Early uncorrected vision, though, suggested better vision trended with centering on the light reflex.”
If a surgeon is interested in trying this method of centration, Dr. Chang says the instrument most surgeons have that may let them do it is a placido disc corneal topographer. “I use the Atlas topographer, which has a coaxial fixation light in the center of the rings,” Dr. Chang says. “With other topographers, the manufacturer can verify if their fixation light is coaxial with their particular topographer’s camera. This would be your preop/postop reference point.” Intraoperatively, certain surgical microscopes have coaxial lighting, such as the Zeiss Lumera. “It has three lights, with the two smaller lights coaxial with the surgeon’s eyes,” Dr. Chang says.“So if you tell the patient to fixate on one of the two stereo coaxial lights, and you look through the ocular on the same side as that light, you have a patient-fixated, coaxially sighted, corneal light reflex. Then, you have an optical arrangement illuminating the eye in the exact same configuration that you did preop and postop; so you have a marker you can correlate preop, intraop and postop.” Dr. Chang says it’s worth checking with your microscope’s manufacturer to see if the fixation light and your viewing axis are truly coaxial.
The next step involves giving surgeons more opportunities to use this centration method, says Dr. Chang. “I’m trying to promote this concept to industry, so we can have more devices that make it easier for surgeons to utilize it,” he says.
The Other Half of the Story
Houston IOL and optics expert Jack Holladay, MD, MSEE, FACS, says that centering on something such as a corneal light reflex can be helpful with a multifocal lens, but leaves out an important second criterion for getting the sharpest vision.
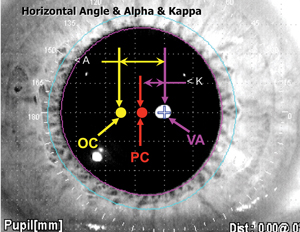
“For a diffractive multifocal lens to work properly, it requires two things, which usually produces a paradox,” explains Dr. Holladay. “First, it has to be lined up so the rays from the cornea are converging so the central ray that comes through the cornea goes through the center of, and is perpendicular to, the lens. In other words, picture two lenses along a common optical axis—they are lined up perfectly. However, when the IOL naturally centers in-the-bag and is aligned with the cornea on the optical axis, both are tilted about 5.2 degrees, called angle alpha, and decentered 0.6 mm temporal to the visual axis and 0.3 mm from the pupil center. This means the lens will always be tilted about 5 degrees relative to the visual axis, so the chief ray coming through the cornea that hits the center of the IOL is never perpendicular and the pencil of light rays never symmetrically converge from the cornea. Because these rays aren’t symmetrical and the chief ray isn’t perpendicular, they strike the microscopic diffractive edges of the IOL at angles for which they weren’t designed.
|
“The problem with moving the lens that far nasally, however, is it violates the second requirement of multifocal lenses,” Dr. Holladay continues. “The second requirement for diffractive optics is that the lens has to be concentric with the aperture, the pupil. The bifocal or trifocal diffractive optics are only balanced, or symmetrical, when the incoming pencil of rays, or wavefront, are symmetrical with respect to the diffractive rings. This only occurs when the diffractive rings are concentric with the pupil. The imbalance of the resulting diffractive pattern also causes additional light scatter and is additive to the first cause described above. So, unfortunately, it’s not possible to satisfy both criteria with the human eye, because the first Purkinje image is almost never centered on the pupil. It’s a paradox. The separation between the center of the pupil and the first Purkinje image is called angle kappa, and the best you can do is put the lens somewhere between these two points to minimize the additional light scatter and reduce complaints of haloes, glare and waxy vision.”
Dr. Holladay says that clinical studies analyzing multifocal IOL results in patients with varying sizes of angle kappa and decentration of the IOL relative to the pupil have confirmed these concepts clinically. “An article by Amar Agarwal and co-workers suggested that patients with large angle kappas—where the center of the pupil and the light reflex are far apart—actually end up with worse performance with diffractive multifocal lenses than patients with smaller angle kappas.1 A second article confirmed that large angle kappa and decentration of the IOL temporal to the pupil (and farther from the visual axis) were associated with the highest risk of poor outcomes with multifocal IOLs.”2 For the most successful outcomes with diffractive multifocal IOLs, Dr. Holladay recommends that at surgery the IOL be nudged nasally so the diffractive rings are located just nasal to being concentric with the pupil, between the pupil center and the Purkinje light reflex (if coaxial). Secondly, he recommends avoiding patients with large angle kappas (> 0.4 mm or 2.8 degrees when using a penlight or >5.2 degrees on the Orbscan II, which measures about two times larger values).3 “Following these two rules will avoid the majority of diffractive multifocal patients who are unhappy due to unnecessary glare,” Dr. Holladay says. REVIEW
1. Prakash G, Prakash DR, Agarwal A, Kumar DA, Agarwal A, Jacob S. Predictive factor and kappa angle analysis for visual satisfaction in patients with multifocal IOL implantation. Eye (Lond) 2011;25:9:1187-93.
2. Karhanová M, Marešová K, Pluhácek F, Mlcák P, Vlácil O, Sín M. The importance of angle kappa for centration of multifocal intraocular lenses. Cesk Slov Oftalmol 2013;69:2:64-8. [Article in Czech]
3. Basmak H, Sahin A, Yildirim N, Papakostas TD, Kanellopoulos AJ. Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg 2007;23:456–460.