“Any new surgical technique involves a learning curve, and complications will occur,” notes Ronald Yeoh, MD, medical director, founding partner and senior consulting ophthalmic surgeon at Eye & Retina Surgeons, Camden Medical Centre in Singapore. “The increasing trend towards femto-laser-assisted cataract surgery, or FLACS, means that we are encountering complications peculiar to this surgery. The transitioning surgeon needs to recognize these and modify surgical technique to manage them appropriately.”
Here, Dr. Yeoh and three other surgeons with extensive experience using femtosecond laser technology as part of cataract surgery share pearls taken from their experience with complications: what those potential complications are, how to manage them if they occur, and how to minimize the likelihood of them occurring in the first place.
Preoperative Precautions
For any surgery to succeed, appropriate patients must be chosen, and the patients must be made aware of possible postop concerns.
• Make sure the patient can lie flat and remain still. “There are some challenges that are unique to femtosecond cataract surgery—things that would not be a challenge in conventional surgery,” says Sonia H. Yoo, MD, professor of ophthalmology at the Bascom Palmer Eye Institute, University of Miami School of Medicine. “One is that the patient must have the ability to lie down flat in the right position and remain still.
|
“That’s true for several reasons,” she continues. “For one thing, most surgeons have the laser in a different room from the operating arena, so the patient has to get up and be transferred to the other room after the laser part of the procedure. Also, we need to have the patient’s cooperation during the laser, so that he can look at the light or adjust his position. With IV sedation on board, that might not be possible—the patient might fall asleep; his head might bob; he’s more likely to move at an inopportune time. As a result, we don’t sedate patients before the femtosecond laser part. So when you evaluate patients you need to make sure they’ll be able to lie flat and remain still.”
• Select cooperative patients with wide palpebral apertures. “As any LASIK surgeon knows, suction loss will create problems with flap creation,” says Dr. Yeoh. “When performing FLACS, suction loss can lead to incomplete capsulorhexes, incomplete nuclear division or incomplete incisions. Prevention is the best cure for this, so it is best to select patients with wide palpebral apertures who are cooperative.”
Dr. Yoo agrees. “If an individual has a very deep orbit or high brow, it can be difficult to dock the laser to the eye just because of the anatomy,” she says.
• Alert patients of the possibility of conjunctival redness. “This can result from the suction applied by the patient interface,” explains Zoltan Z. Nagy, MD, PhD, clinical professor of ophthalmology at Semmelweis University in Budapest, Hungary. (In 2008, Dr. Nagy performed the first- ever femtosecond-laser-assisted cataract surgery.) “This is more of an issue when the patient is on anticoagulant therapy, as many elderly patients are, so we need to ask patients about this before starting the procedure. It may be possible for them to stop the medication for a few days before the surgery, but if they cannot stop it because of cardiovascular problems, they should be informed of the possibility of postop conjunctival redness before the surgery. Usually, patients accept this as part of the surgery, so it’s not a problem.
“In most cases the redness goes away by the next day, or within a couple of days,” he adds. “Once in a while the redness lasts for a longer period, but only in patients who are on anticoagulant therapy. Fortunately, conjunctival redness is not as big a problem as it used to be [in our practice] because the new SoftFit patient interface on our LenSx machine allows us to use lower pressure.”
• During the preop examination, make sure the pupil dilates well with drops. “During conventional cataract surgery we’ve gotten pretty good at dealing with small pupils, using hooks and rings and intraocular mydriatics,” says Dr. Yoo. “A small pupil is also an issue with femtosecond laser cataract surgery, because if the pupil is too small we might not be able to use the laser. However, the usual aids may not be advisable in this situation. The problem isn’t so much having a drug or hooks or rings inside the eye; it’s that you have to make a wound to get them into the eye. When you use the laser you pressurize the eye, so if you’ve made any wounds you could lose the anterior chamber, putting the patient at risk. Admittedly, there have been some reports of surgeons placing hooks or rings or drugs in the eye and then cutting with the laser, but those are special cases.
|
“If you’re surprised on the day of the surgery by a pupil that you thought would dilate but for some reason doesn’t,” she adds, “one option is to simply not use the femtosecond laser. Another option would be to go ahead and make a wound and inject drugs or use hooks or rings prior to applying the laser, but you’d have to weigh the risks and benefits of doing so, because doing so may increase the patient’s risk of a complication.”
• An NSAID can help prevent femtosecond-laser-induced miosis. “Prostaglandins are released in the anterior chamber during the femtosecond laser step, causing pupillary constriction,” explains Dr. Yeoh. “Small pupils can cause the rest of the surgery to be more difficult. My publication in the latest issue of the Journal of Cataract and Refractive Surgery1 shows that a single application of a non-steroidal anti-inflammatory agent, used with the dilating drops an hour before surgery, is very useful in preventing femtosecond-laser-induced miosis.”
Working with the Laser
Surgeons offer these strategies for minimizing problems during the laser part of the procedure:
• When docking the patient, make sure the eye is flat to the plane of the patient interface and properly centered. “Making sure the eye is flat to the plane of the patient interface will minimize the relative tilt of the lens,” says Dr. Yoo. “If you have significant lens tilt, you may end up with an incomplete capsulotomy.”
“If you put the patient interface on correctly and in a centered manner, lots of complications can be avoided,” agrees Dr. Nagy. “If the patient interface of our LenSx machine is well-centered, for example, the information collected by the OCT is accurate, so it can define the lowest and highest points of the anterior capsule and avoid any piercing of the crystalline lens or incomplete capsulotomies. This has helped us achieve a free-floating capsulotomy 97 to 98 percent of the time.
“Good centration is especially important for creating the corneal wound,” he adds. “If the patient moves his eye and the interface is decentered, then the corneal wounds may be more central than expected, creating surgically induced astigmatism. The other possibility is that the wound could become too peripheral. It’s good to make the corneal incision as peripheral as possible, but if it’s too peripheral because of a decentered interface, it may hit the conjunctival vessels, which could lead to bleeding and an incomplete corneal incision. So centering the patient interface is very important.”
• If bubbles are present, undock and redock. “Imperforate incisions can result from poor docking, with air bubbles obstructing the incision site and poor positioning of the incisions,” notes Dr. Yeoh. “Good docking technique will help avoid trapped air bubbles.”
• Do everything possible to prevent suction loss during femtosecond application. Dr. Nagy notes that factors which can cause suction loss include loose conjunctiva and the patient moving or blinking while the laser is working. “If loose conjunctiva gets into the visual area, then the suction may not be secure, which could allow the interface to move during the treatment,” he says. “The surgeon should also remind the patient not to move or blink while the laser is working. If the patient moves his eye, it could break the suction. It’s rare for this to happen, but it is possible.”
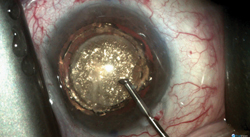
Dr. Yoo notes that suction loss isn’t always a big deal because you can often reapply or switch to manual surgery. However, suction loss can sometimes lead to trouble. “I did have one case where suction loss occurred during the lens segmentation and the segmentation pattern was briefly applied to the cornea because the laser is so fast,” she says. (See picture, above.) “There’s a safety mechanism on our laser that cuts it off once suction is lost, but I guess there’s a brief time during which you haven’t completely lost suction, and during that instant the laser energy was directed in the wrong plane. Fortunately, there were no visual consequences; the patient has done really well. You can see a waffle grid pattern in a section of the cornea—the same grid pattern the laser was making in the lens—but that area was not over the pupil, and the cornea was not cut or seriously damaged. I’ve been following the patient for about 18 months, and you can still see that pattern on the cornea. Other similar cases have been reported in the literature.
| ||||||
• If you lose suction, stop and proceed with manual surgery. Dr. Yoo notes that if the laser procedure is interrupted because of suction loss, most surgeons will just stop using the laser and complete the surgery by hand. “The only exception might be when the suction loss occurs while docking the laser prior to administering the laser,” she says. “In that case, surgeons typically try again. But once you’re depressing the foot pedal and the laser has started, if you lose suction you’re basically done with the laser part.”
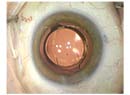
• Be careful when dealing with a liquefied cortex. “Generally, using the laser reduces complications when you’re dealing with a very dense lens,” says Dr. Yoo. “However, if you have a very dense lens and a liquefied cortex, such as a white cataract where the cortex is very liquid, you may get a plume of lens material once you open the capsule. That may actually block the lens segmentation.
“In those cases, you may want to increase the energy a bit on your laser when you’re doing the capsulotomy to make sure you cut through the fibrotic capsule and make sure the laser energy penetrates through small amounts of liquefied cortex that may escape during that capsulotomy,” she says. “Once you switch to manual surgery the viscoelastic will clear your view.
“Interestingly, because these lasers generate images of the lens once the patient is docked—most platforms use OCT imaging—sometimes you can actually see that the lens is dense but the surrounding cortex is liquefied,” she adds. (See example, right.) “In that case you should be prepared to take your foot off the pedal if you see liquid coming out during the capsulotomy.”
Managing the Capsulotomy
Once the laser portion of the operation is done, several potential problems unique to laser-assisted surgery need to be anticipated and addressed to ensure complication-free completion of the cataract surgery.
• Use a specially designed spatula to open the femtosecond-laser-created incision. “You can use any small instrument to open the femtosecond laser incisions,” notes Dr. Yeoh. “However, this is less than ideal, as size and shape are not optimized. Indeed, in the early days of FLACS, we used Sinskey hooks or cyclodialysis spatulae to open the incisions, but they were found wanting. The Slade Femtosecond Spatula works well; another option is the Yeoh Femto-incision Double Ended Spatula, which I designed but have no financial interest in. The latter is optimized in shape and angulation for use with these incisions.” (See picture, p. 34.)
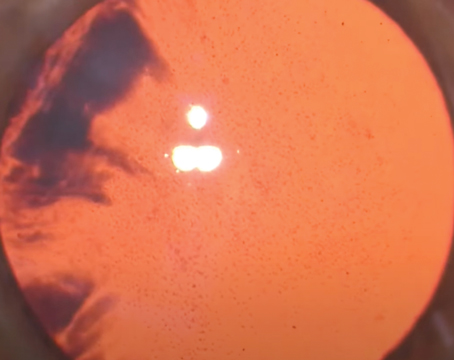
• Use viscoelastic to avoid missing an incomplete capsulotomy. “When using a femtosecond laser to create the capsulotomy, some areas can remain incompletely cut,” notes Robert Weinstock, MD, director of cataract and refractive surgery at the Eye Institute of West Florida in Largo, Fla. “By itself, an incomplete capsulotomy is not really a complication, because 99 percent of the time you can just grab the capsule with a forceps or microforceps and complete the capsulotomy without any problem. The problem occurs when you don’t realize that there’s an adhesion. If you grab the capsule quickly without paying attention and pull it out of the eye, it can rip at the point of adhesion and cause an anterior tear in the capsule, which then has a risk of running around posteriorly. So the way to prevent this complication is to pay close attention when removing the capsulotomy tissue.
“I find it helpful to put viscoelastic inside the eye before I attempt to remove a femtosecond-laser-created capsulotomy,” he continues. “That does two things. First, in many cases the process of making the capsulorhexis and breaking up the lens releases gas; those gas bubbles rise into the anterior chamber to the underside of the cornea where they interfere with the surgeon’s view. Putting in the viscoelastic pushes the gas bubbles out of the way so you can see what you’re doing.
| ||||||||||
• Watch for an oval bubble under the anterior capsule. “If the capsulotomy is not free-floating, there are some telltale signs you can see through the microscope,” says Dr. Nagy. “One is an oval bubble under the anterior capsule. If the bubble is oval you can be nearly certain there’s an incomplete cut in that area. The oval bubble will not appear every time you encounter an incomplete cut, but if it does appear, it’s a telltale sign that the capsulotomy may be incomplete. If the capsulotomy is incomplete, use your capsulotomy forceps to lift the tissue following the circular contour created by the laser. If you follow the contour you should avoid tearing the capsule 100 percent of the time.”
Removing the Nucleus
The way the laser creates the capsulotomy and fragments the nucleus is very different from a manual approach, resulting in some unique problems (and solutions) when it’s time to remove the crystalline lens from the bag.
• Pupil constriction. As already noted, one issue during femtosecond laser cataract surgery is that the pupil can come down. “The laser puts energy into the eye and—in my opinion—sets off a little inflammatory response,” explains Dr. Weinstock. “If you have a widely dilated pupil that’s away from the capsulotomy, usually you’re fine. But if you have a Flomax case, where the pupil is already predisposed to constriction during surgery, you’re at risk of the pupil coming down pretty quickly right after the laser treatment. For example, if you’re making a 6-mm capsulotomy and the pupil’s only at 7 or 7.5 mm, you will have enough room to do the capsulotomy, but the laser energy will be close to the pupil margin. That can trigger pupil constriction.
“To minimize the chances of pupil constriction in this situation, you want to do two things,” he continues. “First, get the patient under the microscope pretty quickly after performing the capsulotomy, probably within 15 minutes. Second, put a drop of a strong dilating agent such as 10% neo-synephrine in the eye right after the laser treatment. You should get good penetration with the drops, in part because you’ve pressed on the eye during the laser treatment, causing a tiny bit of epithelium breakdown.
“Because of the possibility of extra pupil constriction, we now routinely put in a strong dilating drop right after using the laser, before the patient goes under the microscope and is prepped and draped,” he adds. “We do this for all eyes, not just Flomax cases. Of course, there is a small risk that the drops will have a systemic effect, but patients are under monitored anesthesia, so if their blood pressure goes up they’re in a controlled environment. In any case, we haven’t seen any adverse complications from that addition to our protocol.”
• Be cautious when hydrodissecting and doing the cortical cleanup. Dr. Weinstock notes that hydrodissection and hydrolineation are a little harder to do during femtosecond laser cataract surgery. “We’re used to seeing a very good fluid wave when we do hydrodissection during manual cataract surgery, because when we peel off the capsule, usually the cortex is intact underneath,” he explains. “It’s very easy just to slip the irrigation tip into that space between the underside of the anterior capsule and the first layer of cortex. But when you do femtosecond laser surgery, the laser not only cuts the capsule, it goes down and cuts a rim of cortex too, the exact same size and shape as the capsulorhexis.
“The result is a kind of manhole cover effect,” he continues. “It makes a flush edge where you’re trying to hydrodissect. That makes it very hard to find the little space where you need to stick the cannula to get a true fluid wave between the capsule and the peripheral cortex. So instead of just doing this through one incision I find myself going in through my second incision and trying a different orientation. I find myself trying to puncture through the cortex and elevate it a little bit to get into that space. It doesn’t leave you a lot of room to grab cortex, and you have to go up underneath the iris. Because of this, when using femtosecond laser capsulotomy we’re not typically hydrodissecting as well as we have in the past.”
• Problems with gas buildup. Another potential complication with a femtosecond laser using a fragmentation pattern is that one of the by-products is gas buildup. “If gas is being created during the fragmentation, gas bubbles will accumulate inside the lens or behind the lens—and the greater the density of the lens, and the more fragmentation patterns you lay down in the lens, the greater the gas buildup,” notes Dr. Weinstock. “In theory, this will create increased tension inside the capsular bag.
“Early on, when people first started using femtosecond lasers for this purpose, there were several reports of nuclei dropping into the posterior segment,” he continues. “Many people believe these were caused by overly aggressive hydrodissection. Essentially, you’ve created pent-up pressure in the bag from the gas and then you’re adding fluid. In theory, you can blow the capsule open just from the pressure. For this reason it makes sense to titrate your hydrodissection when you perform femtosecond laser cataract surgery, and do it a little more slowly.”
“How much gas is formed depends on the energy we use and the spot size and spot separation parameters during the femtosecond pretreatment,” Dr. Nagy points out. “If a gas bubble forms within the crystalline lens, the surgeon should allow the gas to leave the eye through the anterior chamber and the corneal wound. I recommend the so-called “rock-and-roll” technique. This means that we perform a gentle hydrodissection and then move around the lens, pushing it down and back a little to allow the gas bubble to escape. If the surgeon does not do this and the hydrodissection is abrupt with a high-speed water jet, then there’s no chance for the gas bubble to escape. This can result in a rupture of the posterior capsule, the so-called capsular block syndrome.”
Dr. Weinstock also favors the rock-and-roll technique. “It helps to decompress the eye a little by rocking the lens a bit as you’re hydrodissecting,” he says. “Sometimes the gas will release and pop forward, relieving some of the pressure inside the capsular bag. For the same reason, I depress the wound and burp a little viscoelastic out of the eye before I hydrodissect to make sure the eye is a little soft as I’m doing it. Fortunately, I have not had any posterior rips from hydrodissection or hydrodelineation.”
Dr. Yoo notes that in her experience, capsular block syndrome is rare. Dr. Yeoh agrees. “With gentler hydrodissection after burping the gas out from the capsular bag,” he says, “there have been no more reports of dropped nuclei after FLACS.”
• Use a paddle prechopper to complete the nuclear division before emulsifying the nucleus. “FLACS can divide a nucleus up in many ways: cross; cylinder; grid; and so forth,” says Dr. Yeoh. “However, surgeons don’t always realize that femtosecond nuclear fragmentation leads to incompletely divided nuclei, which can be difficult to remove. There’s a 500- to 700-µm offset from the posterior capsule during nucleus fragmentation, so the posterior part of any nucleus is invariably going to be untreated and hence unseparated. Surgeons therefore need to adapt their technique to complete the nucleus separation.
“I recommend the use of a paddle prechopper to complete this nuclear division,” he says. “The paddle prechopper from ASICO (designed by me with no financial interest) is helpful in most cases. It’s simple to insert into the lasered grooves; then opening the prechopper completes the separation. After that, emulsification of the nucleus is straightforward.”
• Beware of unnoticed capsular tags when during irrigation/aspiration of cortex. “Current femtolasers have reduced the risk of incomplete capsulotomies to well under 5 percent,” says Dr. Yeoh. “Among the current instruments, AMO’s Catalys makes the capsulotomy the quickest, taking only about 1.5 seconds, which may further reduce the risk of incomplete capsulotomies. Nevertheless, the surgeon needs to make sure the femto-created capsulotomy is complete without tags, and he needs to take special care when doing irrigation/aspiration of cortex around the edge of the capsulotomy to make sure that a hidden capsular tag is not inadvertently aspirated, leading to a radial tear.”
Dr. Weinstock agrees. “It’s possible to engage the capsule by accident during cortical cleanup and damage it,” he notes. “Sometimes it’s easier to leave cortex behind, and that means potential complications down the road.”
• Do a careful sweep of the angle underneath the wound with your irrigation/aspiration tool. When a surgeon uses the laser to chop a lens into very small pieces, some pieces may be out of sight and difficult to find at the end of the removal process, causing them to be left behind. “Of course, this can also happen in manual surgery after emulsification of the lens,” Dr. Yoo notes.
| ||||||
Experience Counts
Perhaps the most important pearl for surgeons considering performing femtosecond laser cataract surgery is to expect a significant learning curve. “Capsular block syndrome was first described by an Australian group,” says Dr. Nagy. “They were early users of the femtosecond laser for this purpose, and they didn’t realize how much of a learning curve was involved. I think it takes 30 to 50 cases to become comfortable with this procedure and avoid most mistakes. Until reaching this point, the surgeon should be very cautious.”
Dr. Nagy believe that despite being associated with a few possible complications, femtosecond laser cataract surgery has many real advantages. “I think this technology helps to create consistent results, with a customized capsulotomy, customized corneal wounds and prefragmentation of the crystalline lens,” he says. “Now we’re using this technology up to Grade +4 cataracts. If a lens is white with a lot of water content, femtosecond laser capsulotomy is especially useful, reducing the risk of a peripheral tear and helping to avoid the so-called “Argentinean flag” sign—the spontaneous rupture of the anterior capsule due to high pressure within the crystalline lens. This technology is very good for trauma cases where there’s damage to the anterior capsule because of an injury, and also in pediatric cases because the pediatric anterior capsule is very elastic; a manual capsulotomy tends to end up much larger than you intended it to be. The laser also has great promise for other related surgeries, such as posterior capsulotomy.”
One thing is clear: While many surgeons remain skeptical of the value of femtosecond laser cataract surgery—especially given its price tag—it does appear to be here to stay. REVIEW
Dr. Nagy is a consultant to LenSx/Alcon. Dr. Yeoh is on Alcon and AMO’s speaker panels. Dr. Yoo is a consultant for Alcon and AMO. Dr. Weinstock has no financial interest in any product mentioned.
1. Yeoh R. Intraoperative miosis in femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2014;40:5:852-3. doi: 10.1016/j.jcrs.2014.02.026.