This leads to the question, when would a patient or doctor prefer to implant a monofocal toric lens over the ostensibly more advanced and multitasking presbyopic IOL option? In this article, we’ll delve into some of these reasons.
Mono- vs. Multifocal Torics
Despite the popularity of premium IOL options, experts say that there are plenty of reasons to recommend a monofocal toric rather than its premium counterpart.
• Coexisting conditions. Perhaps the largest limiting factor for toric multifocal lenses are patients who present with coexisting ocular pathologies. Dr. Miller describes some of the many pathologies that would make implanting a toric multifocal inappropriate. “You’ll see patients with amblyopia, epiretinal membranes, macular degeneration, macular edema, macular holes, macular schisis, vitreoretinal traction, advanced glaucoma, ocular misalignments, loose zonules, dry eye, basement membrane degeneration, et cetera,” he says. “There are a thousand-different corneal, retinal, optic nerve, and central pathologies that could result in a poor visual outcome if you implanted a multifocal lens. These comorbidities basically close the lid on multifocals, but they don’t close the lid on a monofocal toric to correct astigmatism.”
Cynthia Matossian, MD, an ophthalmologist based in Doylestown, Pennsylvania, also weighs in on the significance of these ocular pathologies. “One group of patients where I wouldn’t recommend a multifocal toric lens is those that have coexisting pathologies that affect the macula, retina and the optic nerve. If they have macular degeneration (typically early to moderate) with a strong family history, or if they have other kinds of macular diseases, as long as it’s not that progressive, I’d go with a monofocal,” she says. “They could have a macular hole or epiretinal membrane. Addressing these preop will absolutely help their astigmatism and outcomes, but they won’t do well with a multifocal because their vision is already compromised; giving them a clearer refractive option is great but splitting the light or adding potential light phenomena like starburst, halos or spiderwebbing will make things much worse. In this group of patients, where a lot of people fall, a monofocal toric is definitely the way to go.
“Glaucoma is also a big issue with multifocal toric lenses,” Dr. Matossian continues. “These patients have compromised optic nerves, so, implanting a multifocal toric in patients who are already having issues with depth of field is asking for trouble. They won’t do as well as they would with a monofocal toric.”
Robert Lehmann, MD, an ophthalmologist based in Nacogdoches, Texas, reaffirms the issues that arise when implanting a multifocal toric in patients with less-than-healthy eyes. “I don’t push multifocality—especially in patients who have glaucoma, Fuchs’ dystrophy, severe dry eye, et cetera. There are corneal issues where I wouldn’t want to use a multifocal lens because the results aren’t going to be good. If you’re dead-set on implanting a multifocal toric lens, ideally, the patient would have a virgin cornea. Outside of that, I would be hesitant to implant one over a monofocal to correct their astigmatism.”
When discussing where the Bausch + Lomb Trulign fits into this landscape, Dr. Lehmann says, “Typically, I consider the Trulign in much older patients, usually above 75 years old, because we don’t see as many issues with glare, halos or contrast sensitivity. But if you implant a multifocal and decrease their contrast sensitivity when they’re younger than that, you’re not doing them any favors because they might be at risk for a condition that will later on decrease their contrast sensitivity on top of that.”
• Level of astigmatism. Aside from the obvious red flags of ocular history and coexisting conditions, a patient’s level of astigmatism may also dictate whether or not a monofocal toric is more appropriate than a multifocal lens. “There is quite a bit of room for monofocal implants in our spectrum of patients scheduled for cataract surgery,” Dr. Matossian says. “A substantia
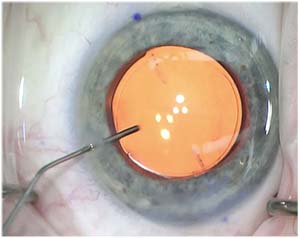 |
| When deciding to implant a monofocal lens, take into account patient preference. |
Dr. Miller specifies the issues involved when a patient’s corneal astigmatism exceeds the toric powers available. “You wouldn’t implant a multifocal lens in an eye with corneal astigmatism that exceeds the dioptric correction available in the marketplace. If you have a patient with 3.75 D of corneal astigmatism, industry simply doesn’t sell a lens at that toric power in the United States. So really there’s no choice—you would implant a monofocal toric instead.”
• Patient preferences. Despite the numerous medical reasons to choose a monofocal toric lens over its multifocal counterpart, sometimes, it’s up to the patient. “I see a lot of patients who have read things about how bad multifocals are,” Dr. Miller says.” They’ve read about the glare and halos or maybe they have friends who said, ‘I would never do this again,’ and so they decide they just don’t want a multifocal.
“You also encounter patients who have worn glasses or contact lenses all of their lives to correct astigmatism, and they would be delighted if all they had to do was wear reading glasses for near vision,” Dr. Miller continues. “If they’re fine with reading glasses, monofocal torics are the way to go.”
Dr. Lehmann also shares some of his insights into patients deciding to stick with a monofocal lens. “The patient that sits there and says, ‘I’m very happy with glasses,’ is a terrible candidate for these newer multifocal torics. We hear from some, ‘My grandchildren wouldn’t know who I was without my glasses,’ so they’re not likely to benefit from a multifocal.
“Occasionally, you’ll see people who are in a work environment where they wear glasses all the time and it doesn’t bother them. Again, a monofocal toric to correct their astigmatism is going to be better for their lifestyle,” Dr. Lehmann says. “What’s interesting is patients oftentimes begin the conversation by saying, ‘Well I’ve worn glasses for X years,’ and you can’t predict the other half of the sentence. Seventy percent say, ‘I’m content with glasses.’ The other 30 percent say, ‘I hate them! There’s a way to eliminate them?’ You just need to pay attention to their habits and lifestyles.”
In addition to the habits of patients, doctors may also need to take into account personalities to see if a patient is going to be satisfied with a multifocal toric. When asked about identifying patients whose personalities would benefit more from a monofocal toric, Dr. Matossian says it’s hard to pinpoint. “Some studies or authors say if someone is an extreme perfectionist, they may not do well with a multifocal,” she says. “They won’t be satisfied if they work under dim lighting conditions because a multifocal lens splits the light—about 40 percent to distance, 40 percent to near, and the rest is lost. So it’s not ideal for people who work in dim conditions. Invariably, they are going to have issues.
“Say you’re a limo or taxi driver,” she continues. “They’re not ideal multifocal candidates because of all the nighttime driving that comes with those occupations. They would benefit from a different lens because the monofocal toric would correct their astigmatism and help them see that much better.”
Dr. Lehmann agrees, adding that it can be difficult to pin down who would be a better monofocal toric candidate based on personality alone. “We tried to come up with an evaluation of some sort—a way to measure a patient’s psychology to predict which way the wind is blowing in their mind. I think we’re still flailing and failing, having not developed a psychology of multifocal lenses.”
Dr. Miller, however, finds that personality types don’t determine whether he implants a multifocal or toric monofocal lens. “I find that those cautions we used to hear, like ‘don’t implant engineers, don’t implant type-A personalities or whiny people, don’t implant pilots, et cetera,’ to be untrue,” he says. “The final word on happiness with multifocal implants is simple—it’s refractive error. If it’s significant, no matter how happy-go-lucky the patient, he or she is not going to be satisfied with the results. You don’t need to select based on personality type.”
Qualitative Issues
Despite the advancement of multifocal toric lenses, patients and doctors still keep the qualitative issues with these lenses in mind when deciding whether to use them.
“I would not implant a multifocal in people who are very prone or sensitive to halos, starbursts, spiderwebbing or any kind of light phenomenon because of their careers,” Dr. Matossian avers. “I’ll go with a monofocal toric because they won’t have the associated lighting issues. It still corrects their astigmatism without inducing any light phenomenon.”
In a 2016 study evaluating the efficacy of both multifocal and monofocal intraocular lenses after cataract extraction, researchers found that despite patients with a multifocal lens relying less on glasses, there were significant instances of halos and glare.1
In the realm of
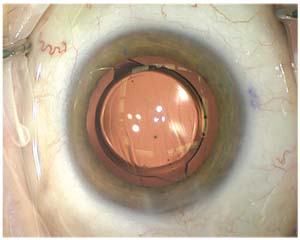 |
| The risk of qualitative vision issues may push patients toward monofocal torics. |
Financing
Another issue that might inform a patient’s decision to go with a monofocal toric is cost. “I’ve certainly recommended a monofocal lens over a multifocal because of cost,” Dr. Lehmann says. “You wouldn’t want a patient to feel that they’re getting second-best because they can’t afford this particular technology. You can still get the job done very well and get them results that they’re happy with using a monofocal. The technology we have now basically guarantees that a patient is receiving a reliable and effective treatment, and not getting the short end of the stick, so to speak.
“In any field there are technologies that cost more money, and if a patient is unable to afford those, obviously you can try to make it affordable with financing and other options,” Dr. Lehmann continues. “But I think it’s not a healthy thing to make a patient go with a multifocal they would struggle to afford when he’s going to see well with a monofocal and likely to be very pleased. I also don’t want them leaving the office feeling that they really settled for some kind of worse option because, frankly, that’s just not the case.”
Dr. Matossian also discusses her experience with financing issues regarding multifocal lenses. “Even though some patients have astigmatism,” she says, “they just don’t have the funds to pay for both a toric and simultaneously multifocal IOL because there’s a pricing difference. I would opt for a monofocal in that case.”
Despite the availability of multifocal toric lenses, doctors and patients are often opting to go with monofocal torics due to finances, personal preference and which lens will give them the best outcomes. “All together, these categories account for at least half, or maybe close to 65 percent of my practice,” Dr. Miller says. “I would say the toric multifocals are a small subset.” REVIEW
Dr. Miller is a consultant for Alcon and J&J Vision. Dr. Matossian is a consultant for Alcon and Bausch + Lomb. Dr. Lehmann is a consultant for Alcon.
1. Multifocal versus monofocal intraocular lenses after cataract extraction. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003169.pub4/abstract accessed 12 January 2018.
2. Summary of safety and effectiveness data (SSED). https://www.accessdata.fda.gov/cdrh_docs/pdf/P980040S065B.pdf accessed 8 February 2018.