One of the many challenges cataract surgeons sometimes face is weak or missing zonules, a situation that’s often associated with pseudoexfoliation. (We know that pseudoexfoliation not only affects the zonules, but can also infiltrate and affect the ciliary body; that combination can lead to zonulopathy.) Here, I’d like to share some of the strategies I use to minimize complications during surgery—and postoperatively—when working with such patients.
Searching for Warning Signs
One of the reasons zonular weakness is challenging is that it’s not always obvious before surgery that the problem exists. Sometimes the signs are subtle and easily missed at the slit lamp. For example, you may not notice a small amount of white fibrillar material on the iris or the anterior lens capsule.
In fact, if the problem is mild enough, it’s even possible to miss it during surgery. One study found that 70 percent of patients with subluxed IOLs, years after their cataract surgery, had pseudoexfoliation that wasn’t detected or reported in the notes made by the original surgeon. For these reasons, I take the advice offered by my former colleague, the late Alan Crandall, MD: Assume that every cataract surgery patient with a family history of glaucoma has pseudoexfoliation. (As I tell my residents, there’s no such thing as "routine" cataract surgery.)
During a routine examination you may find signs that a patient has a pseudoexfoliation issue. For example, you may note an unusual discrepancy, such as an asymmetry between the eyes in anterior chamber depth, or a hint of lens subluxation. Deposits of fibrillar material on the anterior lens capsule or sphincter are a giveaway, and phacodonesis or iridodonesis, poor dilation, abnormal lens or iris movements and a small pupil are other warning signs. Any discrepancy that can’t be explained should put you on the alert. In that situation you need to be prepared for possible trouble.
Perhaps even more important is any direct evidence of weakened zonules, especially at the lens equator. In particular, with dilation you may be able to see focal areas of invagination of the lens capsule. Whenever there’s focal weakening of the zonules—especially if there’s a loss of zonules—the capsule won’t be uniformly on stretch. The lack of stretch in one area will create a dip, and areas still under stretch may form a hump, creating a scalloped edge with hills and valleys. The valleys mark areas of zonular weakness or loss. This is a classic scalloped lens edge, and it indicates you’ll have a problem at the time of capsulorhexis.
Respecting the Zonules
In most cases of pseudoexfoliation, the surgery goes very well despite the problem. However, if you see a sudden deepening of the chamber, that indicates the presence of zonulopathy. That should kick in a whole set of strategies to minimize the chance of a potential adverse outcome.
The fact is, during cataract surgery it’s easy to make zonulopathy worse. Therefore, we need to take some essential precautions to avoid that. In essence, we need to minimize the stress we create in the x-axis or the y-axis by minimizing the side-to-side and up-and-down motion of the capsular-bag-zonular complex. This will avoid damaging the weakened zonules more than they’ve already been compromised. Accomplishing this involves maintaining a stable anterior chamber; doing a careful hydrodissection/delineation; using tangential forces during phaco and irrigation/aspiration rather than radial; and inserting and rotating the IOL slowly and carefully.
Here are some specific strategies that will help to protect the zonules:
• Be sure to widen a small pupil. It’s impossible to do a safe surgery if you can’t see well. (Of course, this is a problem you may face whether or not the patient has pseudoexfoliation or weak zonules.) You can use a cohesive viscoelastic of your choice to viscodilate the pupil; some surgeons recommend a push-pull technique using hooks to widen the opening. Some surgeons use scissors to make small micro-sphincterotomies that relax the pupil. Iris hooks or a device like the Malyugin Ring are other options. (If you use a Malyugin Ring, consider placing one of the circular scrolls right underneath your keratome incision; this can help to prevent the iris from exiting through the incision.)
• Make sure your capsulorhexis isn’t too large or too small. To help minimize stress forces in the x-axis, you need to have a capsulorhexis of adequate size—at least 5.5 mm. If the capsulorhexis is too large, you may not have the edge of the capsular tear sitting over the edge of the optic. If it’s too small, you can get phimosis and shrinkage over time, creating stress on the zonules at the equator and accelerating the zonulopathy 360 degrees.
A small capsulorhexis also makes it difficult to do the surgery in a way that reduces zonular stress during the operation. For example, if you can lift the endonucleus into the anterior chamber and phaco it there, rather than in the capsular bag, you’ll prevent all of the forces associated with phacoemulsification from impacting the zonules, but if the capsulorhexis is small, it'll be very hard to do this.
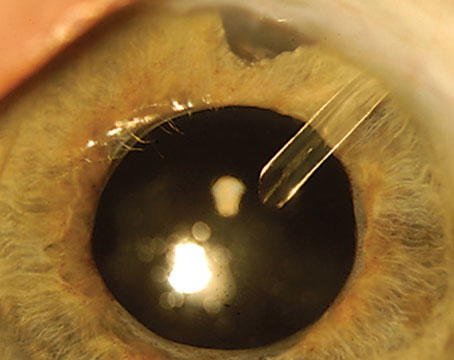
One strategy I find helpful when creating a capsulorhexis is to use the Microsurgical Technology (MST) forceps. They have ruler markings starting from the tip that can help the surgeon create an ideal-sized capsulorhexis opening by confirming the diameter of the capsulorhexis you’ve made. (See picture.) I measure it after I’ve created the capsulorhexis. If necessary, you can always enlarge it.
 |
| MST forceps with ruler markings can help a surgeon confirm the size of the capsulorhexis. (Note the Malyugin Ring scroll that's been placed directly beneath the keratome incision; this helps prevent iris herniation through the incision.) |
• Consider implanting a one-piece IOL. A one-piece IOL unfolds very slowly, without causing much tension; that gives you time to orient the haptics in the plane and axis you want. It’s very zonule-friendly. In contrast, the haptics of a three-piece lens open very rapidly; the lens pops out of the lens injector. I don’t have any evidence that a one- or three-piece lens will result in a better outcome in pseudoexfoliation, but they open differently. A one-piece lens gives you more control and thus may allow you to avoid zonular stress.
• Do a thorough hydrodissection and hydrodelineation. You don’t want to attempt to rotate the lens nucleus in the bag unless you have a complete separation of the capsular/zonular apparatus from the cataract itself; that’s why it’s very important to do a very good hydrodissection. Note: Having a fluid wave isn't sufficient to do a rotation. I tell residents: The goal is to direct that force of fluid to separate the nuclear material from the lens capsule at the equator.
I like to use the Chang cannula for this part of the surgery; it has a 90-degree-angled flat tip. Because of the cannula design, I can start doing the hydrodissection right underneath my keratome incision temporally, underneath the capsulorhexis edge and continue to irrigate going superiorly; then I do the same thing going in the other direction, again starting near the incision.
I also use the cannula to make sure the hydrodissection is complete. The distal point of the beveled tip can be used to impale and rotate the lens in the bag. Usually the hook is lying parallel to the plane of the cataract; I’ll rotate it 90 degrees and embed it into the cataract, and then rotate it. Once I get good rotation, I know I’ve separated the lens from the capsule/zonular complex.
• If you’re dealing with profound zonulopathy, do a viscodissection. That will not only separate the cataract but also elevate it out of the bag. If the cataract is soft enough, you can do a hydrodelineation to separate the nucleus from the epinuclear and cortical material, producing the ring sign. Then, because I’m right-handed, I go in with a flat instrument using my left hand, while I viscoelastic-elevate that piece into the chamber with my right hand. Next, I phacoemulsify the nucleus. Finally, I go after the remaining equinuclear and cortical material with additional viscodissection outside of the cortex.
• When sculpting, don’t push. Residents and glaucoma fellows often want to push the phaco handpiece into the cataract. Instead, let the phaco tip lead you. When you’re doing longitudinal phaco the device will clear the path for you, without pushing. Think of it as being like mowing the lawn with an automatic mower. The mower will pull you in the direction you’re cutting the grass. It’s leading you; you’re not pushing it.
If you do push while sculpting, you’re tugging on the zonules in the subincisional space, pushing the whole lens-zonular complex into the zonules 180 degrees away from you. You want to minimize that stress. So, let the phaco handpiece do its job. And once you’re done, don’t phaco coming backwards. That will minimize any damage to the corneal endothelium.
• Maintain a stable chamber. This is about minimizing the forces in the y-axis by preventing chamber shallowing or collapse. Strategies that can help accomplish this include:
— Make a 2- to 2.2-mm keratome incision. If you make the incision 2.4 mm or bigger, I believe the chamber will collapse no matter what you do. So make the incision snug around your phaco and irrigation/aspiration sleeve. You want a very controlled environment.
— Make your incision triplanar. I also tell residents, when you make your keratome incision, it can’t be biplanar. In the presence of zonulopathy, the lens and iris can shift. But if you make a nice 2.2-mm triplanar incision, nine out of 10 times the chamber will hardly shift at all.
— Avoid pressure changes when moving instruments in and out of the eye. I use my 27-ga. cannula to firmly inject BSS into the chamber while I simultaneously turn off the continuous irrigation in my phaco handpiece and gently pull it out, very slowly. This strategy achieves two things. First, because the irrigation is off, the iris won’t follow you out through the keratome incision. Second, the BSS will keep the chamber formed so you don’t get a trampoline effect and a sudden collapse of the anterior chamber, which could have a very problematic impact on the zonules. (Note: This strategy partly works because I use a 2.2-mm keratome incision.)
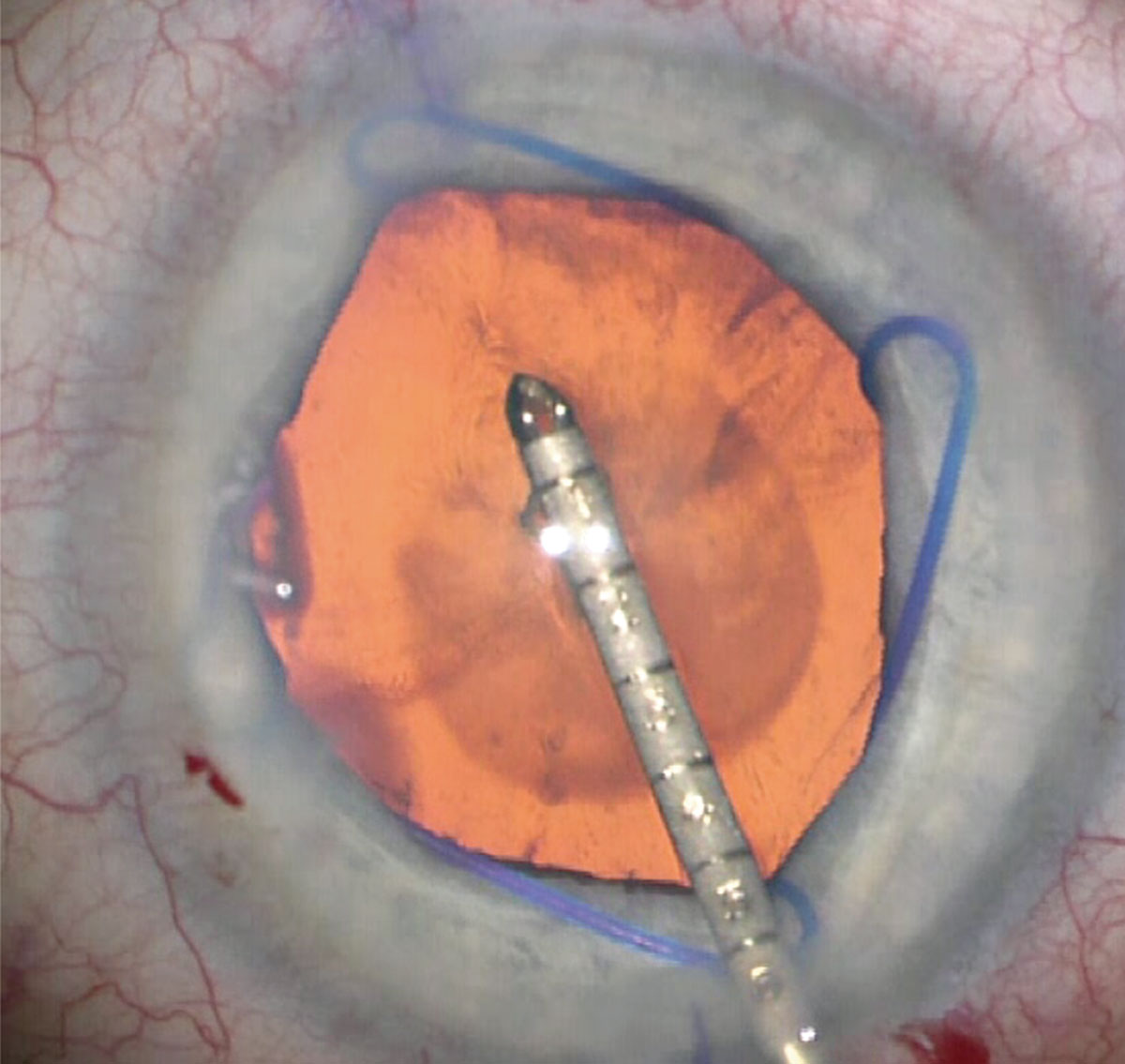
Another way to maintain a stable anterior chamber is to inject viscoelastic as you turn off the irrigation/aspiration. Once I have a stable chamber, I put my I/A handpiece in the eye; I remove the cortical and epinuclear plate, if there is any; I may even take out some of the debris underneath the anterior capsule that can contribute to phimosis. With my other hand I’ll go underneath the I/A tip while it’s still irrigating and then go underneath the edge of the capsulorhexis. (See image, above.) Then I fill the bag with viscoelastic while turning off the I/A. (If you leave it on, it will aspirate some of the viscoelastic.)
 |
| One way to maintain a stable anterior chamber is to inject viscoelastic as you turn off the irrigation/aspiration. Here, viscoelastic is injected into the capsular bag, causing a fluid wave; the I/A handpiece is kept in the eye with the irrigation off. |
I don’t want to remove the I/A handpiece during this process, because it could collapse the chamber. Instead, I leave it in, almost like an anterior chamber space maintainer. Once the whole bag is filled up, and the viscoelastic is bulging into the anterior chamber, I’ll gently take out the I/A handpiece and the chamber will be maintained.
• Peel tangentially, not radially. When I need to peel away cortex from the lens capsule, for example during the divide and conquer technique, I peel it in a tangential direction, like peeling the skin off an orange once you’ve cut it into pieces. When you pull radially, you’re pulling on the zonules. I’ll take my phaco handpiece and impale the desired piece without phacoing it, and then using vacuum, I peel the tissue back from an edge that’s already been hydrodissected. This minimizes damage to the zonules.
The tangential approach is critical, sweeping from one side to the other. I tell residents, go to the West Coast and walk to the East Coast and peel everything. In radial peeling, you’re going underneath the edge, grabbing a piece of cortical or nuclear material and pulling it to the center; that pulls directly on the zonules. Tangential peeling minimizes that.
• When rotating the cataract, consider using two instruments. If you use the divide-and-conquer technique, you want to make sure you’re rotating the whole lens before you start your sculpting; but rotating the material with one hand stresses the zonules significantly. Adding a second instrument to help the phaco handpiece do the rotation can eliminate most of the zonular stress. For example, push on one heminuclear piece while you pull on the other heminuclear piece in the opposite direction. This will help you maintain control inside the bag during the rotation and minimize the stress put on the zonules.
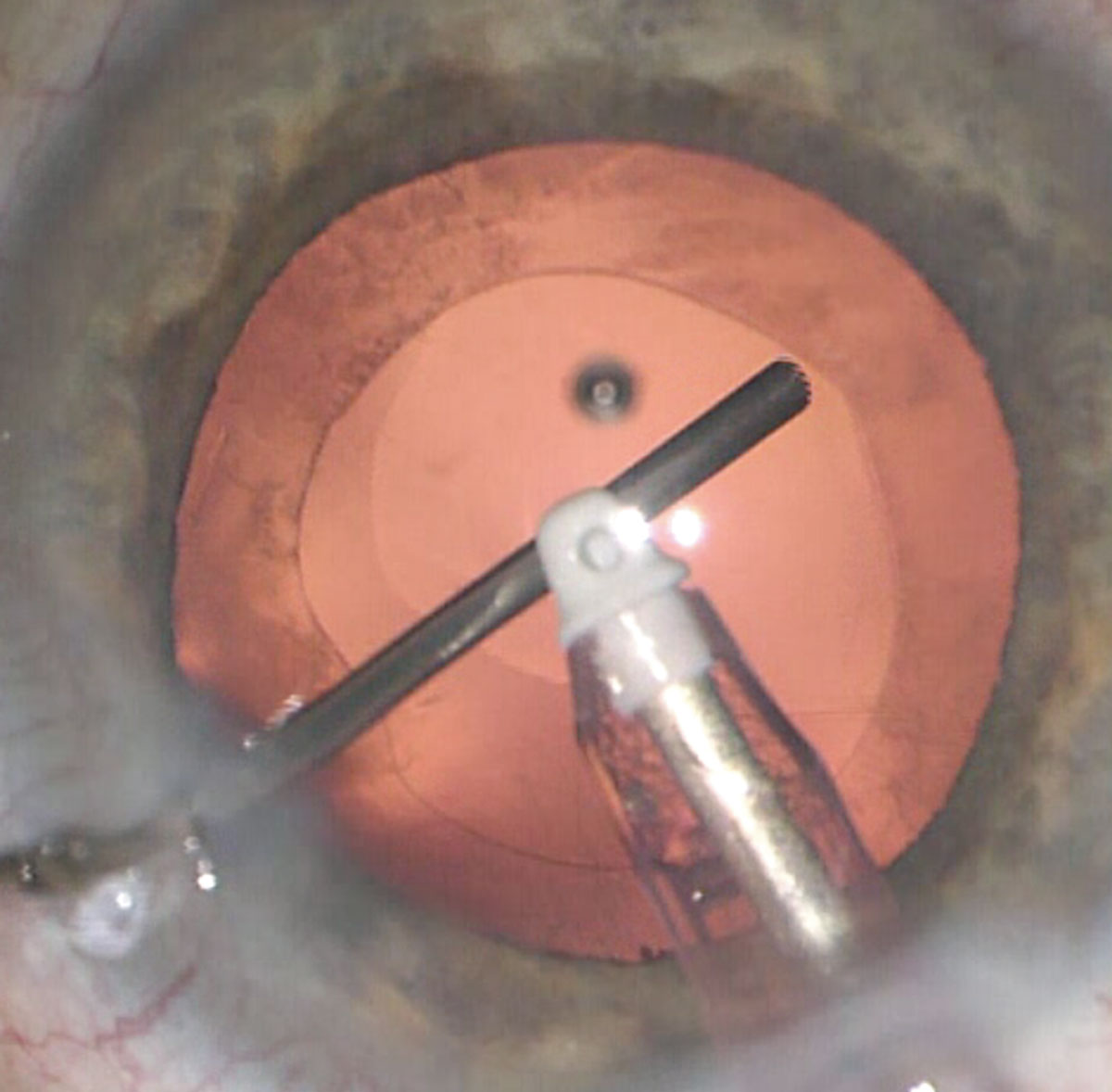
• If necessary, use iris hooks to stabilize the capsule during the surgery. Sometimes you may notice that the entire capsular bag complex is weak. In some patients there’s such significant zonulopathy that you can start a partial capsulorhexis and find yourself worried about the rest of the bag collapsing. In this situation you can use iris hooks to support the capsulorhexis itself (rather than the iris). That can minimize the y-axis stress while you do your phacoemulsification.
If you have more than three clock hours of weakness in the zonules, you’ll need multiple iris hooks to hold it up. It just depends on the extent of the zonulopathy. Later you can put in a support ring and suture it to the sclera; once that’s done, you take the hooks out.
Capsular Tension Rings and Segments
Capsular tension rings basically help with centration. So if you see that the capsular bag has shifted a little bit, but the shift is mild and the bag isn’t completely off-center, a CTR may solve the problem.
A few things to keep in mind:
• A CTR won’t prevent postoperative subluxation. It will help with centration at the time of cataract surgery, especially in patients with two or three clock hours of zonulopathy, but it won’t help prevent subsequent subluxation years later.
• A CTR won’t prevent postoperative phimosis. Whatever the mechanism of capsular phimosis is, a CTR doesn’t seem to counter it. So, it’s important to make a good 5.5-mm capsulorhexis.
• When you put the ring in, avoid any capsular laxity at the equator. Fill the capsular bag with cohesive viscoelastic. If it’s not fully inflated when you put the ring in, it can actually damage the zonules.
• Use a second instrument when delivering the CTR into the bag. This can help you manipulate the ring without stressing the zonules.
• Inject the CTR in the direction of the zonular laxity. This helps to avoid putting stress on the remaining zonules.
Even though the CTR won’t prevent late subluxation or dislocation, my retina colleagues tell me that if that IOL/capsular bag and CTR complex decides to take a dive onto the retina, having the ring in the bag will help them retrieve it. They can simply grab the edge and lift it up. The CTR keeps the capsular bag on stretch pretty much 360 degrees, making it easier to grasp.
If there’s a need for zonular support covering four or more clock hours during cataract surgery, a CTR typically isn’t going to suffice. In that situation a fixate-able capsular tension segment may be what you need. These segments have eyelets that can be used to secure them to the sclera. Often these segments only cover a few clock hours, as is the case with the Ahmed segment, but you can also use what’s called a modified Cionni Ring, which is a CTR, but with eyelets. (You can also fixate the capsule with multiple shorter segments. If you place one segment and see the whole bag tilt 180 degrees away from where you’re suturing the one eyelet, then putting in a second one in the opposite side makes sense.) Note that if you’re putting in a segment, it’s important to also place a CTR within the bag to uniformly stretch it.
The advantage of using a suture-able segment is that you can just slide the segment into the bag within the clock hours at which the laxity is present; the eyelet allows you to create two-point fixation to the sclera using a CV 8-0 Gore-Tex suture. The eyelet is designed to be above the plane of the arc, protruding upward and anterior outside of the capsulorhexis edge, so it’s accessible, while the curved CTR segment covering about 120 degrees sits inside the capsular bag in the lens equator to keep it on stretch. We simply make a little groove in the sclera, 1- or 1.5-mm posteriorly, and pass the sutures through the groove. We bury the knot in the groove, so we don’t need to make a flap.
This approach provides support where the zonules are missing, so the patient can have a well-centered IOL. (It also ensures that the lens won’t fall posteriorly later on.)
One other thing to keep in mind: The size of the CTR matters. CTRs come in multiple sizes, and getting the appropriate size is crucial to making sure the outward force created by the ring is appropriate for the eye. Depending on the axial length of the eye, the manufacturers make a recommendation of what size CTR to use.
In our practice we’ve created a table and posted it on the wall. It tells us the recommended CTR size that’s appropriate for a given eye's axial length. So when I’m in that situation, I have my IOL printout and ask the nurse, “What’s the axial length for this eye?” (I’ll visually confirm it as well.) Then the appropriate sized CTR is requested from the reference table.
Doing What We Can
Ironically, it’s difficult to assess the effectiveness of any preventive strategy we use, because clinical experience has shown that dislocation or subluxation of the capsulorhexis-IOL complex can take an average of eight and a half years to occur. That time lag makes it difficult to draw any firm conclusions about the effectiveness of our efforts. Nevertheless, it’s easy to do things during surgery that can worsen the problem. Thus, it’s crucial for us to do everything in our power to identify a potential issue and take steps to minimize the likelihood of postoperative complications.
Dr. Shareef is a professor at Case Western Reserve University/University Hospitals in Cleveland. He has no financial ties relevant to anything discussed in this article.