The Visian ICL
For the Staar Visian, surgeons say there are several stages of the lens measurement and implantation that are crucial.
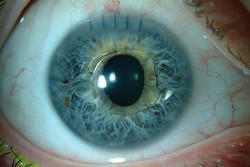
• Preop measurements. “The endothelial cell count is important for both [the Visian and the Verisyse],” says Majid Moshirfar, MD, director of refractive surgery and cornea for the Moran Eye Center at the University of Utah. “So the surgeon needs a good anterior chamber depth measurement. With the Visian, it is still a challenge to get an exact measurement of the sulcus-to-sulcus diameter, which is a key to its implantation. With the advent of high-frequency ultrasound, we have a better idea of what that measurement is behind the iris, but, despite that, you can’t control the amount of separation that will exist between the Visian and the anterior lens capsule, which should be a vault of between 250 and 500 µm. In some cases, you may find that the vault is good in the beginning but gradually decreases, or you may be surprised that the vault is a lot less than you anticipated. There are only four sizes of the Visian so, as a result, not every patient will fit perfectly into one of them, meaning you can’t control the lens vault.”
Dr. Moshirfar says there are a variety of ways to measure the sulcus-to-sulcus diameter, but he recommends ultrasound biomicroscopy if at all possible, and even has a certified ultrasonographer who does the measurement in each case to minimize variability. “If my patient’s anterior chamber is very deep—from 3.6 to 4 mm—and if I have a good sulcus-to-sulcus measurement, the Visian is a good option,” Dr. Moshirfar says. “But if I don’t have a solid sulcus-to-sulcus measurement I think the Verisyse would be a good choice.”
• Peripheral iridotomies. Dr. Moshirfar says that in some cases the Visian may float around a bit, making two preop iridotomies imperative. “With the Visian, you need to make your YAG PIs before the surgery, preferably one to three weeks prior,” says Dr. Moshirfar. “You need to make two PIs and make them peripheral enough so patients don’t have aberrations as a result of them, because in some cases patients can see the iridotomies as well as light distortions in the periphery, especially if they have large palpebral fissures and don’t have the superior brow or lid covering the superior iris. It’s very important that you put the PIs around the 10 o’clock or 11 o’clock positions, or at 1 o’clock and 2 o’clock. Try to avoid the 2:30, 3 o’clock, and 9 o’clock positions, which will cause patients to definitely see the PIs and the light coming through them. Sometimes, you even have to take the patient into the operating room and tattoo the cornea in those areas so they don’t see the light coming through the PIs.”
Minneapolis surgeon Sherman Reeves says that doing the PI ahead of time has a couple of benefits. “If I haven’t obtained a UBM, I can do it at that visit, too,” he says. “Also, though it’s uncommon, you can get some bleeding with an intraoperative surgical PI, so I like to keep the actual surgery as quiet as possible.”
• Folding and implantation. Dr. Moshirfar recommends using OcuCoat in conjunction with the Visian. “Mix the OcuCoat 50/50 with saline solution in the lens cartridge,” he says. “Make sure the lens is symmetrically folded and not torqued in the cartridge. And don’t put too much OcuCoat into the anterior chamber—use just enough so you can put your lens inside and behind the iris. As the lens unfolds in the chamber, be patient and inject it slowly so the first set of wings of the ICL can gradually open. Then, slowly tuck them beneath the nasal iris. As the lens unfolds, you can get the other two ends of the ICL under the temporal iris. Making sure that the patient is well-dilated is very helpful.
“Later, when doing I/A, don’t be overly aggressive,” Dr. Moshirfar adds. “This can create turbulence in the anterior chamber that can create transient anterior subcapsular vacuoles, and can cause some swelling in the anterior lens capsule’s epithelial cells, which could cause issues later.”
The Verisyse
The AMO Verisyse goes into the anterior chamber, so surgeons say its considerations differ from the posterior chamber Visian.
• Anterior chamber depth. Unlike the Visian, which relies on the sulcus-to-sulcus measurement, the anterior chamber depth and its vault size for proper results, surgeons say that the Verisyse is mainly dependent on the anterior chamber depth. “The key is you have to have an anterior chamber depth of at least 3.2 mm,” says Asim Piracha, MD, associate professor in ophthalmology and visual sciences at the University of Louisville. “A nice feature of the Pentacam HR is an Artisan/Verisyse preop calculation, that lets you make sure the eye has the normal anatomy for a Verisyse implant.
|
• Incision. While the Visian is foldable and goes through a temporal clear cornea incision, the Verisyse requires a 5.5 to 6 mm incision that’s not completely corneal: surgeons recommend limbal-corneal or scleral-limbal. Because the incision’s large, many surgeons prefer making it superiorly. “Most of these high myopes who receive the Verisyse have with-the-rule astigmatism or oblique astigmatism, so it makes sense to make a superior wound,” says Dr. Moshirfar. “That way, afterward when there is conjunctivalization of the cornea in that area, the vessels don’t look so red and patients don’t have the look of episcleral inflammation. The upper lid covers it up and it heals nicely.” Surgeons also recommend a nerve block in Verisyse patients to avoid issues from squeezing.
Managing sutures is also a part of the Verisyse surgery. “I make a limbal incision, make a groove, then create a nice step in the groove,” says Dr. Piracha. “I put one slipknot suture in the center of the wound after I put the lens in, which maintains the chamber so I can better work in it. This is important because these myopes often have floppy eyes and you worry about chamber collapse and the lens touching endothelium. I then perform enclavation [discussed below] and then pass the next two sutures and, before tying them, remove all the viscoelastic from the anterior chamber.” For viscoelastic, Dr. Piracha recommends a cohesive visco that comes out easier than a dispersive. “I don’t like a dispersive because it stays in the eye, is more difficult to remove and can cause pressure spikes.”
• Enclavation. This is a maneuver unique to the Verisyse that fixates it in place on the iris. To do it, the surgeon uses a special needle to bunch up bits of iris into small clips on either end of the lens. “If I do a superior incision, I do my nasal enclavation first because there’s less space on that side because the pupil tends to be more nasal, as well as superior,” says Dr. Piracha. “Then I do the temporal enclavation because I have more space. If I’m using a temporal incision—in cases of against-the-rule astigmatism—I do the superior enclavation first.”
Dr. Moshirfar says it pays to enclavate correctly the first time. “You really shouldn’t try to enclavate each side more than twice,” he says. “Even if the lens isn’t perfectly centered, don’t keep trying, because you’ll reach a point where the iris is traumatized and you won’t have enough iris for the enclavation. The best advice I can give is to mark the center of the pupil on the corneal surface and then place two tiny ink marks on the cornea corresponding to the spots on the iris where you will want to enclavate. This way, you can gauge your centration once you’re in the eye because, by that time, the pupil may be a different shape.” REVIEW