When
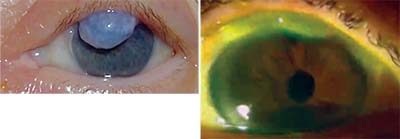 |
| In some cases an overriding bleb (above) will need revision prior to cataract surgery to reduce astigmatism and irritation and clear an obstructed visual axis. In other more subtle cases, such as one with bubble dysesthesia (right), a trabeculectomy revision would reduce the chronic pain symptoms associated with the bleb. |
Managing a Bleb
When the eye has an existing bleb:
• If the bleb is problematic, revise it before proceeding with cataract surgery. For example, a bleb overriding the pupil will need revision prior to cataract surgery in order to reduce astigmatism, reduce irritation and clear an obstructed visual axis. In other, more subtle cases, such as an eye with bubble dysesthesia, a trabeculectomy revision would help to reduce the chronic pain symptoms associated with the bleb. (See examples, below.)
• Test a thin, avascular bleb for leaks. If a Seidel test reveals leakage, the bleb will need to be revised to prevent hypotony, choroidals, corneal decompensation and possible
 |
| This thin, leaking bleb (left) was causing chronic hypotony and needed revision prior to cataract surgery. This thick, vascularized bleb (right) was associated with elevated pressure. After inserting the lens, I passed a 27-ga. needle across the anterior chamber, directed the needle tip through the prior sclerotomy site and separated the scarred-down tissue until I saw the bleb fill with aqueous. |
For example, a thin, leaking bleb (above, left) was causing chronic hypotony and needed revision prior to cataract surgery. I placed a drainage implant in the superotemporal quad-rant and directed the tube toward the prior iridectomy site, using a 30-ga. needle to assist with tube positioning. I stained the thin, leaking bleb with dye to verify that I’d re-moved all of the epithelial cells and then covered the old trabeculectomy with healthy conjunctival tissue. Once the pressure was controlled, I was able to safely proceed with the cataract surgery.
• Be careful to avoid overinflating a functioning bleb during hydrodissection. When performing surgery in the presence of a thin bleb, I use minimal infusion pressure to avoid distending and possibly rupturing the bleb. (Normal perfusion pressure can be used with thicker, more vascularized blebs.)
• If the bleb is thick and vascularized and pressure is elevated, modify the bleb during the cataract surgery. In a patient with a thick, vascularized bleb (above, right), after inserting the lens I passed a 27-ga. needle across the anterior cham-ber and used it to rejuvenate the scarred bleb. I directed the needle tip through the prior sclerotomy site and separated the scarred-down tissue until I saw the bleb fill with aqueous. (An ab externo needling procedure—entering under the conjunctiva—has also been described by others in the literature, with moderate success in improving bleb function.)
Working with a Tube Shunt
In eyes with a tube shunt:
• Look for hardware that’s close to exposure. Eyes with imminent hardware exposure due to a superficial ExPress shunt or a tube inserted too close to the limbus should be revised prior to cataract surgery to reduce the likelihood of hypotony and endophthalmitis. Correcting the exposure problem prior to cataract surgery will prevent postoperative complications. (A very thin patch graft can be covered with a new patch graft.)
• If a tube has
 |
| Eyes with imminent hardward exposure due to a superficial ExPress shunt (left), or a tube inserted too close to the limbus (right), should be revised prior to cataract surgery to reduce the likelihood of hypotony and endophthalmitis. |
 |
| Long tubes can be trimmed during cataract surgery to help protect the corneal endothelium from repeated mechanical trauma. |
To accomplish this, I recreated the fornix-based peritomy to expose the tube. I then constructed a new scleral tunnel adjacent to the existing tube using a bent 23-ga. needle and withdrew the tube from the original entry site and directed it into the new scleral tunnel. Because the tube was now following a more direct route, extra slack was created and I was able to reposition the tube farther into the anterior chamber. (There was no need to re-ligate the tube, since the bleb surrounding the tube remained intact.) Finally, I reapproximated the conjunctiva to the limbus using two running 7-0 vicryl sutures and verified the proper position of both the tube and the IOL. The combined surgery improved the patient’s vision, while also ensuring that the tube will continue to function properly.
• If a tube is too far into the anterior chamber, consider shortening it during cataract surgery. Trimming a long tube can help to protect the corneal endothelium from repeated mechanical trauma. In many cases I use microsurgical scissors to trim the tube after I insert the intraocular lens, prior to viscoelastic removal, although in some cases Bennett scissors may be the better tool to use. Once the tube has been trimmed, the cataract surgery can usually be completed using your standard technique.
Managing Uveitic Disease
Certain types of glaucoma require special care when performing cataract surgery. For example, in eyes with uveitic glaucoma:
• Preoperative inflammation control is essential. Eyes with uveitic glaucoma are prone to developing posterior synechiae and fibrin membranes that can occlude the pupil
 |
| Before cataract surgery, this glaucoma patient’s tube shunt barely entered the anterior chamber and was at risk for total occlusion. Left: At the conclusion of cataract surgery, after recreating the fornix-based peritomy to expose the tube, I constructed a new scleral tunnel using a bent 23-ga. needle, adjacent to the existing tube. I then withdrew the tube from the original entry site and directed it into the new scleral tunnel. Right: The more direct route provided extra slack, allowing the tube to protrude farther into the anterior chamber. The combined surgery improved the patient’s vision and helped ensure that the tube will continue to function properly. |
• If the eye has a tube shunt, consider temporarily plugging the tube during surgery. A tube plug can be used to reduce the likelihood of inflammation in uveitic glaucoma eyes that are at the greatest risk. I create a plug by tying a knot in a 4-mm segment of 3-0 prolene suture. I use Utrata forceps to gently guide the plug into the tube orifice; the plug prevents reflux of inflammatory mediators into the anterior chamber. I then complete the cataract surgery and the lens implantation using my usual technique. At the conclusion of the case, I remove the plug using the Utrata forceps.
• Consider augmenting the usual topical prednisolone and NSAIDs with subconjunctival and oral steroids. These will help control postoperative inflammation in uveitic glaucoma eyes.
Managing Glaucoma in General
The following strategies are helpful in all eyes that have glaucoma:
• Use plenty of dispersive viscoelastic to protect the corneal endothelium and maintain a deep anterior chamber. Many glaucoma patients have compromised endothelial cells due to years of exposure to topical glaucoma medications and elevated intraocular pressure. These endothelial cells may be more prone to damage from phacoemulsification energy.
• If you need to place iris hooks, avoid the tube insertion site or conjunctival bleb site. My tubes usually enter the anterior chamber near the 12 o’clock position. I position my superior hook to avoid ensnarling the tube tip with iris tissue, and place my temporal hook posterior to the cataract incision site. For eyes with a prior trabeculectomy, I avoid placing a hook through a functioning bleb.
• Ensure inflammation
 |
| Left: In eyes with uveitic glaucoma, preoperative inflammation control is essential to ensuring the best outcome. These eyes are prone to developing posterior synechiae and fibrin membranes that can occlude the pupil following cataract surgery. Right: In the most at-risk uveitic eyes that have a tube shunt, a tube plug can be used to reduce the likelihood of inflammation by preventing the reflux of inflammatory mediators into the anterior chamber. In this case I created a plug by tying a knot in a 4-mm segment of 3-0 prolene suture; I used the Utrata forceps to gently guide the plug into the tube orifice. I completed the cataract surgery and the lens implantation using my usual technique, and at the conclusion of the case I removed the plug using the Utrata forceps. |
• Take steps to prevent post-operative pressure spikes. Glaucomatous eyes usually have compromised outflow facility and are prone to pressure spikes, which are more harmful to a damaged nerve than a healthy one. Therefore, it’s very important to minimize the risk of postoperative pressure spikes by thoroughly removing all viscoelastic. Also, consider prescribing acetazolamide postoperatively.
Look Before You Leap
When formulating an operative plan for performing cataract surgery on a glaucoma patient with a pre-existing tube or trab, a thorough preoperative assessment of the patient’s corneal health—including pressure control and inflammation, as well as tube placement and/or bleb function—is essential. In some patients it may be necessary to “touch” that trab or tube prior to or during cataract surgery to insure a good postoperative result. By revising an imperfectly functioning tube shunt or trabeculectomy, you may avoid future complications and help the patient achieve an optimal visual outcome. REVIEW
Dr. Fechter practices at Eye Phy-sicians & Surgeons of Augusta. He has no financial disclosures relating to anything discussed in this article.



