 |
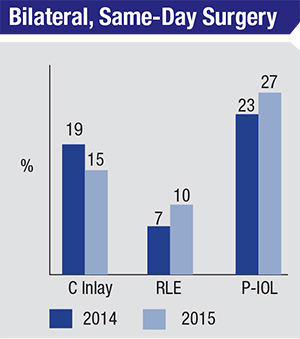
| Surgeons who are comfortable doing simultaneous, bilateral corneal inlays, refractive lens exchanges and phakic IOL procedures. |
Laser Refractive Surgery
A perennial topic of conversation surrounding LASIK and PRK is that of procedure volumes. This year’s survey showed a continuation of the trend in volumes flattening or even shrinking slightly.
This year, LASIK volume reported on the survey dropped 27 percent from last year, and PRK volume decreased by 7 percent. The ratio of PRK to the total number of laser vision correction procedures remained the same as last year at 28 percent. “Clearly, LASIK reached its peak around 2001,” says Dr. Duffey. “It’s been on a downward trend ever since. For the high-volume surgeon, at least, it’s really dwindled. The same is true for the surgeons reporting they do 25 cases per month and even five cases per month. Those groups too reached their peaks in 2001 and have been going down.” The percentage of surgeons reporting that they perform 25 or more cases of LASIK each month declined from 36 percent to 22 percent. Those doing five or more cases decreased slightly from 59 percent to 56 percent.
Interestingly, though volumes have gone down, surgeons’ confidence in LVC as a procedure class has gone up. Forty-four percent of respondents say they’d perform either PRK (15 percent) or LASIK (29 percent) on a high (-10 D) myope, compared to those who would prefer a phakic IOL (33 percent) or refractive lens exchange (4 percent). “It’s amazing to me that we’re still doing more LVC than lenses for -10 D myopes,” says Dr. Duffey. “It’s true in my practice, as well. Laser vision correction is just less complex and less risky than an intraocular procedure.”
On the hyperopic side, 61 percent of surgeons prefer LVC for a low hyperope (+3 D), vs. 17 percent who would prefer RLE. The situation flips for high hyperopes (+5 D), however, with 74 percent preferring RLE vs. just 8 percent who would do LVC.
In terms of flaps and residual stromal bed thickness, the latter has consistently increased on the study. “When we used to ask about how much stromal bed they would leave after making the LASIK flap, surgeons would often leave 250 to 225 µm,” recalls Dr. Duffey. “Now, it’s more commonly 275 and 300 µm. Similarly, when surgeons were asked the thinnest cornea on which they’d perform LASIK, they used to say it didn’t make a difference if it were 450, 480 or 520 µm. Now, many people aren’t comfortable unless the corneal thickness preop is 500 or 520 µm. I think we’ve gotten better at preop testing.”
Astigmatism Management
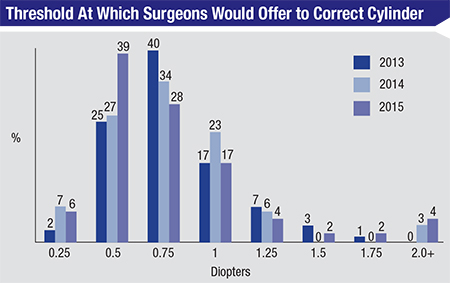
The survey also showed the trend of surgeons buying into the idea of refractive cataract surgery, where they try to provide sharp visual outcomes in addition to removing the cataract. This mainly manifests itself as their inclination to tackle astigmatism.
In 2012 for instance, only 17 percent of the survey’s respondents said they’d offer to correct 0.5 D of astigmatism. Today, however, 39 percent say they’d be willing to go after such a low amount. Overall, 73 percent of the surgeons will offer to correct astigmatism when it has reached 0.75 D; 6 percent will offer correction if it’s 0.25 D, 39 percent for 0.5 D and 28 percent for 0.75 D. By the time the level of a hypothetical patient’s cylinder is at 1.25 D, 94 percent of the surgeons surveyed will have offered to correct it. “A number of things influence this,” says Dr. Duffey. “As femtosecond technology becomes more available, it’s easy to just use it on a case. So, if you’re doing femtosecond on a cataract patient anyway, then you can just use it to correct whatever astigmatism is there. That’s certainly my approach. Speaking for myself, I have a lot of patients who come to me now because they know I’m able to get a lot of patients out of glasses, which I do because I make sure that I correct whatever astigmatism is present.
 |
Lens Surgery
One of the interesting facets of lens surgery that has emerged on the survey is the percentage of surgeons who are comfortable with performing simultaneous, bilateral lens surgery.
Last year, 7 percent of surgeons said they’d do bilateral RLE at the same visit, and 23 percent would perform bilateral phakic lens implantation. This year, 10 percent and 27 percent of surgeons are comfortable with bilateral, simultaneous RLE and phakic IOL surgery, respectively. “The perplexing part is, when I speak to surgeons, no one says he’s doing it,” says Dr. Duffey. “I know some insurance entities are making a push for bilateral, same-day surgery in California and Colorado, which could contribute to the increase. In general, I see the numbers go up each year but, anecdotally, I just don’t see people out there doing it.”
Due to a dwindling response rate, this marks the final ISRS refractive surgery survey, capping off a 19-year run of providing surgeons a barometer of the standard of care. Dr. Duffey says he appreciates what the survey has taught him. “You can see that the technology has gotten better and we’ve gotten smarter, learning from our mistakes,” he says. “We’ve shared data and have become better-educated. Meetings such as those held by the ISRS and ASCRS have helped us a lot, and I hope that these surveys also helped change the landscape and the standard of care thanks to what we’ve learned from each other.” REVIEW