 |
The survey, administered by Mobile, Ala., surgeon Richard Duffey and Palm Springs, Calif., ophthalmologist David Leaming, was e-mailed to 1,165 surgeons, and 561 of these physicians opened the survey. Of those who opened it, 112 (20 percent) responded. Here’s a look at the key results from this year’s ISRS refractive surgery survey.
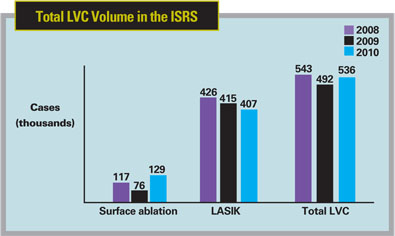
• LVC volume increases. As noted earlier, the volume of LVC procedures increased by 9 percentage points, with the proportion of total LVC volume represented by surface ablation increasing from 15 to 24 percent. Dr. Duffey says this increase in surface ablation procedures accounts for the overall increase in LVC volume, since estimated LASIK volumes actually decreased by a small amount, from 415,000 procedures on last year’s survey to 407,000 this year. “This is pointing out the conservative leanings of surgeons,” says Dr. Duffey. “We’re trying to make sure that we’re not overextending what LVC can do and perhaps run a higher risk of ectasia.”
• Femtosecond’s popularity is up. Three years ago, a little less than 30 percent of the survey’s respondents said they preferred to use a femtosecond laser to create flaps for LASIK. This year, however, that number stands at 55 percent, and also includes the newcomer to the market, the Ziemer Femto LDV (used by 5 percent of the respondents who prefer to use a femtosecond for flaps). “People trust the femtosecond laser more than they have in the past,” avers Dr. Duffey. “Also, residents in training are using it. The femtosecond laser companies have done a good job introducing the devices into university settings. That way, when surgeons leave their fellowships or residencies, they’ve been exposed to LVC and femtosecond lasers and don’t want to learn how to operate microkeratomes.” Dr. Duffey is quick to note that microkeratomes have made a lot of improvements over the years and that he still gets good results with his.
 |
• Corneal tissue concerns. In past surveys, at least half of the surgeons would say that a 250-µm residual stromal bed was adequate post-LASIK. On the current survey, however, only 45 percent think that 250-µm is the best amount to leave. “Now surgeons are starting to say that 275 µm or more is adequate, with this thickness now being chosen by 54 percent of them,” observes Dr. Duffey. “Also, 45 percent of surgeons prefer to use 100-µm flaps or thinner, which will yield more untouched corneal tissue in the bed.” In terms of ectasia, the percentage of surgeons who report ectasia cases isn’t growing. “Ectasia seems to be on the decline,” says Dr. Duffey.
 |
“The benefit of LVC is that there’s virtually no risk of cataract, retinal detachment, cystoid macular edema or endophthalmitis,” he adds.
Dr. Duffey says the real question for the surgeon is how comfortable he or she is with treating high myopia with LVC. “The ectasia-risk study published by Drs. Randleman and Stulting found there may be a little higher risk for ectasia in patients over -8 D, and that it may be little higher still in patients over -10 D,”1 says Dr. Duffey. “In this survey, however, with all other things being equal, 48 percent would choose LVC vs. 40 percent for a phakic IOL.”
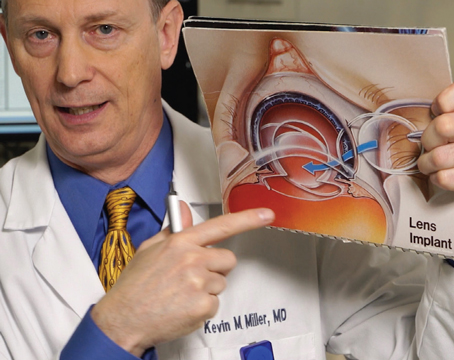
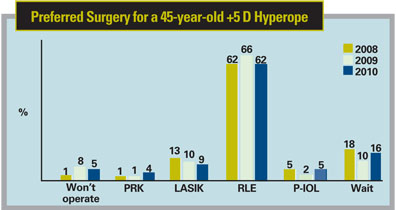
For the high hyperope (+5 D), however, the story is different, and LVC isn’t as attractive as a lens-based procedure. Sixty-two percent of surgeons say they’d perform refractive lens ex--change on such a patient, vs. only 13 percent who would perform LVC, even though the U.S. Food and Drug Administration has approved LVC for up to +6 D. “Some surgeons have found there are issues with regression of effect over time,” says Dr. Duffey. “There are also issues with perfect centering of the procedure.”
1. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology 2008;115:1:37-50.