As we’ve developed better techniques for managing regular astigmatism, such as toric intraocular lenses and better nomograms for limbal relaxing incisions, this has only intensified the importance of being able to parse out how much astigmatism is regular and how much is irregular. This is crucial, because we can confidently handle the regular portion of a patient’s astigmatism, but have to follow entirely different treatment paths for the irregular component. In this article, I’ll explain how I determine, roughly, how much irregular astigmatism a patient has, if any, and review treatment plans for common causes of irregularity.
Astigmatism Breakdown
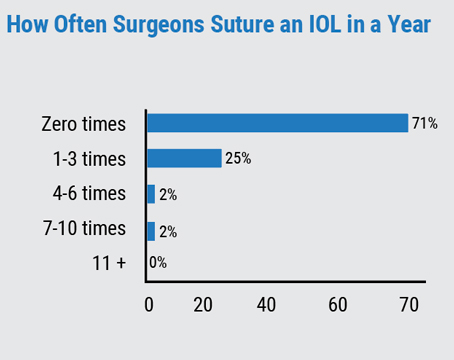
What started me thinking about irregular astigmatism is the fact that I’ve had an increasing number of patients referred to me because of complaints after toric IOL implantation. It turns out most of these referrals are due to irregular astigmatism that was missed before the implant surgery, or increased after the implant surgery, and which the toric lenses can’t correct.
Everyone has some component of both regular and irregular astigmatism, but the key to success with the toric lens is gauging the magnitude of each. For instance, if a patient has about 90 percent regular astigmatism and 10 percent irregular, chances are he’ll be OK with a toric IOL. However, if it’s more like 30 percent irregular and 70 percent regular, and you feel that the patient will desire correction of the former, that’s a situation in which it’s better to try and find a modality that can deal with both, rather than perform two separate procedures.
To try to get a general sense of the magnitude of any irregular astigmatism present, a good test for many patients is to determine the difference between their spectacle acuity and their contact lens acuity. Another way is to evaluate tests for corneal irregularity such as corneal topography, and compare this with the patient’s best corrected vision and other pathology present in the eye. Here are several common scenarios:
• Astigmatism with no other pathology. For example, if the patient only has regular astigmatism, when you put spectacles on him he’ll say his vision is great, and he’ll be happy with the correction. However, if the same patient has a significant amount of irregular astigmatism, when you put the glasses front of him, the vision won’t look very good. He’ll say it seems “distorted” or “shadowy.” However, when you then put a set of rigid gas permeable contact lenses on him, the vision will be great. In order for the process to work, the irregular astigmatism has to be in the cornea, without any other pathology that can distort vision.
• Astigmatism and cataract. Having a cataract present makes this process harder. You can first get a sense of the degree of regular and irregular astigmatism from topography, but the other tests will be difficult to interpret. For instance, the vision will be bad in spectacles, but this could be due to either the cataract or the irregular astigmatism. Even in RGPs, the vision will be better than in glasses, but will still be bad, due to the cataract.
 In such cases, history is helpful. For example, the patient may have some irregular astigmatism that’s been present for a while, such as someone who had LASIK 10 years ago and who has a mildly decentered ablation. He’s been content with his vision up until the past two years, when the cataract developed. In this case, the irregular astigmatism is a minor component and the unsatisfactory vision is mostly due to the cataract. The best treatment path would be to remove the cataract, place the implant, and take the patient’s vision to where it was 10 years ago.
In such cases, history is helpful. For example, the patient may have some irregular astigmatism that’s been present for a while, such as someone who had LASIK 10 years ago and who has a mildly decentered ablation. He’s been content with his vision up until the past two years, when the cataract developed. In this case, the irregular astigmatism is a minor component and the unsatisfactory vision is mostly due to the cataract. The best treatment path would be to remove the cataract, place the implant, and take the patient’s vision to where it was 10 years ago.
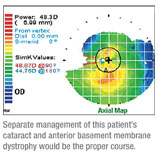
• Cataract and anterior basement membrane dystrophy. Here, in the typical case, the patient will present with poor vision and astigmatism that’s part regular and part irregular as well as a cataract and ABMD. She’ll say her vision has gotten worse over the past five years or so, which leaves you wondering which aspect got worse: the cataract; the regular astigmatism or the irregular astigmatism. In this case, it’s a judgment call, with a lot of help from topography, to determine whether she’ll benefit from regular cataract surgery and phototherapeutic keratectomy later for the irregularity from the ABMD, or whether the ABMD and the amount of irregular astigmatism was small but instead she had relatively high pre-existing regular astigmatism. In such a case, you have to do a careful analysis of the topographical aspects of it, because you can’t depend on other tests like refraction or RGP lenses because of the presence of the cataract.
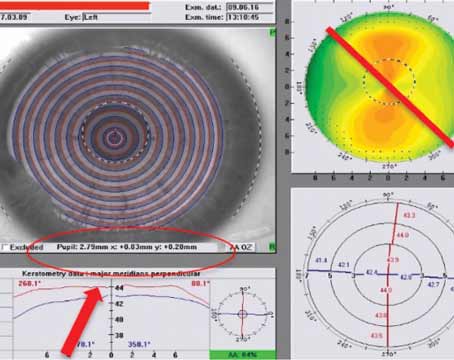
• Irregularity post-laser vision correction. One challenge with an irregular cornea after LASIK is determining if the visual problem is due to keratoconus, a decentered ablation or ectasia. In such a case, you really have to depend on an analysis of the posterior cornea and regional thicknesses. If the patient has inferior steepening, the question is whether the ablation was high, leading to the inferior portion being more myopic because it didn’t get enough laser energy, or whether the patient actually developed ectasia, causing the inferior cornea to be weaker, steeper, thinner and protruding. In clear-cut cases of ectasia or keratoconus, you’ll find a thin area where the cornea is also steep or, in cases of decentration, you’ll discover the cornea was thinner superiorly—where more tissue was taken off—even though it’s steeper inferiorly. However, there are some cases in which it’s difficult to tell. In such cases, in addition to careful use of Pentacam, Orbscan and/or regional optical coherence tomography, the one test you can use is time: Decentrations tend to get better with time because the epithelium fills in, while keratoconus and ectasia may worsen. However, not everyone progresses over time.
Treatment Pathways
Though irregular astigmatism is best treated on a case-by-case basis, here are techniques for treating particular causes.
• Anterior basement membrane dystrophy. The method I prefer for ABMD is PTK, because it leaves a smooth cornea. In this treatment, I manually remove as much residual basement membrane material as I can with a blunt PRK spatula. Then, I use the excimer to take off 4 to 5 µm of tissue across the cornea. For this treatment, I dry the cornea, and then use a 6-mm broad-beam laser centered on the pupil, and treat with 15 to 20 pulses. I then dry the cornea where likely I won’t see any significant residual basement membrane in the center. After that, I’ll move to the peripheral cornea, especially if the patient has symptoms of recurrent erosion. In the periphery, I center the laser on the limbus and move slowly around the peripheral cornea to try to remove 4 to 5 µm of tissue in all areas of the cornea. As I go, I dry the cornea to check for residual patches of basement membrane material in those stubborn areas. If I see an area with thickened material I might take off a couple extra microns there.
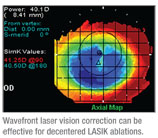
 • LVC decentration. For the most part, the wavefront correction of an excimer laser can adequately treat most of the decentered ablations that resulted from standard treatments done years ago. In such cases, it’s a matter of capturing the wavefront that appears to be similar to what you see on topography, where the refraction matches relatively well, and what the patient is complaining of symptomatically. If you can get a reasonable match, you’ll be able to determine if the wavefront ablation will improve the problem.
• LVC decentration. For the most part, the wavefront correction of an excimer laser can adequately treat most of the decentered ablations that resulted from standard treatments done years ago. In such cases, it’s a matter of capturing the wavefront that appears to be similar to what you see on topography, where the refraction matches relatively well, and what the patient is complaining of symptomatically. If you can get a reasonable match, you’ll be able to determine if the wavefront ablation will improve the problem.
Mild decentrations often respond well to wavefront ablation, but severe decentrations can be harder to improve to a point where the patient is happy.
Though irregular astigmatism can pose a unique challenge, a careful evaluation of each patient’s unique astigmatic situation will often lead to a satisfactory treatment.
Dr. Hardten is an adjunct associate professor of ophthalmology at the University of Minnesota Department of Ophthalmology. He consults for AMO and Alcon. He has done research for Avedro and Topcon, and has done speaking for Carl Zeiss Meditec.