Though the femtosecond laser does a very good job of making reproducible flaps, surgeons who use it always appreciate one or two extra tips to help them make flaps with even fewer mishaps or complications. In this article, refractive surgeons experienced in the use of the device share their insights on how to get the best results.
Machine Settings
Northwestern University Feinberg School of Medicine’s Surendra Basti, MD, who has taught femtosecond courses at meetings of the American Society of Cataract and Refractive Surgery, says that, though the advice to “know your machine” sounds generic, it’s a rule every surgeon needs to follow.
“In terms of getting good flaps, setting the machine so that it creates reproducible flaps is key,” Dr. Basti says. “However, every machine is different, so you have to see what results you’re getting with your machine and adjust based on that.” Trevor Woodhams, MD, of Atlanta, says one of the keys to good surgery is “finding best trade-off between speed of the treatment and the ease of peeling off the flap.” In this vein, surgeons note that the machine’s spot/line separation has to be of a certain value in order for the flaps to be easy to lift. “For the laser to create a smooth flap, it provides energy in small spots, placed in lines. The laser delivers many of these lines of spots,” says Dr. Basti. “The space between the spots and the lines doesn’t get laser energy, and is therefore a barrier to lifting the flap. If you’re having difficulty lifting the flap, you should first change the spot/line separation, because placing them closer together will accomplish the goal of decreasing the area not receiving laser energy. For our machine, the optimal spot/line separation is 9 x 9.
“However, one situation where power is the cause of an undesirable event is if you’re experiencing a lot of diffuse lamellar keratitis, especially near the edge of the flap,” adds Dr. Basti. “If you’re getting frequent DLK, the first adjustment you should make is to decrease the power.”
Suction and Applanation
Vancouver, Wash., surgeon Brian Will says that vacuum problems have become much less frequent with modern femtosecond lasers. “However, the surgeon can have an adverse effect on holding vacuum if he torques the vacuum ring,” he notes. To apply the ring, Dr. Will prefers to use a two-handed method while wearing his reading glasses—he’s presbyopic—rather than looking through the microscope. “For me, this is faster and it’s less stressful for the patient,” he says. “The key is putting it over the center of the pupil. The vacuum ring has crosshatched marks; you can use those as a frame of reference and put the pupil in the center of the crosshair.
“Occasionally, you’ll encounter eyes where the pupil isn’t in the center of the cornea or the eye has a lot of astigmatism,” Dr. Will continues. “That can be problematic in getting good centration. Once the vacuum has been applied and you’re not happy with the positioning, release the vacuum and reposition the vacuum ring.”
To get good suction, Fort Worth surgeon Phillips Kirk Labor uses what’s known as the “unclip technique.” He explains it this way: “When you first put the suction ring on the eye under the optics of your microscope, decenter the ring slightly superonasally,” he says. “You should see a little bit of the sclera inside the suction ring. Then draw suction and swivel the bed underneath the IntraLase. Bring the docking mechanism down into the ring, using the light reflex on the monitor to align the cone. Come down until the IntraLase tells you have good applanation, but then z down a little more, to make sure you’ve got good applanation. Then, unclip the suction ring and that will allow it to achieve suction perfectly.”
There may also be occasions in which the patient has a narrow fissure that makes it challenging to seat the vacuum ring. “In some cases a lid speculum can be helpful if you have a lot of squeezing, but sometimes not. I’ve also found that a 4 x 4 piece of gauze can help you get some purchase on the lid,” explains Dr. Will. “With the gauze, you can get enough traction on the lid itself in order to get the vacuum ring into the eye. The gauze everts the lid almost like when you have to remove a tire from a bicycle rim; you just have to work at it. With this technique, there have only been a couple of patients in whom I couldn’t fit the ring in well over 20,000 cases.”
 |
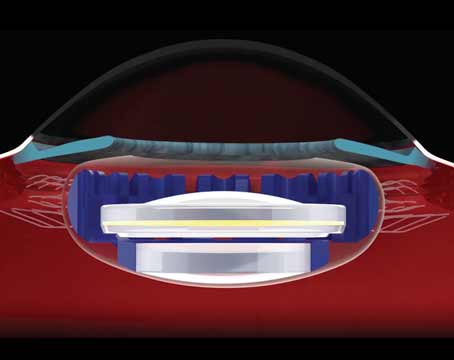
| Attempting to create a flat that encroaches on the limbus may allow expanding gas to flow retrograde into the episcleral vasculature and accumulate in the anterior chamber. |
These are two intraoperative complications that are mostly avoidable with the right preparation, surgeons say.
“Gas under the epithelium often occurs in patients with small, superficial cornea scars,” says Dr. Basti. “To avoid it, be careful with case selection. For instance, if you have a patient who has such a scar, you’ll want to discuss with him the possibility of air collecting under the epithelium in the region of the scar. If you want to completely avoid air collecting under the epithelium, then do PRK. If you do encounter gas in the epithelium after using the femtosecond, give it 15 to 20 minutes and the gas will resorb.”
The opaque bubble layer, or bubbles that occasionally appear in the intrastromal interface, can interfere with excimer laser ablation and tracking. “I created the partial docking technique to decrease the chances of getting OBL,” says Dr. Will. “With the partial-meniscus docking technique, I leave part of the peripheral cornea uncompressed. This lets the initial pulses of the femtosecond laser start right at the very edge of my docking meniscus, to allow the gas to dissect toward the limbus.” Dr. Will also uses a relatively small “pocket,” the space that the laser creates to allow the gases to escape. His pocket is 0.1 mm. “The advantage of a smaller pocket is that it lets you cut larger flaps,” he says. “This is due to how the software works. The galvo mirrors can only move so far in one direction, and if you use up a portion of that ‘quota’ with your pocket, then you’ve reduced the overall flap diameter you can create. For example, if 10 mm is the maximum flap diameter that the galvo mirrors can make, and you made a 0.4-mm pocket, then the biggest flap you could make would be 9.6 mm.”
 |
| An opaque bubble layer occurs when expanding gas fractures the cornea. It occurs with improper corneal applanation technique. |
The surgeons also have general advice for different stages of LASIK.
During the procedure, the suction ring can induce subconjunctival hemorrhages, but Dr. Basti says these can be prevented. “We instill a drop of either Naphcon A or Vasocon A 10 minutes before the flap creation procedure,” says Dr. Basti. “This has significantly decreased the incidence of subconjunctival hemorrhage.”
Dr. Will says if a flap tears during lifting, don’t panic. “If it just has a tear, continue to lift the flap,” he says. “Treat the patient normally, put the flap back down, and the patient will do fine. Don’t cut it off and discard it, since you can always do that later if necessary.”
“It’s key to be able to recognize the difference between a postop keratome flap and a postop femtosecond flap,” says Dr. Woodhams. “For example, in a femtosecond flap, the edge of the flap will be more opaque and defined, especially on the first postop day, when compared to a microkeratome flap. There will also be a kind of peau d’orange appearance to the femtosecond flap interface that’s quite different from the interface of a flap created by a keratome.”
Ultimately, surgeons say knowing your laser, getting a feel for the right parameters and planning ahead to avoid potential problems can make for good, reproducible flaps.