Patients with damaged or congenitally malformed irises can suffer from myriad conditions: severe photophobia; reduced vision; halo; and glare. However, newer surgical techniques and the advent of lifelike artificial irises can give these patients new leases on life. Here, experienced surgeons discuss the ways they approach these sometimes challenging cases.
Surveying the Damage
According to Michael E. Snyder, MD, who is in practice at Cincinnati Eye Institute, the first consideration when choosing between these treatment options is to assess the amount and type of iris damage. “Small defects are more easily repaired than larger defects,” he says. “We also look at the quality of the remaining iris tissue. If there’s a traumatic injury and only a small amount of iris tissue is lost out of the wound and the remaining iris tissue is normal, that’s a pretty straightforward repair. If a lot of tissue is lost and/or the remaining iris is of poor quality, then it’s much harder to repair, and an artificial iris may be needed,” he says. Assessing both the iris stromal tissue and the degree of iris pigment epithelial loss is similarly important. If residual iris tissue has marked transillumination defects, the eye might look okay after a repair, but the patient may still be profoundly photophobic.
Recently, Dr. Snyder has also started considering patient age in the treatment decision. “That’s another piece of the puzzle. I’m seeing some patients now who had their irises repaired using a cerclage suture a decade or two ago. A number of these patients are reappearing because the suture material has cheese-wired through the natural iris tissue. Then, the question about suture repair or prosthesis use includes whether the patient has a long horizon or, perhaps, a shorter horizon,” he adds.
An additional factor is the status of the natural lens. “In a patient who has a normal, clear crystalline lens, we often try to defer doing anything surgically in the anterior segment. We can’t put an iris prosthesis into a patient who has a natural lens still in place, and if we do a repair in the presence of a clear, normal crystalline lens, we might induce a cataract. In these cases, we might be much more conservative and try to manage the situation with optical means, like tinted specs or opaque periphery contact lenses as best possible. If patients have a cataract or a lens implant in place and a larger defect or poor quality of the residual remaining iris tissue, then a prosthesis becomes a wiser choice,” he explains.
Dr. Snyder also stresses the importance of realistic patient expectations. “When we’re doing iris repair or prostheses, the pupillary opening is a fixed size, usually about the size of the average pupil in normal indoor room lighting. It doesn’t expand; it doesn’t contract. So, in very dim lighting, it might be a little smaller than the fellow eye. In very bright lighting, it might be a little bigger than the fellow eye. The devices are custom-made so that they look much like the picture that we sent to [the company] of the fellow eye, and the matches are pretty good, but not perfect. I always tell my patients that the matches are like a cocktail-party match, meaning that with cocktail-party lighting and cocktail-party distance, it looks pretty good—especially after a cocktail,” he says.
 |
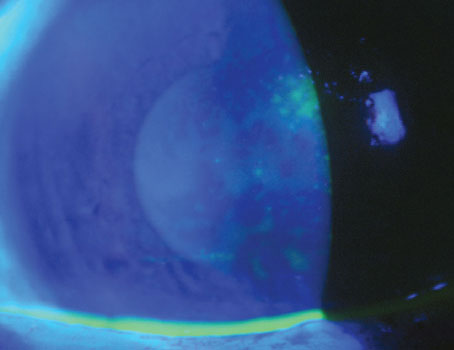
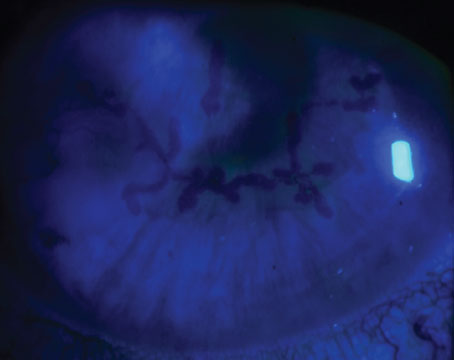
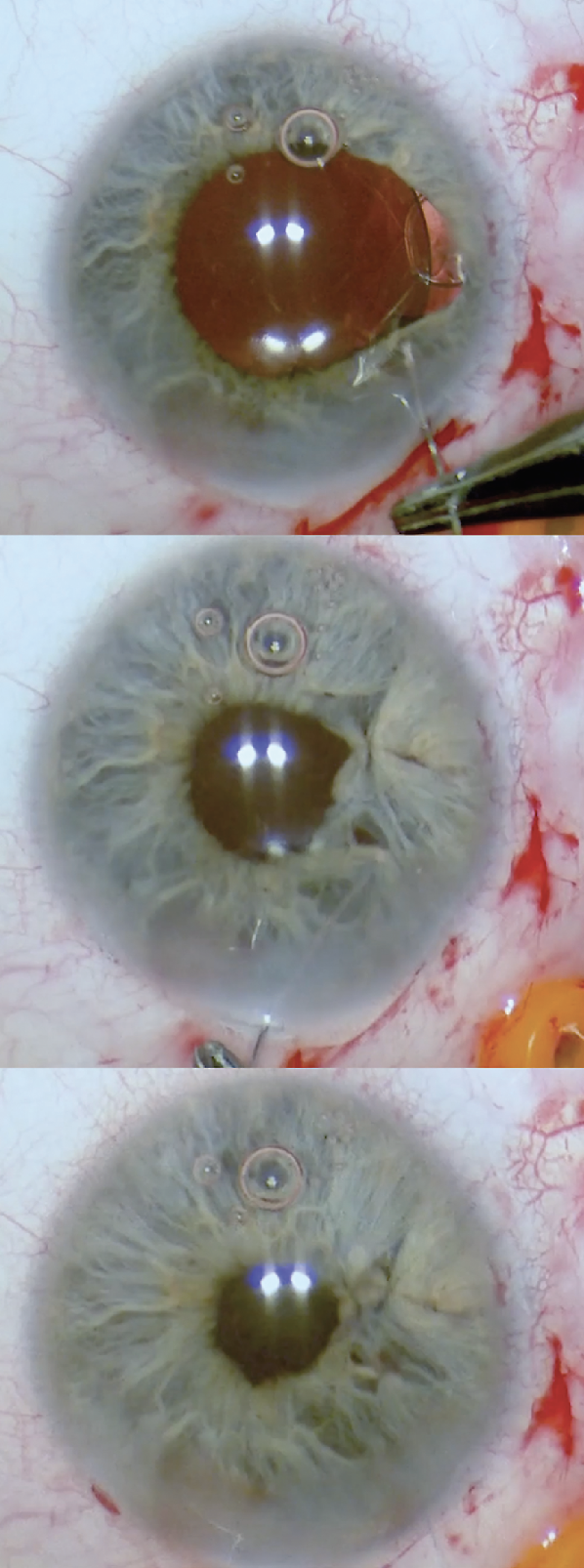
| Figure 1. This patient had a corneal nail penetration through the visual axis, iris and lens into the vitreous cavity. Half of the iris tissue was lost (top image). Synechiolysis, capsule-preserving cataract surgery, removal of fibrous ingrowth, capsular tension ring placement and iris prosthesis placement eliminated the photophobia and restored a more normal body image, recovering 20/50 uncorrected vison and 20/30 with pinhole vision, despite the corneal scar (middle image). On transillumination, note the marked reduction compared to preoperatively. The capsular tension ring can be seen in the perimeter of the bag, just outside the edge of the iris prosthesis (bottom image). (All Images: Michael E. Snyder, MD) |
Iris Repair
According to Nicole Fram, MD, who is in practice at Advanced Vision Care in Los Angeles, if the defect is less than three clock hours, surgeons can attempt suturing the defect. “I use 10-0 Prolene, or polypropylene, and you can use many different needles,” she says. “Ethicon makes a CIF-4 tapered needle that’s very commonly used. It’s nice because it’s very sharp going through the iris, because it’s tapered; however, the surgeon should exit the cornea through a paracentesis, as it can cause a leak in the cornea if it’s primarily exited at the limbus. Or, you can use spatulated needles, such as the Ethicon CTC-6L or Alcon PC-7 needle. For iridodialysis repair, where the iris disinserts from the iris root, surgeons can use a straight needle like Ethicon’s STC-6 needle that we bend a little bit or the CTC-6L (curved).”
Kevin M. Miller, MD, in practice at UCLA Health, agrees that the best suture for iris repair is 10-0 Prolene. “It’s a little bit wiry and hard to work with, but it doesn’t dissolve; it does a good job. And then there’s just the matter of how to tie the knots,” he says. “There are different techniques, which fall into three categories. The first category is the McCannel suture, which was first described by Malcolm McCannel, MD. The suture is passed through the defect, and then a paracentesis is performed. We make a cut in the peripheral cornea near where the iris defect is located, then pull the sutures up to the corneal incision, tie the knot there at the incision, and trim the ends of the suture. The knot drops back inside the eye after you cut the sutures.
Next is the Siepser sliding knot technique. With this technique, there is no need to pull the iris up to the incision. You can actually tie a slip knot outside the eye, loop it around a couple of times and pull the knot back inside the eye. There are a few variations on this approach, but they’re basically the same.
The third technique was popularized by Ike Ahmed, MD, with intraocular tying instruments, like microsurgical tyers. The knot is tied inside the eye. It’s like building a boat inside a bottle. All three techniques work, although some are easier to do than others. The technique we choose is based on the circumstance.”
Dr. Fram says she uses the “Sharpie Pen” test for peripheral small iris defects to make sure iris repair will fix the symptoms. “Sometimes, there are small iris defects, like a laser peripheral iridotomy that was made too large, or it’s properly sized but hitting the tear meniscus of the upper lid,” she explains. “In that case, you can take a small marking pen and color over the cornea in the area of the iris defect and ask the patient if the symptoms improve. These iris defects can have symptoms consistent with ghosting or multiple images, so darkening the area or using an opaque contact lens to show the patient what it would look like if the defect was closed surgically is a helpful test before repairing the defect.”
Transillumination defects are another common indication for small iris repair. This is commonly caused by iris prolapse during cataract surgery in the setting of intraoperative floppy iris syndrome. Postoperatively, surgeons will see transillumination defects where the posterior pigment of the iris sloughs off. “When the temporal iris is missing or damaged in that exposed region, patients can be very symptomatic and sensitive to light,” Dr. Fram says. “In that case, we’ll first put on an opaque contact lens to prove that suturing the defect with an imbricating suture would help. With an imbricating suture, you weave in and out of where the iris defect is, and you bunch up the tissue so that the transillumination defect is less. Sometimes, sectoral areas are missing, where the phaco has eaten up part of it, or they’ve amputated part of the iris because of severe prolapse during the case. These sectorial defects can also be repaired as long as they’re less than two to three clock hours and the tissue is healthy.”
Patients can also experience traumatic mydriasis, where the pupil sphincter muscle is damaged and isn’t working anymore. For this condition, Dr. Fram uses a pupillary cerclage. “We weave in and out in the area where the sphincter muscle was functioning, and we use a purse-string approach to cerclage or close for 360 degrees,” she explains. “Then, we tie the suture in a Siepser or Ahmed fashion. This procedure is probably technically the most difficult surgery I do. It requires you to be very fluent with your right and left hands, and it requires you to be very patient while you’re doing the procedure.”
 |
|
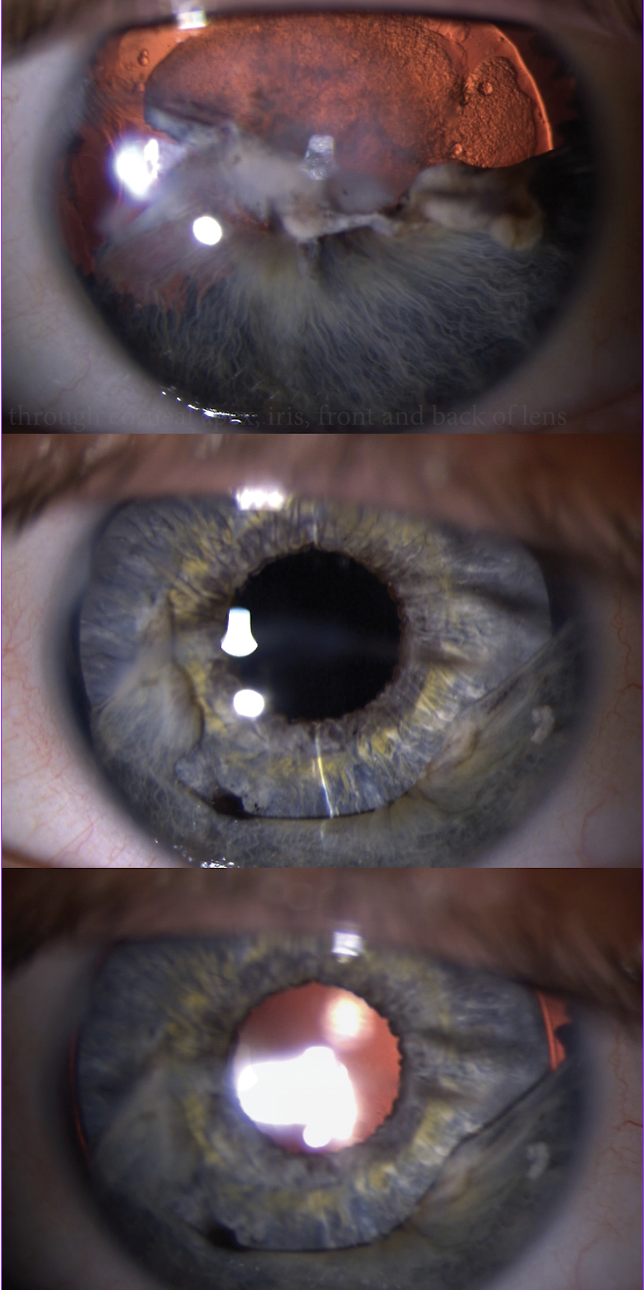
Figure 2. Iris sector defect repair with imbricating sutures at the start of the repair (top), after the first suture placement (middle), and after completion (bottom). |
Artificial Iris Implantation
When the defect is too large to close with sutures, surgeons use an artificial iris. “We can close iris defects, like iridectomy-type defects, maybe up to 1.5 clock hours in size,” Dr. Miller says. “The iris is pretty stretchy, and it will pull together if you do it right. But once you get above about 1.5 clock hours of defect, you can’t pull it together; the sutures will cheese-wire through the iris tissue. In these cases or in cases where there are multiple defects in multiple locations, it’s often just easier to implant an artificial iris device rather than having to deal with closing so many different defects. I implant many more artificial iris devices than I do suture repairs, but that’s because other surgeons send their worst cases to me.”
Only one artificial iris is currently FDA approved. In the United States, the HumanOptics ArtificialIris is distributed by VEO Ophthalmics in Cleveland. It was FDA-approved in 2018. “The artificial iris is an elastomer silicone implant that’s color-matched to the other unaffected eye,” explains Dr. Fram. “So, you take a picture of the eye that doesn’t have the iris trauma. The patient then views and approves the picture, and then it gets sent to VEO/HumanOptics in Germany. They go through this incredible process of putting pigment in the elastomer that’s color-matched to the native iris in the other eye.”
According to Dr. Miller, there are two ways to place an artificial iris in the eye. “Surgeons can either place it with some kind of forceps, or it can be injected through a large injector, like a lens implant injector,” he says. “Then, surgeons need to decide how to fixate the device inside the eye. There are two categories of fixation techniques: passive and active. With passive fixation, you’re basically just placing it in there in some location where it’s not going to move. The two passive locations where you can put the iris are inside the capsular bag and within the ciliary sulcus if there’s good zonule support. In all cases, the natural lens must be sacrificed. Patients who have a clear lens are ineligible for an artificial iris.”
With the active fixation techniques, the artificial iris is secured with sutures. “The most common is suturing the iris to the sclera,” Dr. Miller says. “You can suture the artificial iris to residual native iris tissue if you have enough and it’s not too atrophic. We don’t do much of that, but it’s doable. You can suture the iris to a lens implant that you then suture to the sclera. We used to do a lot of that in the early days, when somebody needed an iris and a lens. But more commonly nowadays, if they need an iris and a lens, we either suture the iris and lens together, and then we suture the iris to the sclera, or we suture both independently to the sclera. You get four-point fixation rather than two-point fixation when you suture an iris implant to the sclera. Then, some surgeons suture the artificial iris to a lens implant, and then they Yamane the lens implant to the sclera. We don’t know if this approach will stand the test of time.”
Artificial irises can also be used in albino patients, which can be life changing. “Most of the time, albinos have no pigment at all,” Dr. Miller explains. “Therefore, the light that enters the eye just scatters, causing fairly profound glare-like sensitivity issues. And in those patients, there’s no pigment to stretch to cover any defect. In these patients, an iris prosthesis is a uniquely wonderful option.”
Dr. Fram adds that there are some caveats to this technology. “Every patient should be consented regarding three major comorbid conditions: glaucoma; corneal edema; and retinal pathology (tear, detachment, cystoid macular edema),” she says. “Because these patients usually have trauma or a history of multiple surgeries, they have some secondary glaucoma to begin with and may need a filtering procedure in the future. Patients should also be consented that we’ll need to check their retinas after surgery to make sure there are no retinal tears or detachments or cystoid macular edema. Then, patients need to be consented that the cornea could require an endothelial keratoplasty in the future. I always do endothelial cell counts and pachymetry, retinal nerve fiber layer, and macular OCT, wide-angle fundus imaging prior to surgery to counsel them about their risk profile prior to surgery.”
She adds that the consenting process should be performed by the surgeon and not delegated, as patients need to understand that this may not be the last surgery that they have. “They need to know that it’s a journey and that you’ll be with them the whole way through,” she adds.
Drs. Fram and Miller have no financial interests to disclose. Dr. Snyder is a consultant for HumanOptics.