|
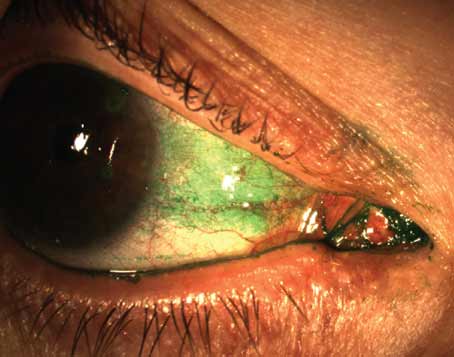
It is often suggested that prolonged exposure to the sun may instigate pterygia formation,3 and given anecdotal observations that it emerges more frequently among surfers and golf enthusiasts than in the general population (with greater prevalence in geographically predisposed areas), the relationship appears valid. Naturally, the climate here in Jacksonville, where I practice, is a fertile breeding ground for this ocular condition. I do however, see a significant portion of my pinguecula and pterygium surgery patients flying in from disparate parts of the country and world in response to word-of-mouth and online referrals that transcend geographic borders. These patients present complaining that they are self-conscious about this condition, embarrassed by their appearance and even depressed, in some cases.
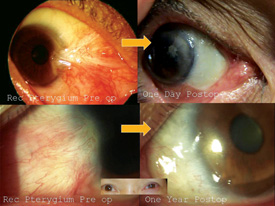
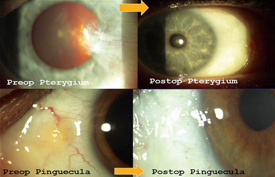
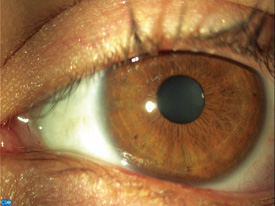
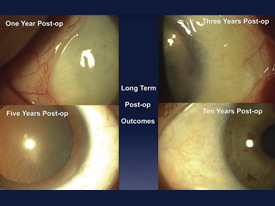
Here, I will share my technique that I have honed over a decade on more than 500 patients, with consistent results. It enables not only those with cosmetic pterygia and pinguecula, but even those suffering from recurrent and aggressive vision-threatening pterygia, to expect clear, white eyes one day postoperatively. Starting with a sutured technique 20 years ago,4 and adding amniotic grafting (Gulani-Tseng) 11 years ago, my method has since evolved into a sutureless procedure that incorporates the healing properties of human placenta.5,6 Patients are universally satisfied with their aesthetic results within 24 hours and are able to return to work and other daily activities within a couple of days.
This technique neither threatens nor adversely affects vision because there are no incisions involved in the cornea. While the average pterygium recurrence rate is commonly considered to hover around the 39 percent mark, the recurrence rate with my technique is less than 1 percent.
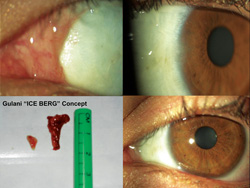
My no-stitch technique utilizes human placenta as a scaffold bandage and chemical facilitator. It lends an elegant appearance to the eye and provides comfortable and expedited healing.4 I call my pterygia removal technique the “Iceberg Technique” because the part of the pterygium that is visible is just the tip of the iceberg, while the actual growth tends to be much deeper, and this surgical procedure addresses that.
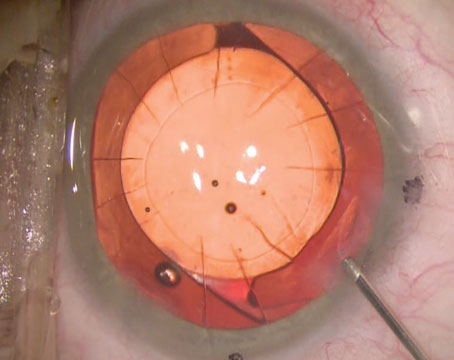
Step-by-Step Technique
My suture-free, three-step pterygium and pinguecula removal technique includes mitomycin-C, amniotic tissue and Tisseel Glue. In a typical case, I begin with a fixation stitch at the opposite limbus and then I delineate the entire lesion with intralesional anesthesia. I then trace the entire pterygium/pinguecula down to its roots, literally cutting down its tentacles using retro-resistance to guide me. Next, I peel back the limbal portion from the cornea using centripetal resistance and follow this up by using a 64-ga. blade to clear the cornea, limbus and sclera, using fast, smooth movements (like an eraser). At this point mitomycin-C (0.04%) is used on four pieces of Weck-cel placed under the conjunctiva (rolled into it and avoiding sclera) for 20 seconds, followed by a copious balanced salt solution flush. I then retrieve the amniotic graft, place it onto the bare sclera and sweep it into place under the medial, superior and inferior conjunctiva using what I call a no-touch “tyre–tool” technique. Next, I use two separate syringes to deliver each component of the Tisseel glue beneath the amniotic graft in a controlled fashion. I follow this by using a Weck-cel sponge to squeegee the graft on the sclera and also to swipe the fornices for any excess glue to avoid the possibility of postoperative keratitis. I then use the same 64-ga. blade in a single, controlled motion to trim the excess amniotic graft along the limbus using a single circumlinear motion. The cut is deep enough to cut the amniotic graft, but not the cornea. I then peel away the excessive amniotic tissue to facilitate an elegant outcome; these patients can wear contact lenses the next day or get ready for refractive surgery soon after. We have had no graft slippage in our series of patients and have had consistent, successful long-term outcomes one-day postoperatively among patients regardless of age, sex or race.
The postop regimen comprises steroid drops q.i.d. for the first week and then tapered down every week by one drop for one month. Non-steroidal drops are prescribed b.i.d. for two weeks, and antibiotic drops are prescribed q.i.d. for two weeks.
Despite the consistency of our results and a satisfied worldwide clientele, we are careful to emphasize to our patients that even though their complaints are often of a cosmetic nature, this is a surgical procedure, and as with any surgical procedure there are associated risks. Even with a recurrence rate of less than 1 percent, the risk of untoward effects, including scarring and the possibility of a worse-looking eye, remains. Three cases with unique circumstances in my experience include a patient who was perfectly satisfied with a sparkling white eye after my surgery; when he flew back home his eye surgeon did not see any stitches or red areas postoperatively, so he rubbed a Q-tip across the eye and rubbed the glued graft off the eye. This patient flew back to me and needed re-grafting. In another case, a patient needed muscle alignment surgery, and in another instance, a patient is being followed up for a localized pupil shape anomaly that is improving. All three of these cases were of extensive bi-temporal surgery, and hence I continue to recommend that patients only have one lesion removed at a time.
Raising the Bar
The importance of this procedure goes beyond successfully treating pterygium and pinguecula patients with a procedure that offers the opportunity for sparkling white eyes one day postoperatively with a less than 1 percent recurrence rate. It also offers a vehicle to maintain the integrity of the ocular surface—or further improve the ocular surface—thereby raising the bar on refractive surgery outcomes.
|
For instance, the elegance of this no-stitch amniotic graft technique enables many patients who were initially non-candidates for laser refractive surgery or premium lens refractive surgery (due to tissue-induced irregular astigmatism, corneal scars, tear film instability or higher order aberrations) to be safely prepared for vision corrective surgery, such as surface ablation and even premium IOLs.7 The removal of corneal scars and pterygium tissue, and the resultant clear and measurable optical system, in essence safely and elegantly converts patients from non-refractive surgery candidates into refractive surgery candidacy.
Also, given that many patients who present with pterygium and pinguecula have already had some form of laser vision surgery or premium lens surgery, this provides a method to maintain their optimized vision during pterygium surgery because it does not distort LASIK flaps, induce keratitis or cause corneal desiccation/distortion with traumatic techniques or refractively adverse corneal incisions.
I have performed LASIK, surface ablation, multifocal IOL/toric IOL/ICL and even Intacs procedures in patients who have undergone my amniotic graft pterygium and pinguecula removal surgery with successful outcomes.8 Given the no-cut nature of my grafting procedure, there is no induced refractive change with this technique—thereby maintaining good vision or perhaps even improving vision by relieving the astigmatism caused by pterygium-induced pull on the cornea.
From my perspective, a worldwide clientele that seeks out our services for this procedure is testimony to the need for safe, effective pterygium and pinguecula surgery that essentially removes the lesions and reduces the threat of recurrence. Our no-stitch grafting technique can be considered to be analogous to the era of LASIK surgery when we moved from expectations of 20/40 vision to 20/20 vision. I am requesting all eye surgeons to raise the bar on ocular surface surgery outcomes to those of cosmetic surgery given the capabilities of our procedure. REVIEW
Dr. Gulani is the founding director of the Gulani Vision Institute, and former chief of the Cornea Service and assistant professor at the University of Florida Medical School.
1. Coroneo MT, Di Girolamo N, Wakefield D. The pathogenesis of pterygia. Curr Opin Ophthalmol 1999;10(4):282-8.
2. Elliot R. The aetiology of pterygium. Trans Ophthalmol Soc NZ 1961;13:22.
3. Blum HF. Carcinogenesis by Ultraviolet Light. Princeton University Press; 1959.
4. Gulani AC. Simultaneous pterygium and cataract surgery. J Postgrad Med 1995;41:8-11.
5. Gulani AC. No-Stitch Pterygium Surgery: Next Day Cosmetic Outcomes. Video Journal of Ophthalmology 2009
6. Gulani, AC. Sutureless Amniotic Surgery for Pterygium: Cosmetic Outcomes for Ocular Surface Surgery. Techniques in Ophthalmology 2008;6(2):41-44.
7. Gulani AC. Principles of Surgical Treatment of Irregular Astigmatism in Unstable Corneas. TextBook of Irregular Astigmatism. Diagnosis and Treatment . Thorofare, NJ: Slack Inc.; 2007:251-261.
8. Gulani AC. Corneoplastique. Video Journal of Cataract and Refractive Surgery 2006;22;3.