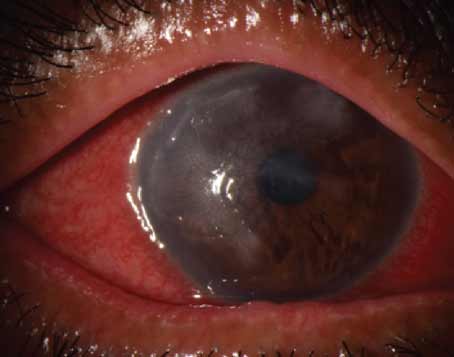
Eyes that have undergone radial keratotomy have irregular corneas, which can present unique challenges for cataract surgeons. Lens calculations, the surgical procedure itself and the postoperative healing period are not routine in these eyes.
Lens Calculations
According to Daniel Chang, MD, who is in practice in Bakersfield, California, the challenge with lens calculations is that these patients have irregular and fluctuating corneas. “You have a target that’s hard to hit and that’s moving,” he says. “When it comes to biometry, it’s a challenge trying to figure out what to do with the information that you get, because every machine is going to give you something potentially very different, particularly when it comes to astigmatism.”
Los Angeles surgeon Uday Devgan, MD, agrees. “Lens calculations after RK are challenging because RK changes the cornea,” he says. “It’s different from LASIK, because LASIK just changes the front curvature of the cornea. In RK, both the front and the back of the cornea are changed. The RK cuts that are made change the whole structure. In other words, in LASIK or PRK, the laser is taking away some tissue; in RK, no tissue is taken away. We are just changing its configuration. By making those radial cuts, you flatten the center of the cornea.”
Because of the RK cuts, when the cornea is measured, surgeons are overestimating its power. “As a result, the typical lens calculation formulas will indicate too low of an IOL power,” Dr. Devgan says. “The key is to adjust the IOL power calculations based on the RK that was done, and there are many different ways of doing this. Probably the easiest is to go to the ASCRS website, where you can just type in all of the data you have.”
Dr. Devgan notes that the amount to add to the lens power depends on how many cuts were made with the RK. “These aren’t as exact as a lens calculator, but are a general rule of thumb,” he says. “If you have a four-cut RK, add 0.5 to 1 D of IOL power. If it’s an eight-cut RK, add maybe 1 to 1.5 D of IOL power. If it’s 12-cut and beyond, add at least 2 D of power. It’s not quite as accurate as doing all of the fancy calculations and special measurements, but it works.”
Richard Hoffman, MD, who is in practice in Eugene, Oregon, uses the ASCRS calculator, as well as the Holladay 2, which has a box to check for post-RK eyes. “When all else fails, you can just use the effective corneal refractive power on your corneal topography,” he says. “That will usually get you close, but the Holladay 2 formula takes into account the corneal topography and the previous RK. I’ve been pretty successful with those two methods in getting people close to where they should be.”
Limitations of RK
Because RK causes the cornea to be irregular, Dr. Devgan recommends not placing a multifocal lens in a post-RK eye. “With RK, the cornea is basically multifocal already,” he explains. “RK isn’t a smooth, clean treatment like LASIK. As a result, RK patients don’t do well with multifocal lenses. I prefer to stick with a monofocal lens in these eyes. RK patients can do very well with a monofocal toric lens if they have a consistent degree of astigmatism.”
Dr. Hoffman agrees that multifocal IOLs shouldn’t be used in these patients; however, he says that surgeons have had success with extended depth-of-focus lenses. “The safest thing is just to implant a standard monofocal lens, but, if you have the right patient who understands all the limitations, an extended depth-of-focus lens is a possible option for them,” he says.
Surgery
 |
|
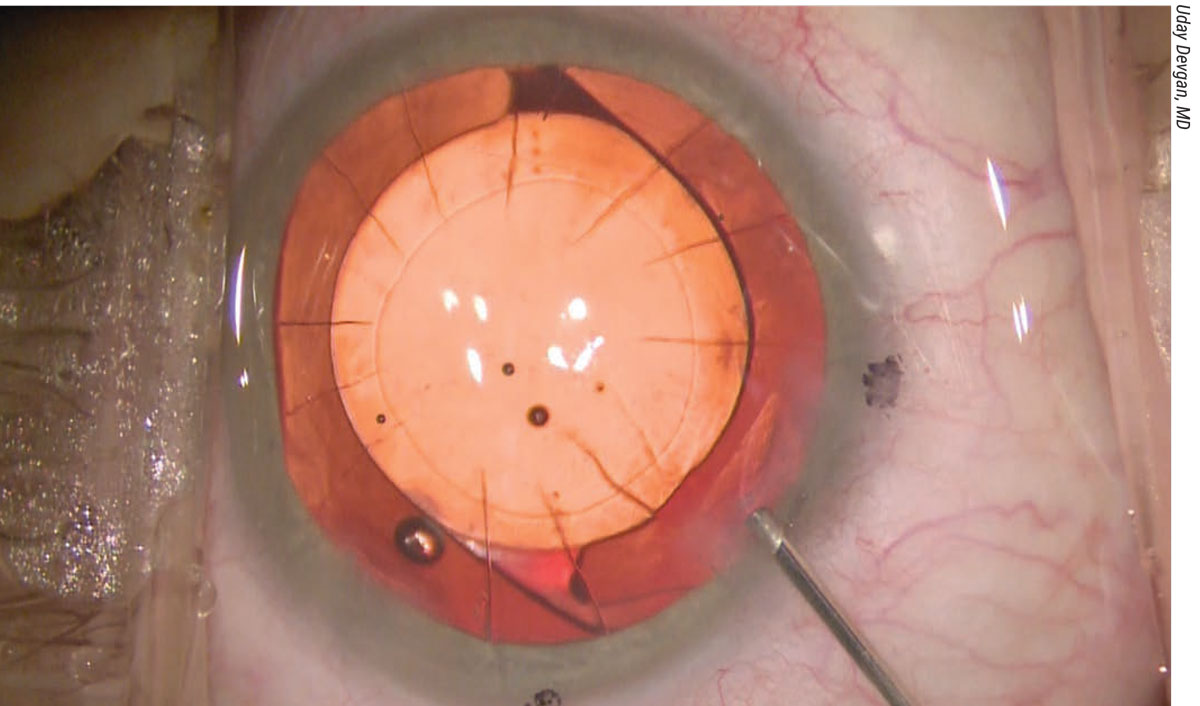
An eye with a toric IOL and many RK cuts. Surgeons say that, in some RK eyes, you can put the entry wound between two of these cuts. |
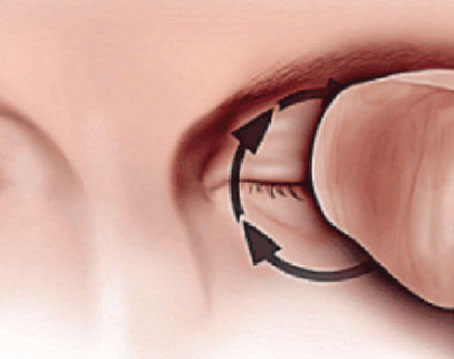
When contemplating surgery, it’s important to remember that RK cuts are typically 90 percent or more of the corneal depth. If the surgeon inadvertently intersects the existing RK incisions when making the cataract surgery incisions, the RK incisions can unzip. “You never want to intersect a pre-existing RK incision,” Dr. Devgan advises. “If you have an eight-cut-or-fewer RK incision, you can usually slip your phaco incisions in between two of the RK cuts. However, once you get to 12-cut or more, you’re probably not going to be able to make your incision in the cornea. In these cases, you may have to revert to making a scleral tunnel incision.”
Dr. Hoffman uses a bimanual technique in these patients. “It’s nice, especially in RK eyes, because you can fit your 1-mm bimanual incisions in between the RK incisions, even if the eye had a 16-cut RK, because usually there’s a space between some of the RK incisions that’s wider than the space between others,” he explains. “Most RK patients have eight-cut RKs, so just a standard coaxial technique can be done. If a patient has many incisions and you don’t do a bimanual technique, then you usually have to cut down the conjunctiva and do a scleral tunnel incision. By having the sclera in the roof of your tunnel, you can go through those RK incisions without them splitting open. If a patient has 24 RK incisions, I can do the entire bimanual procedure through two 1-mm incisions that are fit in between the RK incisions. When it’s time to place the implant, I’ll just do a 2.2-mm stab incision that’s through the conjunctiva and the sclera, so I don’t really have to cut down the conjunctiva.”
According to Dr. Devgan, it’s important not to use too high of an infusion pressure intraoperatively because that can put stress on the RK incisions. “At the end of cataract surgery, I not only check my cataract surgery incisions to make sure they’re sealed and watertight, I also check all the pre-existing RK incisions, too,” he says. “You can do this very easily by using a fluorescein dye strip and painting the whole anterior surface of the eye with the dye. Then, you can see if there’s a leak anywhere.”
In the postoperative period, surgeons and patients should be prepared for swelling of the RK incisions. “Even the gentlest and most beautiful cataract surgery is going to cause the RK incisions to temporarily swell,” says Dr. Devgan. “Sometimes, surgeons will perform a cataract surgery on an RK patient, and on postop day one, the patient-—instead of being plano—is +1.5. The surgeon is distraught, but this is actually OK. Here’s how you tell: Look at the patient’s preoperative K measurements. For a simple example, let’s say the K reading was 36 D. On postop day one, just put the patient back in that same machine and do K measurements. Instead of 36, let’s say it’s 34.50. This means that the peripheral RK incisions swelled up after the surgery and made the central cornea even flatter, but that’s temporary. The patient will typically be 35.50 a week later. Then, two weeks or a month out, the postop K value is back to 36, the swelling has resolved and the patient is plano. So, when you check the patient’s prescription postop, make sure you also compare the keratometry values from before and after surgery.”
Additionally, Dr. Devgan recommends always choosing the higher lens power if you’re choosing between two powers. “RK has been called the gift that keeps on giving, meaning if you make the patient a perfect plano prescription postop, he or she will only stay that way for a couple of years,” Dr. Devgan says. “After a few years, he or she will be +0.5, and then in 5 or 10 years, he or she can be +1 again. The cornea is never fully stable throughout the patient’s life. Always choose the higher lens power, and let the patient end up -0.5 D postop instead of a perfect 0. It will only stay -0.5 D for maybe a year or two, then it’s going to be a perfect plano.”
Managing Patient Expectations
Dr. Hoffman adds that there is a greater chance for refractive surprises in post-RK eyes, so he encourages patients to have realistic expectations. “This is actually not difficult in most RK patients, because, most of the time, these patients have fluctuating vision, and they might have had a hyperopic shift post-RK. They are willing to accept a less-than-perfect result. I tell them that, in a normal patient, there’s a normal bell curve that’s somewhat narrow. In an RK patient, the bell curve is widened, so a patient could end up farsighted or nearsighted enough where he or she would need glasses to fine-tune vision,” he adds.
Dr. Chang recommends asking patients how they felt about the quality of vision they had after RK but before the cataract formed. “The saving grace with these patients is that they were all early adopters,” he says. “They’re not like LASIK patients who expect everything to be perfect, so you have an easier population to deal with in that regard. From a counseling standpoint, you have some advantages there.”
Dr. Hoffman prepares patients to expect a longer period for stabilization of the refraction postoperatively. “For the first few days or weeks, the patient should be farsighted, about a +2,” he explains. “Sometimes, patients will be a +4 or +5 on the first day depending on the number of RK incisions they have, and they will slowly lose that farsightedness. Depending on how many incisions they have, it might take two or three months for their refraction to stabilize, so they have to be patient postoperatively. Many of them experience fluctuating vision throughout the day, and they had that before their cataract surgery. Cataract surgery doesn’t get rid of that, unfortunately, so they can still have fluctuating vision after their cataract surgery.”
Dr. Hoffman also mentions the possibility of the RK incisions opening up during surgery, which would require suturing. “In the worst-case scenario, surgeons will need to suture and glue the incisions,” he says. “This is rare in patients with eight- or 16-cut RK, but I see a lot of patients with 20-cut, 24-cut and 32-cut RKs. In these patients, there’s a greater chance of those incisions splitting open at the time of surgery or toward the end of the procedure. Luckily, I haven’t seen many cases of that lately.”
Dr. Chang is a consultant and investigator for Johnson & Johnson Vision and Acufocus. Drs. Hoffman and Devgan have no relevant financial
disclosures.