While many American surgeons remain frustrated at the lack of Food and Drug Administration approval of collagen cross-linking—in which riboflavin is applied to the (usually) de-epithelialized cornea followed by exposure to UV light, resulting in a measureable stiffening of corneal tissue—the procedure continues to be refined and tested around the world. Most of the conversation in the United States has been focused on the benefits of the procedure, causing some surgeons to worry that limitations and downsides are being overlooked. Here, four surgeons with extensive experience in cross-linking discuss the procedure and address some of the questions that still surround it.
How Risky Is the Procedure?
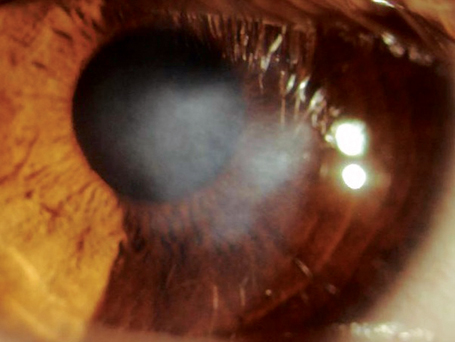
“Cross-linking is a real surgical procedure, which in most forms involves removal of the corneal epithelium,” notes A. John Kanellopoulos, MD, clinical associate professor of ophthalmology at NYU Medical School and director of the Laservision.gr Institute in Athens, Greece. “Unfortunately, it carries all the risks that such procedures carry.
Problems that have been associated with cross-linking include delayed epithelial healing and some epithelial haze, including late epithelial haze a year postop in one patient who had intense UV exposure. In a few cases we’ve seen stromal scarring, and there have been reports of herpetic keratitis, assumed to be a recurrence incited by the cross-linking procedure. There have also been reports of infectious keratitis.”
|
Dr. Kanellopoulos notes that the occasional case of delayed epithelial healing could be a collateral effect of the cross-linking. “It could be a toxicity effect caused by the procedure itself; the postop medications used on the stroma that’s going to be epithelialized; and/or the shock to the limbal stem cells that repopulate the surface of the cornea,” he says. “This is something that needs to be studied to find out what the long-term effect on limbal stem cells might be. As far as scarring, anytime you de-epithelialize the cornea this is a risk, especially if there’s delayed epithelial healing or excessive cross-linking in the corneal stroma. And we still have to keep an eye out for a potential increase in the risk of carcinoma in the conjunctiva and corneal epithelial cells due to the UV light. It’s a known risk for sun exposure; theoretically, it has to be a potential risk for cross-linking as well.”
Roy S. Rubinfeld, MD, MS, clinical associate professor at Georgetown University Medical Center, and in private practice in Chevy Chase, Md., believes that most of the risks associated with collagen cross-linking have been a result of the removal of the epithelium in the original version of the procedure. “Any time you make a large, 9- or 10-mm epithelial abrasion you then have the risks of infection, haze and delayed epithelial healing,” he points out. “In a handful of cases worldwide, delayed epithelial healing after cross-linking has also caused corneal melts.”
As far as characteristics associated with increased risk, Dr. Rubinfeld notes that one study authored by Theo Seiler, MD, PhD, found that patients with very steep corneas had a higher chance of problems or failure—at least when using the epi-off technique.1 “So far, our work with the epi-on approach [leaving the epithelium intact] has not found that to be the case,” he says. “In our study, out of more than 1,200 eyes treated to date, I’m only aware of two patients whose keratoconus progressed in spite of treatment, and those individuals can be retreated. Adverse events have been extremely rare in our studies.”
Despite the risks, Dr. Kanellopoulos doesn’t believe the procedure is dangerous. “In general, these cases represent a very small percentage of the total number of cases done,” he says. “This procedure is performed globally at thousands of centers, and the majority of cases are relatively uneventful. Using our Athens protocol, consisting of topography-guided PRK and cross-linking, delayed epithelial healing—meaning healing delayed more than four days—happens in about 5 percent of cases, as we reported in a paper presentation at the 2011 annual meeting of the American Academy of Ophthalmology. We’ve seen some minor anterior scarring in less than 1 percent of the cases. We haven’t encountered any infectious keratitis in the 420 cases we’ve done. I think that if one is aware of these risks and able to diagnose them early, cross-linking isn’t any more dangerous than PRK or pterygium removal, or any other well-evaluated procedure that we perform on the anterior surface of the eye.”
Dr. Rubinfeld adds that cross-linking risks, which are uncommon to begin with, need to be taken in context. “The alternative to cross-linking is progressive vision loss, hybrid contact lenses and in many cases, corneal transplant,” he points out. “Corneal transplants work, but I don’t know a single corneal specialist who would rather have a transplant performed on himself than have collagen cross-linking. Even with the removal of the epithelium, cross-linking remains a relatively safe procedure, resulting in approval in all 25 European Union nations by 2006. The United States remains the only developed country I’m aware of that has not approved this procedure.”
Are the Complications Serious?
Despite the low rate of complications, surgeons still hope to minimize or eliminate them through better understanding of their causes.
• Infectious keratitis. Like most surgeons who have performed the procedure many times, Raymond Stein, MD, FRCSC, director of the Bochner Eye Institute, assistant professor at the University of Toronto and former president of the Canadian Society of Cataract and Refractive Surgery, sees the procedure in a very positive light. “At the Bochner Institute we’ve done close to 3,000 eyes over the past four years, and our success rate is 98 percent or greater,” he notes. “In addition, we can offer a second treatment to the small number of patients who still show progression.”
Dr. Stein says that complications such as infections are rare. “There were a few infections reported in some U.S. trials that were thought to be related to contaminated riboflavin solution,” he notes. “However, at the Bochner Eye Institute we haven’t seen one infection in four years.”
Part of the explanation for the low infection rate might be that the procedure is known to kill bacteria. “Studies have shown that cross-linking can be used to treat infections, because it’s microbicidal,” says Dr. Rubinfeld. “One of the centers in our study is testing this protocol as well. However, this doesn’t necessarily preclude any risk of infection after a cross-linking procedure, especially if the procedure creates a large epithelial defect. Once the procedure is over and the light is gone, bacteria have six or seven days to gain entrance into the stroma—which is another argument for switching to epi-on.” (Dr. Rubinfeld says he doesn’t mean to overemphasize the risk of infection with epi-off cross-linking, noting that it is uncommon.)
“There’s also a risk that the riboflavin solution itself may be infested with bacteria,” Dr. Kanellopoulos points out. “Obviously, antibiotic prophylaxis, basic hygiene and precautions for the first week are in order, just as you would use with any procedure that de-epithelializes the cornea.”
Dr. Kanellopoulos says it’s hard to tell ahead of time which patients might be at risk of infection. “We do know that if a patient’s healing is delayed, we need to see him more often,” he says. “We may use a bandage contact lens, and we’ve employed autologous serum as a medium to help the epithelium heal faster in some extreme cases. Sometimes we use topical cyclosporin to help the tear film. In many southern Mediterranean patients, such as those we see in Greece, there are coinciding diseases such as blepharitis and ocular surface disease that may also become involved.”
• Haze. “Haze has not been a significant concern,” says Dr. Stein. “Many investigators are trying the transepithelial approach because they thought that haze was a significant problem, but we haven’t seen that. Haze is not uncommon at four to six months if the epithelium is removed, but the haze is usually gone by nine to 12 months.”
Dr. Stein notes that the cause of the haze isn’t clear. “The haze is not scar tissue,” he says. “We don’t really understand it. Maybe it’s some reaction with the collagen fibers, and as the collagen realigns over time, the haze tends to disappear—even without drops. Any haze that does appear is certainly not disabling.”
• Delayed epithelial healing. Dr. Stein notes delayed epithelial healing is rare. “Usually the epithelium heals within four to five days,” he says. “In rare instances it takes longer to heal, and those patients are more apt to have some corneal haze, but that tends to disappear with time.”
Which Protocol Works Best?
Although no protocol has been officially established for the cross-linking procedure, most surgeons seem to be following the original Dresden protocol, which involves removing the epithelium before applying the riboflavin solution, and a fairly lengthy exposure to a low level of UV light.
Dr. Stein agrees that using the Dresden protocol makes sense for now. “That’s the protocol for which we have long-term follow-up,” he notes. “Of course, many companies and surgeons are trying modifications of that protocol, in particular the trans-epithelial approach—i.e., leaving the epithelium on—and modifying the UV light energy level.
There’s some good data coming out about the transepithelial approach. If it works long-term, that would be great because the patient would be more comfortable and have a quicker return of vision. However, we don’t really know what the long-term success rate will be.
| ||||
“The same is true for modifying the energy level,” he continues. “The original Dresden protocol uses an energy level of 3 mW/cm2. There are groups that have increased this to 30 and even 45 mW/cm2. If you increase the energy level to 30 mW/cm2, then instead of 30 minutes of UV light time, only three minutes would be required; if the results are the same as with the lower energy, obviously that would be preferable. But we don’t really know yet.
“I believe any alternative protocol has to have a success rate that matches the Dresden protocol, which is about 98 percent in patients with corneas under about 58 diopters,” he adds. “If any of these alternative protocols turns out to have a 98-percent long-term success rate, then that’s the way things are going to go. A 10 or 15 percent failure rate would probably be unacceptable.”
Dr. Kanellopoulos agrees that the Dresden protocol is the current standard for the cross-linking procedure. “However, we just returned from that group’s annual cross-linking session in Zurich, where an exposure protocol of 10 mW/cm2 for 10 minutes was officially sanctioned,” he says. “We’ve been advocating that shift to higher fluence for the past five years, and we’ve presented strong clinical evidence that it’s as least as effective as the classic Dresden protocol. In addition to cutting the surgery time by two-thirds, it may cause less keratocyte damage. Keratocytes, like most human fibroblasts, have proven to be more resistant to higher fluence UV light exposure for shorter amounts of time, versus the opposite.”
Dr. Kanellopoulos notes that some new evidence regarding the biochemical mechanism of the cross-linking process may support altering the protocol. “Traditionally we thought that cross-linking was accomplished by a Type-Two photochemical reaction of riboflavin being photosensitized by the UV light and becoming a triplet, which in turn creates an oxygen radical,” he explains. “The oxygen radical then would cross-link the collagen. Now, in work that’s been done at Avedro in Boston, they’ve shown that when using the classic Dresden protocol there’s no oxygen available in the cornea past the first minute of the procedure. So this creates a huge question mark: How is the cross-linking occurring from minute one, when the cornea is depleted of oxygen, to minute 25 when there are signs that oxygen returns to the corneal collagen? The speculation is that the riboflavin triplet may be a strong conduit for cross-linking as well. This is called the Type-One reaction, performed by the riboflavin.
“All of this is still theory, but it really changes the thinking behind the choice of light exposure parameters and how much riboflavin is needed,” he continues. “The data is quite strong, and it supports our original clinical observation that higher fluence appears to be as effective as lower fluence. Previously that seemed questionable because higher fluence would theoretically deplete oxygen even faster. However, it could actually facilitate the riboflavin triplet part of the reaction.”
In the meantime, Dr. Kanellopoulos sees no problem with surgeons adopting the Dresden protocol as their initial approach. “I’m pretty sure that over the next few years we’ll see a spectrum of protocols, in part because we won’t need to cross-link every eye the same amount,” he says. “We’ll cross-link some eyes prophylactically, while other eyes with ectasia will require urgent cross-linking to avoid a transplant. For most surgeons, the first indication for it would be ectasia, and I think the Dresden protocol is sufficient as a standard for that purpose.”
Still, some surgeons are concerned about the consequences of using too much riboflavin or UV light. “Riboflavin isn’t toxic,” notes Dr. Rubinfeld. “It’s a vitamin. Of course, the optimum concentration of riboflavin to perform cross-linking in any given patient is unknown. As far as the possibility of too much UV light exposure, some previous lab work has suggested that this could be a risk. On the other hand, the cumulative dose of UV light in the Dresden protocol is 5.4 joules, which is about the amount of UV light that a cornea is exposed to over the course of 15 or 20 minutes on a summer day at the beach. So we’re not talking about very high levels of UV radiation with that protocol. However, some studies going on now use much higher irradiance, and the safety of that could be in question.”
Epithelium On or Off?
Dr. Rubinfeld is a member of the CXLUSA research group. “One of the things our organization has done since 2009 is set up multiple protocols via physician-sponsored, institutional-review-board-approved studies,” he says.
“We’ve done this for two reasons: first, to make the technology available on an investigational basis to patients in the United States; and second, to discover ways to improve the procedure. Starting in May 2010 our multicenter trial has also included epithelial-on cross-linking treatments, and we’ve had excellent success rates.
|
“Leaving the epithelium on has numerous benefits, including speeding the patient’s visual recovery,” he continues. “Recovery often takes weeks or months when the epithelium is removed, but may take less than a day when the epithelium is left on. Perhaps more important, it eliminates most of the risks associated with the original Dresden protocol. If you don’t remove the epithelium, you won’t develop problems associated with delayed epithelial healing; your risk of infection is enormously reduced; and haze and scarring seem to be markedly reduced as well.”
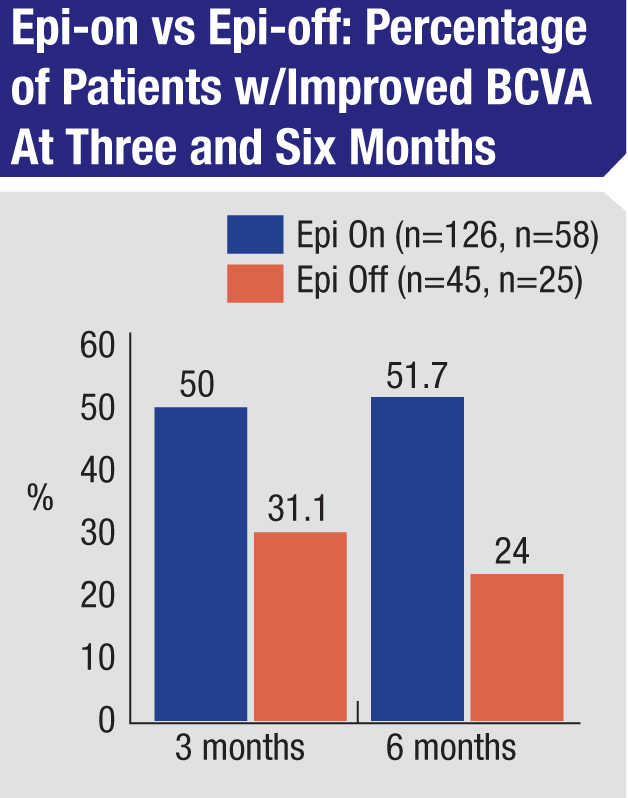
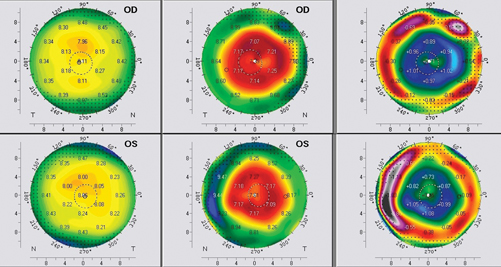
Dr. Rubinfeld says that some mixed results from early attempts at epi-on cross-linking may have resulted from issues relating to the riboflavin. “Some of the early work in this area used a formulation of riboflavin that didn’t penetrate the epithelium very well,” he explains. “It had high molecular weight components, so it was a real challenge to get the riboflavin into the corneal stroma, and that has to happen in order for effective cross-linking to occur. Using our current formulation, we’re finding that our epi-on cross-linking is just as effective at three months and six months postop—or more so—than our prior work with epi-off cross-linking.” (See chart, above.)
Many surgeons are still hesitant to try this approach without seeing clinical evidence supporting it. Arturo S. Chayet, MD, who practices at the CODET Vision Institute in Tijuana, Mexico, is concerned that leaving the epithelium on is unproven and could lead to patients not getting the corneal stiffening they need. “So far, there’s little scientific data showing that it works to leave on the epithelium,” he says. “So I think it’s risky to try to do this with the epithelium intact, especially with a patient who really needs the cornea to be stiffened.” He adds that individual case reports can be misleading. “If you do cross-linking with the epithelium on in a 35-year-old patient and you document that there wasn’t any increase in the keratoconus, that doesn’t mean it was because of the cross-linking,” he points out. “Plenty of individuals with keratoconus at that age don’t progress.”
Astigmatism Management
Of course, for many patients, cross-linking by itself isn’t sufficient. “Cross-linking stabilizes the cornea, and in some cases improves the patient’s level of vision,” says Dr. Stein. “But if patients have developed significant irregular astigmatism that prevents them from seeing well with glasses, they may still need a hard contact lens to improve their visual quality. The best time to do cross-linking is when a patient with keratoconus still can see well with glasses, to prevent the disease from getting worse.”
Dr. Stein says that there are a number of different options open to patients who have astigmatism and keratoconus. “If the patient is successful with a hard contact lens, then we’ll simply do the cross-linking,” he says. “But if the patient doesn’t want the contact lens, or is having trouble wearing contact lenses, then we have two options. One is topographically linked ablation, where we use the excimer laser to remove tissue, usually from the superior cornea; in most cases that the part of the cornea that’s least affected by the keratoconus. By removing some tissue and steepening the upper cornea, we improve the regularity of the cornea, giving the patient better vision. The other option is a corneal ring segment such as Intacs. In most patients with keratoconus we put in one ring down below to flatten the cornea.
“My own feeling is that the topographically linked ablation will prove to be the best option for these patients long-term,” he continues. “We‘ve seen problems with rings, such as extrusions and vascularization, and patients tend to develop precipitates around the ring long-term. So I’m not very comfortable with using the rings, especially with patients under 45 years of age. My feeling is that using the excimer laser to smooth the cornea and combine it with cross-linking is really the way to go.”
Potential Clinical Pitfalls
Though the procedure is relatively straightforward, certain basic criteria have to be met.
• Corneal thickness measurements have to be accurate. “One of the most critical points is making sure you have good equipment,” notes Dr. Stein. “Most laser vision correction specialists have either Orbscan, Pentacam or Galileo units that measure pachymetry across the entire cornea.
That’s very important because I’ve seen hand-held pachymetry miss the thinnest point on the cornea, and you can get into trouble if the cornea’s too thin. We know that with the Dresden protocol the UV light will affect the keratocytes that are down about 300 µm. So, if you’re dealing with a cornea that’s 350 µm at the thinnest point and you take off 50 µm of epithelium, you’ll be in danger of damaging the corneal endothelium. That could be a significant problem.”
|
• The riboflavin solution has to be unadulterated. “It’s important to make sure that the riboflavin drops are made up by someone with experience,” says Dr. Stein. “Just having them made up by your own nearby pharmacy that’s not used to making them could be a problem. I would at least get them from a very reliable source, such as one of several companies that specialize in making the riboflavin drops.”
• Patient expectations need to be realistic. Dr. Rubinfeld notes that when offering this procedure to keratoconus or ectasia patients, it’s important to realize that the patient may be hoping for more than you’re saying the procedure will accomplish. “Patients are usually happy if you tell them you can stop their loss of vision, even though they probably won’t see better than they do currently,” he explains. “But in their hearts they’re hoping you’re just underplaying what you can accomplish with cross-linking. They’re thinking that their friends have had some kind of eye surgery—probably LASIK—and they saw great. So you have to make sure the patient’s expectations are realistic.”
Who Should Get the Treatment?
“Keratoplasty and ectasia patients probably represent 99 percent of the common indications for cross-linking,” says Dr. Stein. “Other groups might include patients with infectious keratitis that’s non-responsive to normal topical therapy, and some cases of bullous keratopathy or swelling where the patients are uncomfortable and don’t wish to have a corneal transplant. For these patients, cross-linking can make the collagen fibers more compact and decrease some of the edema to the epithelium. These cases are not common, however.”
“There’s no question that cross-linking stiffens the cornea,” notes Dr. Chayet. “However, there’s not enough data and information to make sure that cross-linking will help every patient. I’m sure it makes a difference in the teenager recently diagnosed with keratoconus who is rapidly progressing. That’s the number-one type of patient you want to treat.
“However, that’s totally different from an adult older than 30 who comes to your office with keratoconus,” he continues. “I have at least 15 patients in that category that I’ve been following for five years. These patients were previously just in medical therapy using antihistamines, instructed not to rub their eyes, etc. In five years, their keratoconus hasn’t worsened. I don’t think anybody should do cross-linking on a keratoconus patient older than 30 unless they’ve documented a worsening of the cornea in the past three to six months. It’s not clear that there’s any benefit, so without that evidence you’re subjecting the patient to needless risk—albeit a small risk—and you’re probably wasting the patient’s money. I give these patients glasses or maybe implant a phakic IOL. I wouldn’t want the cornea to be touched by anything, including contact lenses, which could make the problem worse.
“Ectasia is different,” he adds. “You can have ectasia in a 35- or 45-year-old person. For those patients, if you caught the patient in an early stage, cross-linking may help. On the other hand, if it’s not early stage ectasia, that patient already has a bad cornea. The bottom line is that cross-linking should only be done to corneas that are in the process of getting worse. Don’t do it in a 40-year-old with keratoconus who’s been stable for the past 10 years.”
However, Dr. Kanellopoulos says there are situations in which his group will use cross-linking despite the absence of progressing disease. For example, he notes that in Greece he often sees patients who are close relatives of individuals known to have keratoconus. “Their corneas may appear to be perfectly healthy, but we can’t consider these patients 100-percent normal,” he says. “That’s one of the situations in which I would use prophylactic collagen cross-linking.”
Cross-Linking and LASIK
Ectasia following LASIK is rare, but it’s a major concern for every LASIK surgeon. Cross-linking shows promise as a means to prevent it. “Some companies are promoting this, and it’s an interesting concept,” says Dr. Stein. “The question is: What is the incidence of ectasia after LASIK? In our experience, it’s maybe one in 10,000 in patients whose flaps were made with a mechanical microkeratome, which are the cases for which we have the longest follow-up. But in the past four or five years, a high percentage of surgeons have switched to using the femtosecond laser and making a thin flap, and I suspect the incidence of ectasia will be lower for these patients. Will it be one in 20,000? If that proves to be the true incidence, does it make sense to treat 20,000 patients to prevent one case of corneal ectasia? Also, I haven’t seen any published results demonstrating that the outcomes are the same when cross-linking is done with LASIK, in terms of the quality of vision.”
“I understand why surgeons would want to try this,” says Dr. Chayet. “If strong data supports it, it’s okay with me. But I’ve been doing LASIK for 17 years, and my rate of ectasia is about one out of 10,000 eyes. I’m very careful with my patient selection and procedure selection. I’m not in favor of cross-linking every LASIK patient unless we have data that supports that it’s safer that way. Again, if nothing happens in the six months after the LASIK, that doesn’t mean that cross-linking helped. If you do a good job, your rate of ectasia after LASIK will be very, very small.”
In contrast, Dr. Kanellopoulos is a proponent of using prophylactic cross-linking in routine LASIK cases, which he refers to as “LASIK extra.”
He sees benefits beyond simply preventing ectasia. “During the past year we’ve employed LASIK extra quite heavily,” he says. “We’ve found it to be extremely effective. A recent study from England found that healing is faster in prophylactic cross-linking LASIK cases, and it holds a potential benefit because it sterilizes the surgical field. Furthermore, we’ll be presenting data at ASCRS from a study of LASIK patients in whom one eye was done with cross-linking and the other without. The postop eyes show a different corneal OCT and a different biomechanical response, especially in hyperopes.
|
“The only downside to using cross-linking for all LASIK patients is that it delays best-corrected visual acuity by one or two days,” he adds. “The next day the eyes are about 20/30, although they reach at least 20/20 within a week. LASIK without cross-linking, of course, usually produces 20/20 on the first day, and this has been our experience over the past two years using the Alcon Refractive suite—the FS 200 femtosecond laser and the EX500 excimer laser.”
Dr. Kanellopoulos says his group has narrowed down its protocol to one minute of high-fluence 30 mW/cm2 of UV light. “We use sodium phosphate 0.1% riboflavin solution without Dextran to soak the corneal bed after the LASIK procedure,” he says. “We lay the flap on after a minute of soaking. Then we rinse carefully to remove any remnants of the riboflavin or any vehicle of the riboflavin solution, and expose the eye to 30 mW for a minute using the Avedro device.”
Dr. Kanellopoulos says that his group’s studies are finding that prophylactic LASIK is especially useful when performing hyperopic LASIK. “In studies that we’ll be reporting at ASCRS in April we’ve found that after almost two years of follow-up, hyperopes appear to have a completely different clinical course if we employ prophylactic cross-linking in their LASIK procedures,” he says. “Hyperopic LASIK typically regresses more than myopic LASIK. In hyperopic LASIK we excavate the cornea in the mid-periphery, and we theorize that this causes that area to bulge out over the next year, making the central cornea flatten, which would explain the recurrence of some of the hyperopia.
“We now have strong initial evidence from our one-eye-standard/one-eye-with-cross-linking study that cross-linked eyes have a more stable keratometry and show a more effective correction of their hyperopia,” he says. “Cross-linking appears to tighten up the tissue and not allow that regression to happen. This isn’t related to potential ectasia, because we wouldn’t be expecting ectasia in these eyes; they’re usually thicker corneas and we don’t remove tissue from the central cornea. Cross-linking in these cases seems to inhibit the biomechanical change that the hyperopic ablation induces the cornea to perform. So we’re very enthusiastic about this as an adjunct treatment for hyperopic LASIK. The statistical significance of the early data is strong enough that we believe cross-linking in hyperopic LASIK may become a necessity.”
In any case, Dr. Kanellopoulos believes that prophylactic cross-linking with LASIK will eventually be commonplace. “When we introduced this idea a few years ago, it may have sounded radical,” he admits. “But it holds several advantages, as described earlier. Although LASIK ectasia is very rare, if cross-linking within a LASIK procedure is simple, fast and safe, I see no reason not to restructure the biomechanical change that we create with LASIK, even if it’s not necessary in every patient.”
Other Questions
Other concerns and possibilities still being addressed include:
• What about using cross-linking to halt infection? “Researchers have shown that if you take bacteria on culture plates and add riboflavin and apply UV light, it kills all of the bacteria,” notes Dr. Stein. “In fact, some clinical investigators are using cross-linking to treat infections that haven’t responded to topical medications. I’ve done a number of cases like that myself, and it’s been successful in a high percentage of them. However, these are usually severe infections that would normally leave significant corneal scarring; the goal is just to eradicate the bacteria or parasites. Most of these patients will still need a corneal transplant.”
• How thin is too thin? “When the diagnosis is keratoconus we generally recommend treatment for all patients as long as they have satisfactory corneal thickness, which is usually 400 µm or greater after the epithelium is removed,” says Dr. Stein. “However, we’ve been successful treating patients with 320 µm or greater, in that we induce some swelling.”
• How much cross-linking is necessary for a given patient? “How stiff do you have to make the cornea to prevent it from progressing?” asks Dr. Stein. “We don’t know. With the German protocol, the early data showed a fourfold increase in corneal stiffness, but maybe just doubling the stiffness would be satisfactory. I suspect that if you’re operating on someone with a very weak cornea, like a 10-year-old with keratoconus, you’ll need to stiffen the cornea a lot more than you will with someone 30 years of age. This will be worked out over time, but in the meantime it doesn’t appear to be a problem if you stiffen a cornea too much. At least that’s suggested by the more than 10-year follow-up data in Europe.”
• Would cross-linking be practical for most American practices? Dr. Stein notes that when preparing to offer cross-linking there’s no major investment in equipment required, as long as your office already owns an instrument such as the Orbscan, Pentacam or Galileo. “However, keratoconus isn’t that common,” he points out. “We generally see one case in a thousand in our population. Also, what tends to happen in each city is that surgeons initially get very busy doing lots of cases, but the numbers tend to go down over time.” He adds that a long time between cases probably isn’t harmful in terms of falling out of practice. “Technically, this is probably the easiest procedure to do that we’ve adopted in our practice. Even if you’re only doing a few cases a month, surgeons should be able to make a go of it.”
Dr. Chayet points out, however, that with the limited patient selection, cross-linking isn’t a money-making procedure. “It’s more a service to those patients who really need it,” he says. “We only do about four eyes per month.”
• Does it improve vision, and if so, for whom? Dr. Rubinfeld notes that cross-linking does improve vision in a number of patients. “We’ve found that about 50 percent of the time patients achieve a significant improvement in vision,” he says. “Nearly all studies have found some improvement in corneal curvature and some flattening after cross-linking.
“However, the reasons for the improvement in vision may be more complex than that,” he continues.
“For example, Cynthia Roberts, PhD, has noted that cross-linking changes the cornea’s index of refraction. All of our investigators have seen cases in which the topography doesn’t look particularly different after cross-linking, but patients go from 20/200 uncorrected to 20/40 uncorrected with markedly reduced astigmatism and better BCVA. One possible explanation is that the cross-linking process is changing the index of refraction.
|
“So far,” he adds, “we haven’t determined which patients will end up with a significant improvement in visual acuity, or the optimum means of achieving that. Of course, this is not LASIK. When we discuss what we think we can accomplish with patients in our study, we tell them that the most important goal, the one we achieve 98 or 99 percent of the time, is to stop their loss of vision.”
• When will American surgeons have access to the procedure? Dr. Rubinfeld notes that the cost of an FDA study is the issue holding up approval of cross-linking in the United States. “An FDA study can cost $50 million because it’s a pre-market approval study, with all that entails,” he says.
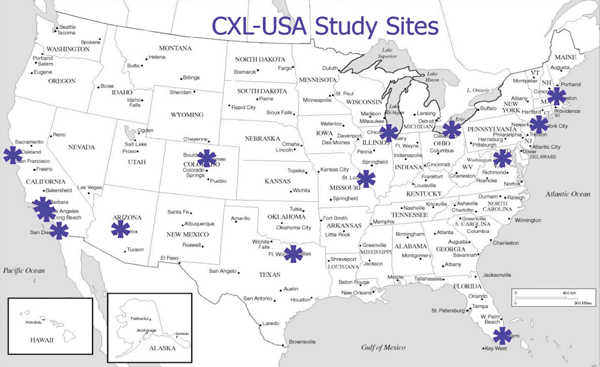
Despite the lack of FDA approval, many patients may be able to receive treatment, thanks to efforts such as the physician-sponsored multicenter trial being conducted by CXLUSA at 12 centers spread across the United States, “We tried to achieve a broad geographic distribution so no one would have to travel across the country to have access to this technology,” notes Dr. Rubinfeld. “The easiest way to find the nearest location of a participating center is to go to our website,
CXLUSA.com. The study is still open and enrolling patients.”
A Premise With Promise
Despite the potential risks, most surgeons who have performed the procedure are totally positive about it. “For the right patients, I think cross-linking is totally worthwhile,” says Dr. Chayet. “The benefits are real, and the complications are extremely low. Many of these patients are desperate. Now we can offer them something.”
“I think the procedure’s good reputation is well-deserved,” agrees Dr. Stein. “We haven’t had one patient in four years who has gone on to require a corneal transplant after cross-linking. At this point, we don’t understand the science very well; all we know is that the clinical results are very good, with a very low complication rate, so we’ve got something that’s really worthwhile for our patients. And we’ll learn more as we go.” REVIEW
Dr. Kanellopoulos is a consultant for Avedro and Seros Medical; Dr. Rubinfeld has a financial interest in CXLUSA, and in technology related to cross-linking. Drs. Chayet and Stein have no financial ties to any product discussed.
1. Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal cross-linking. J Cataract Refract Surg 2009;35:8:1358-62.