 Key on History
Key on History
History is very important because it is often enough by itself to lead to the appropriate diagnosis. As with any disease process, knowing about the “who, what, where” of the problem can help pinpoint the cause. For tearing the easiest question to ask is how much tearing is there, quantifying by how much a patient needs to dab the eyes or wipe the face can help determine its cause and severity. Very mild tearing is less likely related to a complete nasolacrimal duct obstruction (NLDO), whereas constant tearing down the face probably is. Determining when tearing is made worse can also be telling. Patients with tearing secondary to anterior segment issues like dry eye or blepharitis often note tearing worse at the end of the day, or when doing vision-intensive work like reading or computer work; patients with an NLDO will note that tearing is worse outdoors when it is cold or windy. Associated symptoms such as sharp pain followed by tearing is classic for dry-eye-induced tearing. Swelling and pain of the eyelid or medial canthus points to an NLDO or dacryocystitis. Finally, any history of sinus disease or facial trauma should be elicited. The presence of chronic rhinosinus infections or previous trauma including cosmetic rhinoplasty can be associated with a nasolacrimal duct obstruction. Bottom line: A good history will help you focus the examination.
A Guided Exam
The examination of the tearing patient should be similar to that of any ophthalmic patient with special focus and stops along the way. It should be guided by the history and also cover the possible causes of tearing. I always begin by looking at the patient away from the slit lamp. This can be done during the interview process and is very helpful in evaluating non-cooperative patients prior to the hands-on. I like to first observe the condition of the skin and eyelids. In a patient with chronic tearing, the skin around the affected eye is often erythematous and scaly; this is especially true at the medial and lateral canthus where a patient will often rub or dab the eye. Also look for eyelid malpositions; entropion or ectropion is also easily visible without eyelid manipulation. Also observe the patient blinking, both strength and rate. Patients with concurrent or partially resolved Bell’s palsy will have a decreased blink strength and rate or even lagophthalmos. In patients with increased blink rate, think ocular irritation or blepharospasm causing tearing. Then look at the eyes; it is often easy to see if the eye is glistening and wet; if this correlates with the side that has symptoms, then an obstructive process is more likely. If the dryer eye is the symptomatic eye, then dry eye may be the underlying issue.
The next step is physical examination, but still without the slit lamp. A muscle lamp is a perfect light source. The lower eyelids should be examined for presence or absence of laxity with the snap test, where the eye is distracted away from the globe to see if it resets back to the globe or requires a blink to restore its position. Also the eyelid should be closely examined for its natural eyelid position; is the lateral canthus above, in line, or below that of the medial canthus? Downward displacement of the canthus also suggests eyelid laxity, which can cause the epiphora. The puncta medially should also be checked to see if they are in contact with the globe. The eyelid should then be distracted laterally and upwards to see if that restores the natural eyelid position, particularly the puncta of the eyelid. The medial canthus should be examined for any fullness, particularly where the lacrimal sac lies. The lacrimal sac region should be massaged, and if fluid or mucopurulent discharge results, then a nasolacrimal duct obstruction is present.
The examination then can be aided with the slit lamp. The tear lake, the level of tears at the junction of the lower eyelid and globe, should be evaluated. A decreased tear lake points to dry eyes, whereas an increased tear lake is probably due to an outflow problem. The eyelid margin should be assessed for the presence of meibomian gland dysfunction or blepharitis. The eyelid malposition evaluation can also be performed under slit-lamp guidance for increased magnification. Puncta placement and size should also be evaluated with care to see if the puncta are occluded by the caruncle or semilunar fold in resting position. The quality and health of the conjunctiva and cornea should be determined.
 |
Once the primary examination is complete, the examiner should have a good idea whether the tearing is an anterior segment problem, eyelid position problem or lacrimal drainage problem.
Based on this assessment, secondary tests can be performed. For patients with dry eye, Schirmer’s testing after anesthesia is most helpful. Patients who have tearing in the setting of dry eyes usually have decreased basal tear production, and this test is best for evaluating a deficiency.
For an eyelid malposition problem, eyelid taping has been described as helpful.1 In this case, tape is placed along the lateral aspect of the eyelid and used to tighten and displace the lid superolaterally.If the eyelid position is improved and the tearing symptoms seem better, then eyelid surgery will likely be helpful.
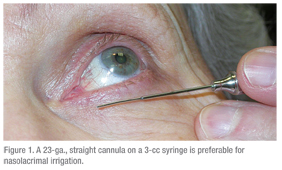
For lacrimal outflow problems, probing and irrigation is most helpful.2 To have reproducible and informative results, it is important to have the proper equipment. I prefer to use a 23-ga., straight lacrimal cannula (See Figure 1). If you use anything smaller, like an anterior segment cannula, the pressure required to pass through the cannula may be too high or water may flow around the cannula, giving you a false-positive result. The size is also helpful because if significant dilation of the puncta is required to pass the cannula, then punctal stenosis is part of the problem.3 A straight cannula is also helpful because the presence of stenosis in the canaliculus can be assessed.
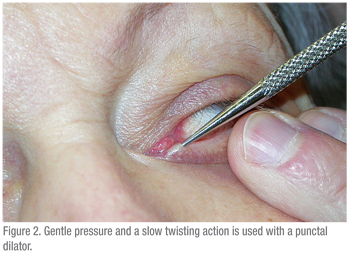
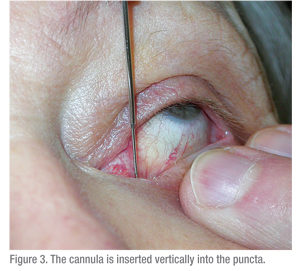
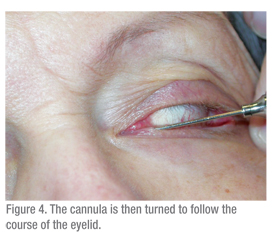
A 3-cc syringe should be used to pass water through the lacrimal system. A larger syringe (5 cc or higher) would require significant force to pass water though the cannula. A smaller syringe leads to the opposite problem: a TB syringe makes pushing water too easy and so obstructions are difficult to detect. Technique is also important. The ocular surface should be numbed and a cotton swab with anesthetic should be held between the puncta for a few minutes to help with discomfort. Then the patient should be instructed to gaze upwards, when testing the lower eyelid. The eyelid should be placed on stretch laterally and the dilator (if needed) should be passed vertically into the puncta and then turned to follow the course of the eyelid horizontally (See Figure 2). When dilating, gentle pressure is placed with the dilator and a slow twisting motion can be helpful. The cannula should be inserted in a similar fashion (See Figures 3 & 4). If using a straight cannula, it can be passed medially until a hard stop is gently felt. This confirms that the canaliculus is patent, since the cannula was able to pass all the way to the medial wall of the orbit. If a soft stop is encountered, where the cannula cannot pass completely into the canaliculus, then a canalicular obstruction is likely.
 |
 |
Finally, the nasal passage should be visualized. Using a nasal speculum and a muscle lamp or indirect headlamp light source is appropriate.
The presence of a mass, major nasal septal defect or nasal mucosal inflammation should raise the possibility of nasal pathology and generate referral to an otolaryngologist.
Once the cause of the tearing is determined, the treatment should be focused at improving or reversing the problem. Anterior segment problems such as dry eyes or blepharitis should be medically managed. Eyelid malpositions, if significant, should be addressed with surgical repositioning and tightening of the eyelid. Nasolacrimal obstructions should be addressed based on the specific anatomical defect. Punctal stenosis can be addressed via punctoplasty. Canalicular stenosis or obstruction often requires canalicular trephination, direct excision of scar and reconstruction with silicone stenting, or Jones tube placement (conjunctivo-dacryocystorhinostomy). For partial nasolacrimal duct obstructions, balloon dilation of the nasolacrimal duct with silicone intubation can be effective. For complete obstructions, dacryocystorhinostomy via an external or end nasal approach is appropriate. In patients who are not good surgical candidates or may be refractory to other interventions, botulinum toxin A injections to the lacrimal gland are useful. Finally, many patients will have multiple factors contributing to their tearing. In these cases, a stepwise approach is key, to address simple things first and proceed with focused surgery as needed.
Epiphora is a common ophthalmic complaint that can be caused by anterior segment, eyelid and lacrimal drainage pathology. Although it may be easy to get overwhelmed assessing these patients, with a thorough history and examination, the problem is often elicited, leading to the appropriate therapeutic intervention.
Dr. Bernardino performs oculoplastics and aesthetic surgery at Vantage Eye Center and has a special interest in eyelid and orbital tumors, lacrimal dysfunction, thyroid eye disease, and rehabilitation after loss of an eye. Contact him at rbernardino@vantageeye.com.
1. Cannon PS, Sadiq SA. Can eyelid taping predict the benefit of a lateral tarsal strip procedure in patients with eyelid laxity and functional epiphora? Ophthal Plast Reconstr Surg 2009:25;194-6.
2. Guzek JP, Ching AS, Joang TA, Dure-Smith P, et al. Clinical and Radiologic Lacrimal Testing in Patients with Epiphora. Ophthalmology 1997:104;1875-81.
3. Kashkouli MB, Beigi B, Murthy R, Astbury N. Acquired external punctal stenosis: Etiology and associated findings. Am J Ophthalmol 2003:136:1079-84.



