“More doctors are now paying attention to dry eye because there’s more we can do about it,” notes
David R. Hardten, MD, director of refractive surgery for Minnesota Eye Consultants and Regions Hospital, and adjunct associate professor of ophthalmology at the University of Minnesota. “There are more diagnostic tests, more treatments and more evidence that appropriate management reduces some of the long-term disability that comes with the disease. We now have tests for factors such as MMP-9 and osmolarity, and ways to image and quantify the tear film and condition of the meibomian glands. These allow us to monitor any ongoing damage, as well as any response to our treatments.
“The problem is that there are now too many diagnostic tests relating to dry eye for us to do them all,” he concludes. “It would take all day.” That reality has led many surgeons to wonder which tests and devices they should be using, and in which circumstances. Here, to help address those questions, a number of doctors who are using these tests and instruments share their experiences and what they’ve learned from using them.
Measuring Factors in the Tears
 |  |
| Two tests that are becoming more widely adopted for dry-eye testing are the TearLab osmolarity test (left) and the InflammaDry test from Rapid Pathogen Screening (above). The TearLab test provides a quantitative analysis of a tear sample’s osmolarity; the InflammaDry provides a gross measurement of the inflammatory marker matrix metalloproteinase-9, indicating the level of inflammation present in a tear sample. |
Kenneth A. Beckman, MD, FACS, director of corneal services at Comprehensive EyeCare of Central Ohio, and a clinical assistant professor of ophthalmology at Ohio State University, notes that there are multiple forms of dry eye, so he uses different tests in different circumstances. “I use the osmolarity test on every patient that I’m evaluating for dry eye,” he says. “It’s a quantitative test. It’s really good at detecting, grading and monitoring dry eye.
 |
| Advanced Tear Diagnostics’ TearScan system measures levels of lactoferrin, associated with the level of aqueous tear production, as well as the level of IgE, an allergy-related marker. A sample is placed into the vial (left) for dilution; the pipette at the top tranfers the correct amount of fluid to the test cassette. The cassette is inserted into the TearScan Reader to get numeric results. |
“It’s also really good at monitoring response to treatment,” he adds. “If I start a patient on Restasis and the patient’s osmolarity goes down from 360 to 310 to 295, I know the patient is getting better. It’s probably one of the best markers out there for monitoring treatment.”
Dr. Beckman also uses the InflammaDry test. “InflammaDry tests for the inflammatory marker MMP-9, which is present in higher quantities in an eye with inflammation,” he says. “I use this when I’m trying to determine how bad the inflammation is on the eye’s surface. In an eye with a lot of inflammation I’ll typically start the patient on Restasis, and maybe a steroid, too.”
Dr. Beckman notes that he doesn’t use the InflammaDry test at every dry-eye patient evaluation. “There are many situations in which I would use it, however,” he says. “If the patient has been referred for dry eye, is scheduled for a dry-eye consult, and the patient’s previous doctor has been dealing with this for a while and the patient is not getting better, I’ll use the InflammaDry test at the initial visit. On the other hand, if someone just comes in for a regular eye exam and happens to mention dry-eye symptoms, my staff will do an osmolarity test on the spot, but we won’t necessarily do an InflammaDry right away unless my clinical findings suggest it’s appropriate. Typically, I may do it on the next visit.
“One of InflammaDry’s most powerful applications is when I’m trying to decide whether I’m going to treat a problem with medications or punctal plugs,” he continues. “In that situation I use both the InflammaDry and the Schirmer’s test. I prefer not to put a punctal plug in an eye with a significant amount of inflammation, indicated by a positive MMP-9 result, especially with a high Schirmer’s score. I don’t want to conserve the tears if the tears are full of inflammation; that’s like bathing in dirty bathwater. So before proceeding with punctal plugs I like to see a negative InflammaDry and a low Schirmer’s score. It’s worth noting, however, that if I get a high score on Schirmer’s, I’ll repeat the test later to make sure it was valid; you can get a lot of false negatives with the Schirmer’s test.”
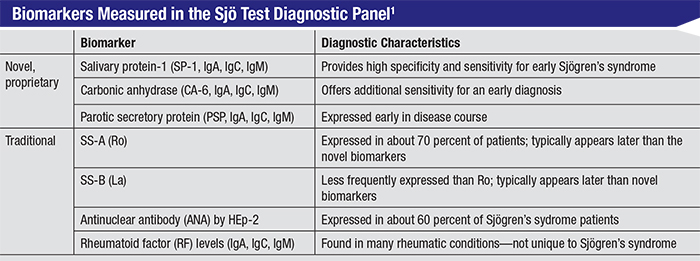 |
| According to Bausch + Lomb, the biomarkers measured by the Sjö test allow earlier identification of Sjögren’s syndrome than previous tests. Clinicians say that earlier identification and treatment by a rheumatologist may also improve dry-eye symptoms. |
Dr. Beckman adds that your staff has to know how to use the InflammaDry test. “As with most tests, you can get a false negative if the technician doesn’t take a good sample,” he says. “It’s also important to make sure the patient didn’t receive drops before this test was done. I’ve never seen a false positive, but I have seen eyes that looked really inflamed and had a false negative.”
Young Choi, MD, medical director at InVision Ophthalmology in Homewood, Ala., has used the TearScan system, which indicates the level of aqueous production, for a couple of years. “I use this test in the initial workup and monitoring of dry-eye patients,” he explains. “I’ll also use this test in select LASIK patients to confirm good candidacy. Furthermore, I use this test for my allergy patients because it provides the IgE level.
“The lactoferrin level is a quantitative test, so not only does it confirm the existence of dry eye secondary to aqueous deficiency, more importantly it indicates the level of severity with an actual number,” he continues. “This is very helpful. Patients like not only seeing an actual number indicating the severity of the aqueous deficiency, but also seeing that our treatment plan is changing that number—in other words, seeing that the treatment is working.” In terms of the test’s limitations, Dr. Choi notes that it doesn’t help in cases of evaporative dry eye.
Mixing and Matching
Like many surgeons managing dry eye, Christopher J. Rapuano, MD, director of the cornea service and co-director of the refractive surgery department at Wills Eye Hospital, and professor of ophthalmology at the Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, uses both the osmolarity test and the InflammaDry. “First, we often do the tear osmolarity test,” he says. “If the osmolarity is on the high side, that supports the diagnosis of dry eye. If it’s relatively normal, then I’ll begin looking for other explanations.
We also sometimes use the MMP-9 test,” he continues. “That’s basically a litmus test; it turns pink or red if your tears contain a significant amount of MMP-9, which is an inflammatory marker. There is a midrange; if it’s pink, it’s mildly positive; if it’s really red, it’s very positive. If there’s a lot of inflammation, then it’s possible that topical steroids will be necessary to get the patient over the hump. If there’s not much inflammation, then topical anti-inflammatories may not be the best way to go.”
Some surgeons use the tests in the reverse order. “When new patients come in, we give them a questionnaire that includes questions about symptoms of dry eye,” explains FrancisMah, MD, who specializes in cornea, external disease and refractive surgery at Scripps Health System in San Diego. “We can’t really do testing without a complaint of dry eye, but if patients give a positive answer to one of those questions, then we’ll start testing.
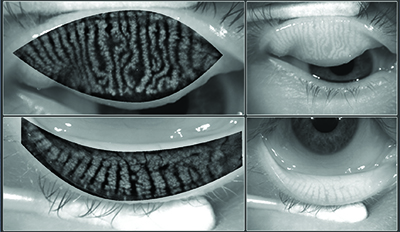
 |  | |
 | The LipiView II device (TearScience) uses high-definition transillumination combined with non-contact surface illumination to visualize the condition of the meibomian glands, without glare. The device can also evaluate blink rate and lipid layer thickness. Above, left: normal meibomian gland structure. Above, right: shortened glands and gland loss. Left: Significant gland loss. | |
“The next step is usually the Tearlab osmolarity test,” he continues. “In general, the patients who have elevated osmolarity are more likely to have issues with their ocular surface and dry eye, so if the osmolarity is high, I look more closely at the meibomian glands and the aqueous. But like the inflammation test, we don’t use the osmolarity test as a diagnostic tool; we use osmolarity more as a follow-up management tool, kind of like measuring a diabetic patient’s blood sugar levels or a glaucoma patient’s intraocular pressure. IOP isn’t diagnostic for glaucoma, but there is likely to be a correlation, and the same is true for osmolarity. We don’t live or die by the number at any given visit, but it is a guide.”
“It’s worth noting that these tests must be done before examining the patient, before giving him any drops and before checking his pressure,” adds Dr. Rapuano. “So if I decide that a test is worth doing, I’ll tell the patient to alert the technician that he needs this test as soon as he arrives for his next visit.”
Dr. Mah points out that several companies are working on tests using other markers. “One promising idea is testing multiple markers at the same time,” he says. “Combining some of these markers could potentially improve the yield in terms of the specificity and sensitivity of testing for ocular surface disease and dry eye. If two factors are shown to be abnormal, that significantly increases the likelihood of identifying and diagnosing an ocular surface disease.”
Testing for Sjögren’s
Another addition to the armada of dry-eye evaluative tests is the Sjö test, currently available from Bausch + Lomb. Dr. Beckman uses the Sjö test. “Sjögren’s syndrome is an underdiagnosed disease that can not only cause dry eye but has other systemic manifestations such as lymphoma,” he says. “If I’m treating for dry eye and the patient is not responding to conventional treatment as I would expect, I’ll do the Sjö test. I’ll also do the test if the patient mentions other symptoms that make me think of autoimmune disease, such as complaining about dry mouth or arthritis.
“I like the Sjö test better than traditional Sjögren’s tests because it has early biomarkers that may pick up the disease much more quickly,” he continues. “A number of my patients who suffered from dry eye for a long time and did not respond to conventional treatment had negative results when they took traditional Sjögren’s tests. But when I did the Sjö test, they had positive biomarkers that led us to confirm the diagnosis and send them to a rheumatologist for management.
“This is valuable for a number of reasons,” he points out. “By identifying the disease you can get the patient into the care of a rheumatologist. These patients are going to need to be monitored for life to watch for other systemic manifestations, including lymphoma. And although many rheumatologists used to think there wasn’t much that could be done for these patients, that’s no longer the case. There are medications that help with the saliva component, and anecdotally, I have a number of dry-eye patients who have been treated systemically for Sjögren’s or other autoimmune diseases whose eyes are getting better. We don’t typically put people on Plaquenil for dry eye, for example, but I have a number of Sjögren’s patients who are being treated with Plaquenil, and they say their dry eye is improving. In our experience, getting the autoimmune disease under control can really help the dry-eye symptoms.”
Dr. Rapuano also uses the Sjö test. “When it first came out, it was a finger-stick test that we did in the office,” he recalls. “That was convenient in the sense that the patient didn’t have to go elsewhere to take the test, but we had a very high percentage of ‘insufficient quantity’ results. So we’d stick patients, make them wait a week or two for the result, and then it would say ‘no answer.’ Patients were not very happy about that.
“The company has now gotten labs to agree to do the test using a blood draw,” he continues. “Even with the pinprick version of the test we had some positive results, but we’re getting more quality testing with the blood test. Most important, we always get an answer.
“I now use the Sjö test if I have a suspicion of Sjögren’s—even a small suspicion,” he says. “In addition to dry eye, the number one symptom I look for when I suspect Sjögren’s is dry mouth. If a patient has that and dry eye, then I ask him or her about other rheumatoid-type symptoms. I explain what Sjögren’s is, that it can be slow-onset and that lots of other systemic issues can go along with it, including dental issues, vaginal issues and cancer concerns.”
Dr. Rapuano says that in the past, if he suspected Sjögren’s syndrome, he would often tell patients to see their rheumatologist. “However, rheumatologists aren’t that eager to see dry-eye patients if there’s no diagnosis except ‘dry eyes,’ ” he says. “They’re much more willing to see these patients if they have a positive Sjö test. And a lot of the current blood tests, like SS-A, SS-B and rheumatoid factor, don’t pick up Sjögren’s very early. The Sjö test seems to pick it up earlier, and if you can pick it up earlier, then patients can seek treatment earlier. The earlier they get monitored, the better.”
 |
 |
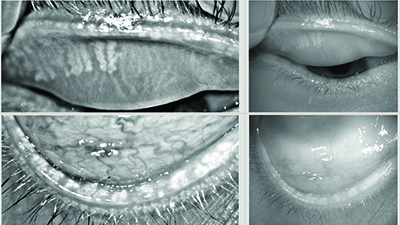 |
| The Oculus Keratograph 5M is a corneal topographer with a built-in keratometer and a color camera optimized for external imaging; it can be used to measure tear-film breakup time and tear meniscus height, to evaluate the tear film’s lipid layer and to visualize the meibomian glands, with or without digital enhancement. Above, top: Healthy meibomian glands imaged by the Keratograph; middle: severe meibomian gland dropout; bottom: digitally enhanced images of meibomian glands. |
Analyzing Other Factors
Several instruments now allow doctors to measure and analyze different aspects of the tears and eye that are relevant to managing dry eye. These include the Oculus Keratograph, which allows meibomian gland imaging and measures the lipid layer and tear film meniscus, and the Lipi-View system from TearScience.
“The LipiView instrument images and measures the patient’s lipid layer thickness with sub-micron accuracy, and analyzes it’s stability or early breakup,” says Vance Thompson, MD, who practices at Vance Thompson Vision/Sanford Health in Sioux Falls, S.D., and is assistant professor of ophthalmology at the University of South Dakota School of Medicine. (Dr. Thompson addresses dry eye most often in the context of refractive and cataract patients. His practice uses the LipiView II—the most recent model.) “Having this objective measurement is helpful for both diagnosis and measuring treatment effect over time. It allows us to measure and document the patient’s blink rate and behavior, and it also gives us, for the first time, a clinically useful way of imaging meibomian gland structure. LipiView has been a tremendous asset to our dry-eye center.”
Dr. Thompson says that to ensure that LipiView provides accurate information, patients need to be educated about what not to do before the measurement. “Eye rubbing is one of a number of things that can negatively affect the tear thickness measurement,” he notes. “That gives us an opportunity to remind patients that eye rubbing can have negative side effects. Patients are also instructed not to swim in chlorinated pools the day of the evaluation, since this can throw off the measurement. Certain ophthalmic drops can affect the accuracy of the measurement, so patients are instructed not to use oil-based drops like Restasis the day of the measurement, and not to instill ointments for at least 24 hours prior. It’s also important for contact lens wearers to remove the lenses a minimum of four hours before the measurement. Cosmetics that are oil-based should also not be used around the eyes on the day of the measurement.”
Dr. Rapuano’s office currently uses the original LipiView I device. “It uses interferometry to look at the lipid layer of the tears,” he notes. “Unfortunately, we haven’t found that function to be especially helpful. However, the instrument also records a video of the eye during blinking, and we’ve found that rather useful for diagnosing partial blinkers. Of course, taking care of or resolving partial blinking isn’t easy, but at least if you’ve diagnosed it you have something to go after when other things aren’t working.”
Dr. Rapuano believes the ability to look at the meibomian glands using the LipiView II should be helpful. “If the eye has very healthy meibomian glands, then the problem may not be a posterior blepharitis evaporative issue,” he says. “If the eye has very unhealthy meibomian glands, then you know that you need to do as much as you can to save the glands that are working. And if you can show the patient a picture revealing that his meibomian glands are only 50 percent of what they should be, the patient may be a little more aggressive with his posterior blepharitis treatments.”
How the Tests Fit in
Surgeons using these tests emphasize that they need to be used in the context of a broader evaluation, including the traditional approaches to evaluating the patient. “Being suspicious of dry eye in every surgical patient and making it a diagnosis of exclusion has helped my postoperative results tremendously,” notes Dr. Thompson. “But since there is no single symptom, exam finding or test result that you consistently see when diagnosing dry eye, you have to rely on putting these factors together. You have to rely on the whole picture.”
Dr. Beckman agrees. “All of the dry-eye tests work hand-in-hand,” he says. “I still do Schirmer’s, tear breakup time and cornea and conjunctival staining. You need to use all of them to come up with a good dry-eye assessment.”
“Just sitting there and listening to your patient is one of the most powerful ways to diagnose dry eye,” notes Dr. Thompson. “Even when I’m talking to patients I’m looking at their tear film reflectivity from a distance, looking for redness, assessing how much they blink during our conversation and even estimating their tear lake. I’m amazed how often you can be suspicious of dry eye before you look with the slit lamp or do a single test. Nevertheless, we know that symptoms and an exam fail to uncover many dry-eye patients. That’s why I appreciate the companies that have brought us testing for tear osmolarity, tear inflammatory markers and meibomian dysfunction. I wish I could use all of them on every patient, but for practical reasons we primarily do the TearLab osmolarity measurement. It’s easy to do, fits well into our clinic flow and give us good data. But we do find value in having all three of the devices that we use. All of them play a major role.”
Dr. Rapuano also sees the recent point-of-service tests as only one part of the dry-eye diagnostic process. “Over the years, we’ve learned that there are many different forms of ocular surface disease that can cause dry-eye symptoms,” he says. “These can range from insufficient tear production to anterior or posterior blepharitis to conjunctival chalasis. So when faced with potential dry-eye patients, I begin by asking about their symptoms. Are they worse in the morning or do they get worse over the course of the day? Are they worse in windy conditions? Then I do a slit-lamp exam. That may reveal lashes poking in, entropion or ectropion or partial blinking. I look at the health of the cornea and conjunctiva and tear meniscus. I look for conjunctival chalasis. I check for corneal fluorescein staining, measure tear-film breakup time and often do a Schirmer’s test. I may also do conjunctival staining with lissamine green.
| |
|
Dr. Hardten notes that it’s helpful to think of these tests as being short-term or long-term tests. “Dry eye is like glaucoma—it’s an ongoing disease that fluctuates over time,” he says. “It’s hard to tell from one day to the next what’s real. So, we use a combination of short-term and long-term testing. For dry eye we have short-term tests like osmolarity and long-term tests like examining the meibomian glands using tools such as the Keratograph or LipiView. These instruments allow infrared imaging of the meibomian gland structure, making it possible to follow the health of the glands long-term. This can help the eye-care provider analyze whether there is significant damage to the meibomian glands, helping to further distinguish evaporative tear-film
deficiency from aqueous-deficient dry eye. Testing the short-term things, such as osmolarity, is like monitoring IOP in glaucoma. You check the intraocular pressure, but you also look at the optic nerve and visual field.”
Finding the Best Option
Dr. Rapuano says no one test is currently sufficient to diagnose the cause of dry eye. “Diagnosis usually comes from evaluating symptoms, a thorough slit-lamp exam and some of these tests,” he says. “They all go together. It would be nice to have one litmus test to give us a yes or no answer about the cause, but we don’t have one. My guess is that we never will, because the causes of dry eye are not a single diagnosis. This is not a pregnancy test-type situation.”
Dr. Mah agrees. “I think in dry eye we’re talking about multiple entities,” he says. “Until we can separate out all the ocular surface issues that are labeled dry eye, I don’t think we’ll have one single test that will be universally diagnostic.”
Given those qualifications, if you’re in the market for a dry-eye test, what is most likely to be clinically useful? Dr. Mah notes that companies tend to say that their test is the one every practice needs to use. “To determine the value of these tests, it helps to read the literature,” he says. “Look at the information and clinical trials associated with a given test. Also, realize that while these tests are all helpful in some way, they all have limitations. You need to know what each test can and cannot do for you, and use it accordingly. Finally, don’t give up on using the time-honored clinical tests. They are still valuable.”
“I think if you’re making a commitment to treat dry-eye patients, you need to understand what’s out there,” says Dr. Beckman. “That includes the more traditional tests that don’t require an instrument. From my perspective, if you’re committed to treating dry eye, I’d say it’s worth getting both the osmolarity test and the InflammaDry, because we use those tests all the time. If you’re dealing with complicated patients, I think the InflammaDry test will give you a lot of information to help direct your treatment.”
What about the cost factor? “The number of testing options you pursue will depend, in part, on how much money you’re able to invest in this area,” notes Dr. Rapuano. “The osmolarity test is probably the one that will give you the most bang for the buck. The MMP-9 test can also be helpful in some patients. Those tests involve very little up-front investment; you need to buy the tests, but you usually get reimbursed enough to cover the costs. You won’t lose money.”
Dr. Beckman agrees. “One of the good things about the more recent tests that do require equipment, like the osmolarity test, is that you can get the basic equipment for free; you just have to buy the cards,” he says. “That cost is usually reimbursed by insurance. None of these tests has a huge profit margin, but that’s not the point; they’re there to provide you with information to help you make good decisions and treat the patient properly. Meanwhile, you’re not going to lose money on them.”
“The Sjö test doesn’t cost the doctor anything, and it’s usually covered by insurance,” adds Dr. Rapuano. “Without insurance coverage it might cost a couple hundred dollars.”
In terms of investing in one of the more expensive instruments that can help with dry-eye analysis, Dr. Rapuano says if he were looking for one new instrument to help analyze the ocular surface he would probably choose one that images the meibomian glands, such as the LipiView II or Oculus Keratograph. “The LipiView II is a much bigger investment,” he admits, “but you can get reimbursed for imaging the meibomian glands.” REVIEW
Dr. Beckman is a consultant for Tearlab, RPS and Bausch + Lomb. Dr. Rapuano is a consultant for Tearlab and TearScience, and has a minor stock ownership in RPS. Dr. Mah is a consultant for Tearlab; Dr. Hardten is a consultant for Allergan. Drs. Thompson and Choi have no financial ties to any of the dry-eye companies.
1. http://www.bausch.com/ecp/our-products/diagnostics/sjo#.VfMtT-n-P8s. Accessed 11 September 2015.







