Adjusting the Lens
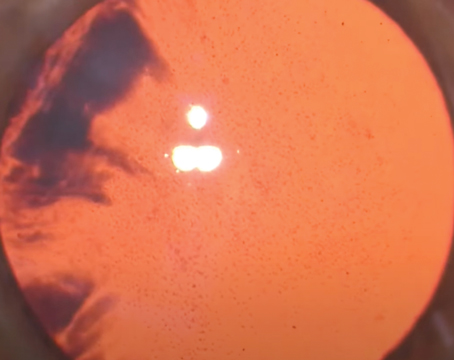
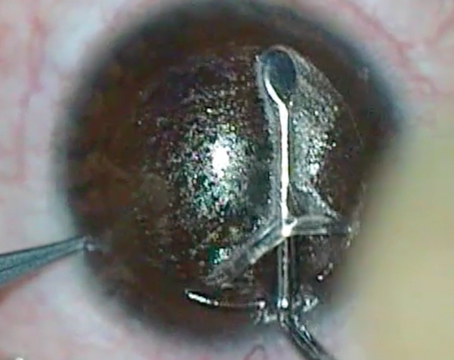
The LAL is a silicone lens composed of both stable material and photosensitive silicone macromers. When the lens is exposed to ultraviolet energy emitted by a special radiation device, the macromers polymerize in whatever shape or pattern is imposed by the radiation application. Non-polymerized macromers will then migrate to the area of the polymerized ones, causing the lens to enlarge in that area. This shape change is what alters the refractive power of the lens. This process, known as adjustment and lock-in, takes place during the period following the cataract surgery and implantation of the lens.
“The FDA protocol requires implantation of the IOL and a wait of 17 days to start the adjustment process,” says Indianapolis surgeon and LAL investigator Kevin Waltz. “The preop astigmatism is not treated during cataract surgery, and the refractive target at the time of cataract surgery is approximately +0.50. All post-implantation treatments are preceded by testing, including two independent refractions. The first treatment is called adjustment number one; it targets the cylinder and decreases the plus sphere toward zero. The next treatment is adjustment number two, and is used if some refractive error remains after adjustment one. If there is very little refractive error after adjustment one, we go directly to lock-in number one. The purpose of this lock-in step is to consume the remainder of the reactive macromer in order to stabilize and ‘lock’ the refraction. There is some inefficiency in lock-in number one, though, because, for technical reasons, it can’t consume all of the unused macromer. Lock-in one does draw all of the unused macromer into a part of the lens where it can be consumed, however, and lock-in two consumes all of the unused macromer that lock-in one does not. After lock-in two, the IOL power is fixed and stable.” At this point in its development, the lens can be adjusted to eliminate up to 2 D of spherical error and up to 2 D of astigmatism (which is 3 D of cylinder at the corneal plane).
During this adjustment process, it’s important for the patient to wear UV eye protection, since UV light can actually alter the lens before it’s shape is finally locked in. “We have some patients we suspect of being less than perfect with their UV protection,” says Dr. Waltz. “But it doesn’t appear to have harmed them, or to have had a serious adverse effect on the adjustment process. We don’t have any patients that we’ve confirmed as non-compliant with the UV protection requirement.”
Current Results
Calhoun Vision’s medical monitor R. Doyle Stulting presented results from one of the LAL investigational sites at the 2014 meeting of the American Society of Cataract and Refractive Surgery. The results he presented were after one adjustment. In the eyes presented, one week after lock-in, 83 percent achieved 20/20 or better uncorrected vision vs. zero who saw at that level before the adjustment, with a quarter of the eyes seeing 20/12 or better.
|
In terms of astigmatism control, after lock-in, 67 percent of the eyes had zero astigmatism. All of the eyes had 0.5 D or less of astigmatism (preop range: 0.5 to 1.75 D) post lock-in.
At Dr. Waltz’s practice, he notes that all of his patients, if done without the LAL, would have required a toric lens. “All patients in the FDA Phase III Calhoun trial must have between 0.75 and 2.25 D of anterior corneal astigmatism to enter the trial,” he says. “This makes them very challenging patients to achieve a plano endpoint. Given this, in my site’s experience, approximately one-third of our patients have uncorrected vision of 20/20 postop, one-third see 20/16 and a third see 20/12. There is an occasional patient with less than 20/20 after treatment, but it’s rare.”
Presbyopic Correction
Researchers and investigators are also using the UV light to make special aspheric adjustments to the LAL in a process called adjustable blended vision. The goal of these adjustments is to broaden patients’ range of vision.
Tijuana surgeon Arturo Chayet, who consults for Calhoun Vision, says the ABV treatment relies on inducing different levels of asphericity in the lenses. “First of all, we make sure the patient can see well for distance, because individuals like to have good distance vision,” Dr. Chayet explains. “We do that by making sure the dominant eye will have great distance vision, though we still give that eye a little negative asphericity so it can have the so-called ‘summation’ with the other eye, and have some improved intermediate acuity. Then, in the non-dominant eye, we’ll give high asphericity. The non-dominant eye will lose a little bit of distance vision because any time you create a multifocal effect or a different focus in one eye, the eye loses a little at some focal distance. Basically, the eye will go from 20/20 to 20/25 in order to gain near vision. Typically, that eye will be able to see between J2 and J3. If the patient wants J1 because his lifestyle requires very good vision at, say, 40 cm, then you can leave that eye around -0.5 D. The patient will still have very good intermediate vision, and the eye will typically have an uncorrected vision between 20/30 and 20/40. The difference between the eyes is well-accepted by the brain, as opposed to the typical monovision treatment in which there is more than a 1.5-D difference between the eyes.”
In a study of binocular vision results in 20 ABV patients at Dr. Chayet’s practice, 75 percent could see 20/16 or better at distance after lock-in. Eighty-five percent now see 20/20 or better and 100 percent see 20/32 or better. In terms of binocular intermediate vision at 60 cm, 60 percent see J1+ versus zero patients preop, 75 percent see J1 versus 20 percent at this level preop and 100 percent see J2 or better compared to 45 percent preop. Ninety percent see J2 or better binocularly at near (40 cm) versus 15 percent preop. Fifty-five percent now see at least J1, compared to 5 percent who could see that well preop.
“Right now, I think we’re learning a lot about how to present the technology to patients and create the right expectations in them,” says Dr. Chayet. “This is a new technology and, as with any new technology, we’re learning more about it, but we’re making very good progress.” REVIEW