Though LASIK, PRK and SMILE are popular, effective options for many patients, not everyone is a candidate for them. As an alternative, patients and their surgeons can turn to phakic lenses such as the EVO implantable collamer lens and the Artisan phakic intraocular lens, though taking the intraocular surgery route opens up a new level of challenges and possible pitfalls.
If you’re looking to start implanting phakic IOLs—or are already involved with their implantation but would like to hear some new tips and tricks—read on to learn expert surgeons’ best practices.
 |
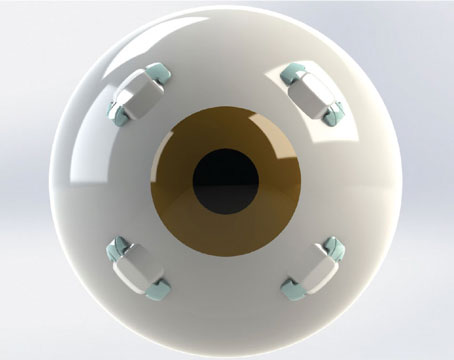
| Currently undergoing FDA trials, the Artiflex PIOL uses iridoplastic bridges, similar to the Artisan PIOL, to clip it to the iris. Instead of a rigid design, the Artiflex is foldable, meaning smaller and less invasive incisions. |
First Steps
Consulting with patients prior to the procedure is key, and ensuring the patient is well educated can help ease the process later on. “These patients don’t usually have any prior knowledge of phakic IOLs,” says Majid Moshirfar, MD, Research Medical Director at Hoopes Vision Research Center, professor of ophthalmology at John A. Moran Eye Center at the University of Utah School of Medicine, and medical co-director at Utah Lions Eye Bank.
“They visit my clinic because they all think that they’ll be able to get procedures in terms of corneal surgery: PRK; LASIK; SMILE. But, when we realize that they don’t have the capability to undergo those surgeries, either because of their baseline refractive error or perhaps they have inherent corneal external disease, we usually have to tell them that corneal refractive surgery isn’t a viable option. Then, I tell these patients to look into an alternative, which is more of an additive procedure. That’s when we talk about phakic intraocular lenses.”
Once the patient understands the procedure and shows an interest, surgeons then go into the possible operative and postoperative outcomes. “You need to talk with a patient prior to the surgery about these things,” says Dr. Moshirfar. “I usually give them the informed consent that’s provided by the company itself, but I still have a face-to-face with them and I try to explain all the possible outcomes.
“I think the common complications that we need to share with our patient is perhaps an oversizing or undersizing of the lens, and perhaps lack of efficacy in astigmatic correction,” continues Dr. Moshirfar. “Sometimes these lenses rotate slightly, and patients may need to have an enhancement for the residual refractive error. Otherwise, macular edema, iris inflammation, pressure rise, endophthalmitis, retinal detachment and acute vitreous attachment are the rare things that can happen. I think clinicians need to share this information, but I think the common issues that need to be addressed are primarily sizing surprises.”
In regard to the Staar Surgical’s EVO/EVO+ ICL, the design of the lens can cause some issues that patients should be aware of before committing to the procedure. “I tell everybody in advance that they’re going to have a little glint when they look at lights, because the EVO has an opening at the center of the lens,” says Deepinder Dhaliwal, MD, professor of ophthalmology and chief of refractive surgery at the UPMC Vision Institute.
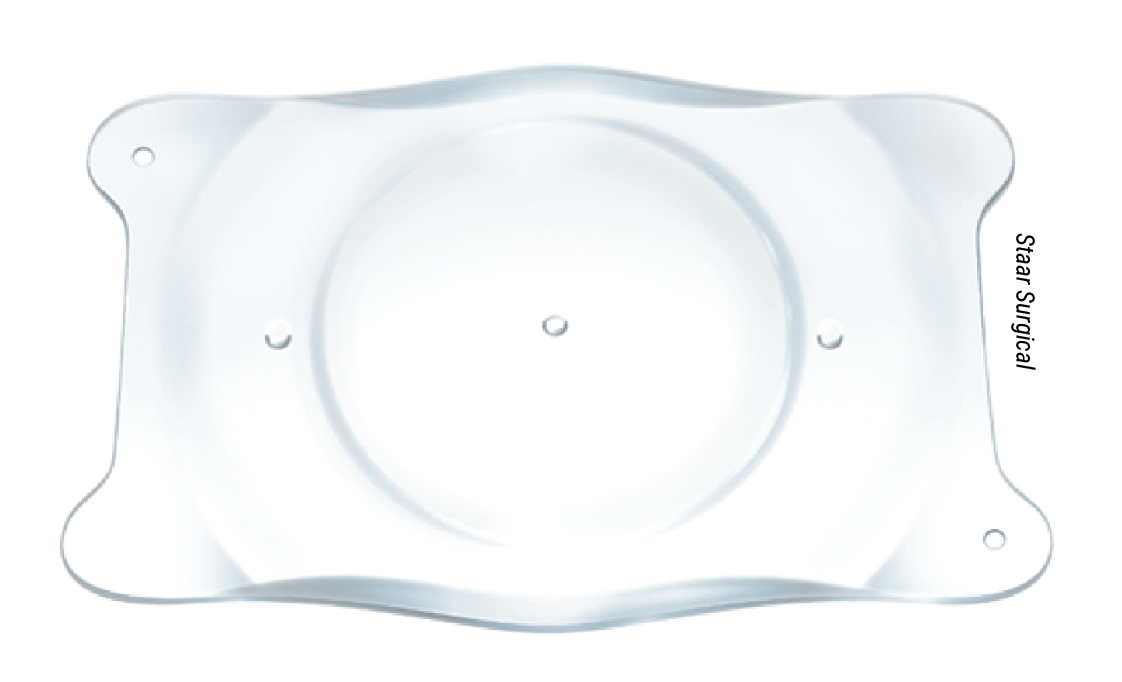 |
| The EVO/EVO+ ICL is indicated for the correction of myopia and astigmatism in patients 21 to 45 years old. Patients with moderate to severe glaucoma, a small anterior chamber angle and a thin endothelial cell layer aren’t candidates for this procedure. |
Choosing the Right Lens
In 2005, Staar’s Visian implantable collamer lens was approved by the FDA. This ICL was a minimally invasive foldable lens that corrected myopia ranging from -3 to ≤ -15 D with astigmatism of ≤ 2.5 D.1 Recently, Staar reintroduced the Visian on a new platform in 2022. The EVO/EVO+ Visian ICL is the latest advance in phakic lens technology, providing correction in high myopes ranging from -3 to -20 D.2 In patients with astigmatism, the EVO/EVO+ ICL can correct 1 to 4 D.2 Also, Staar notes on their website that the EVO+ is similar to EVO, but it’s an expanded optic.
“The reason people embrace the [EVO/EVO+] ICL is the fact that it’s removable technology,” says Dr. Dhaliwal. “It goes in their eye, and they can assess how they like it and if for some reason it’s not jibing with their optical system, or is incompatible for some reason, then they can have it removed.”
Additionally, when the Visian evolved into the EVO/EVO+ platform, they redeveloped the lens to eliminate the need for an iridotomy. “EVO has an opening at the center of the lens, which obviates the need for a peripheral iridotomy,” says Dr. Dhaliwal. “It allows aqueous humor to percolate through the device and bathe the crystalline lens so that the risk of cataract is much less.”
Dr. Dhaliwal summarizes the simplicity of the EVO/EVO+ ICL stating, “I make two paracentesis incisions and the main incision, and then I implant the EVO ICL. Then, I tuck in the little footplates underneath the ICL and remove the viscoelastic.” In a study to understand the applications of the ICL after FDA approval, researchers noted two techniques for incision size. Their standard technique used a 1-mm incision for insertion while their modified technique used a 3-mm incision. While the modified technique provided better results without adversely effecting endothelial cell density and reducing fluctuations in IOP, the standard technique didn’t increase surgically induced astigmatism.3
On the other side of the market, Ophtec’s Artisan phakic IOL, or Verisyse phakic IOL, was FDA approved in 2006. Ophtec describes this lens as a rigid lens with two iridoplastic bridges, or “claws,” that clip into the iris, putting it in the “iris claw lens” category. The lens’s maker says that it’s is offered with a 5-mm curvature with a dioptric range of -5 to -20 D, as well as a 6-mm curvature with a dioptric range of -5 to -15.5 D.
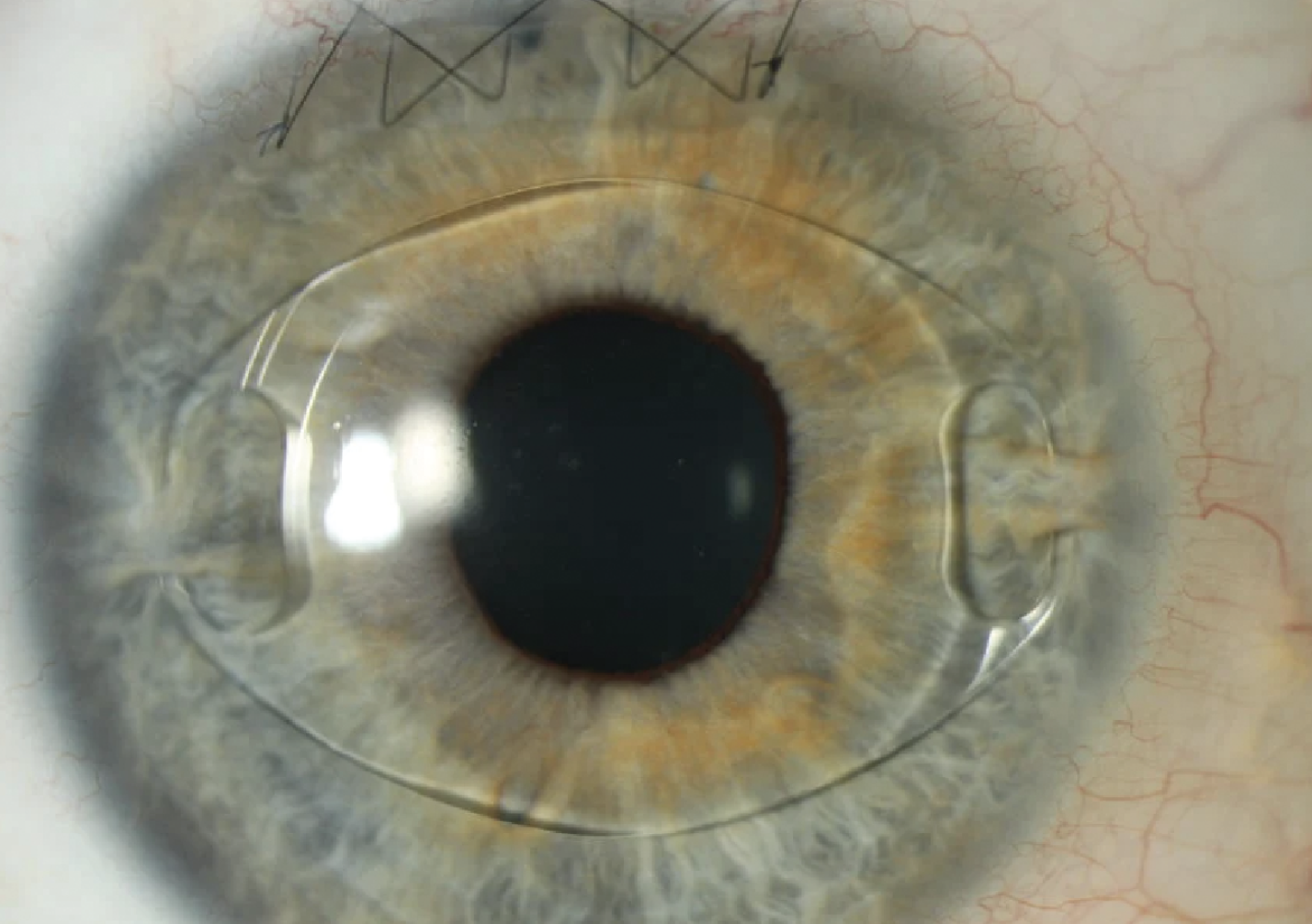 |
| Image of Artisan PIOL implanted into the eye. The lens is positioned in place to allow the “claws” to attach themselves to the iris. Then, the incision is closed with nylon sutures (seen at the top of the image). |
“I still would say on a yearly basis I do close to 80 to 100 ICL cases, but there are situations that, based on the anterior chamber integrity or the iris angle configuration, these patients end up getting the Verisyse lens,” says Dr. Moshirfar. Since the IOL material (polymethyl methacrylate) isn’t foldable or injectable, a 6-mm wide incision is needed to implant the IOL.4
Although all phakic lenses are indicated for myopia, Staar and Opthec offer specific lenses for high hyperopic patients. During a study for the Artisan Hyperopic phakic IOL, 26 eyes with a refractive error ranging from 3 to 11 D were observed over a three-year time period. At six months, most patients met the primary endpoint. Researchers noted that 90.9 percent of eyes were around +/- 1 D of intended correction and 81.8 percent were +/-1 D of emmetropia. Some patients experienced posterior synechiae with pigment deposits and one patient had convex irises. Within two years, the lenses implanted in the convex-iris patient were removed.5
Staar’s EVO/EVO+ ICL isn’t approved for hyperopia in the United States, but their Visian lens is still available and approved for hyperopic patients. In a study to examine the effectiveness of the ICL for both myopia and hyperopia, researchers implanted the ICL into 126 eyes between +8.88 and -20.5 D. Since myopia is more prevalent than hyperopia, only 10 hyperopic patients underwent implantation. The average hyperopia treated in these patients was 7.14 D.6
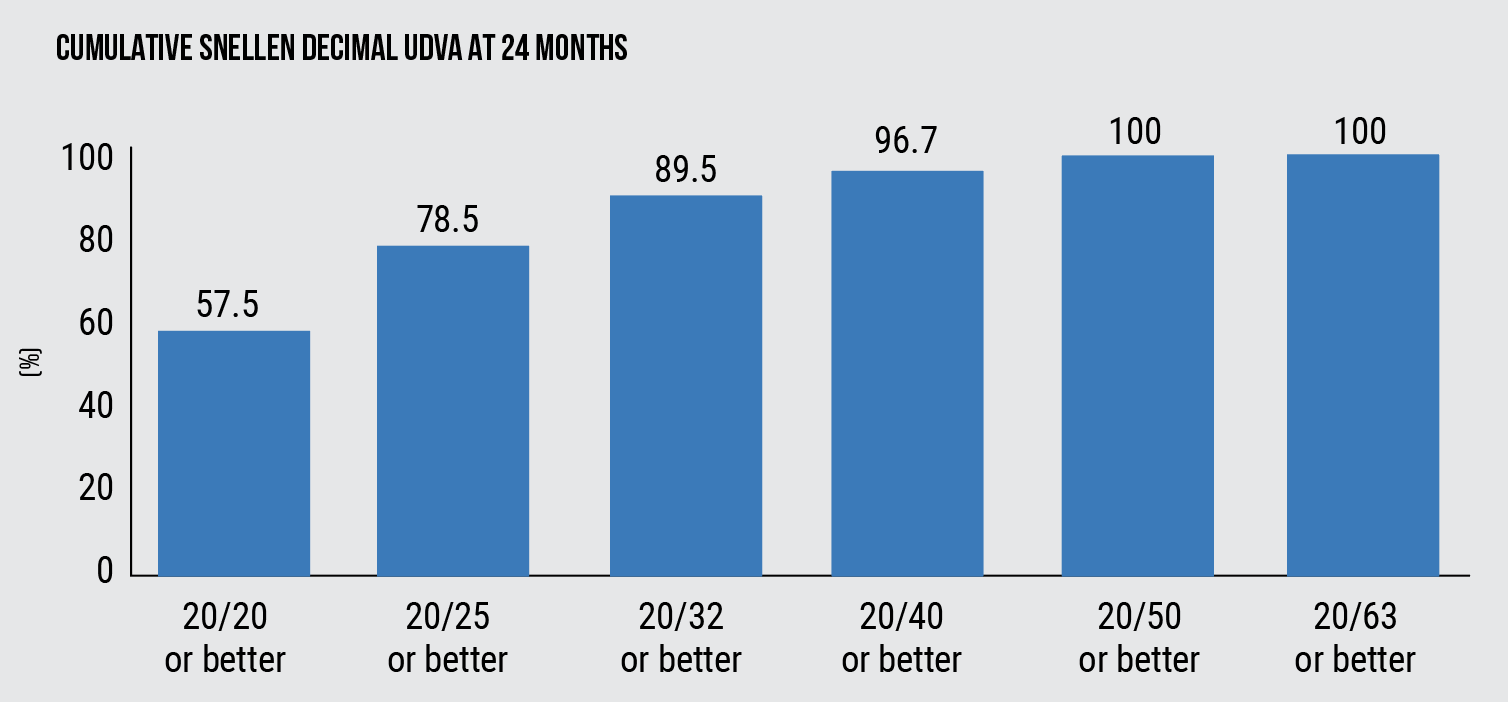 |
| Figure 1. The cumulative proportion of eyes having a given UDVA value at 24 months following implantation of an ICL with a central hole. Before surgery, all eyes had an UDVA worse than 20/63. |
Measure, Measure, Measure
Accurate preop measurement of the patient’s eye is crucial for properly sizing the ICL, surgeons say. Refractive surgeons note that there are several ways to get the most accurate results.
“This is a topic in a lot of conversations, and what I do is I use several devices for measurement,” says Dr. Dhaliwal. “What we realized is that you only need a manual caliper if you’re in between sizes. Basically, you can use any of your devices that you’ve vetted in your practice. We look at Pentacam, we look at the IOLMASTER and we look at other white-to-white measurements.”
Dr. Moshirfar, on the other hand, doesn’t attempt to find the white-to-white measurements, but rather measures the sulcus-to-sulcus distance. “The whole concept of measuring the white-to-white along the 100-degree meridian was the historical way that we did for the FDA approval stages of phakic lenses,” he says. “We don’t do that anymore. I personally have a UBM ultrasound that helps me measure the sulcus-to-sulcus. If somebody implants ICLs on a routine basis, then they should be looking at the parameters that they can obtain from the posterior chamber from the sulcus-to-sulcus.” Since the ICL is implanted into the ciliary sulcus, measuring the sulcus-to-sulcus is very important for predicting the size of the lens, surgeons say.7
Dr. Dhaliwal also determines the sulcus-to-sulcus measurement before operations, but she has a professional assist her. “[At UPMC], we have an imaging technician who records consistent results for our refractive surgery patients,” she says. “She’s doing ultrasound to get the sulcus-to-sulcus measurement.”
 |
| Courtesy Douglas Grayson, MD. |
Handling Patients Postoperatively
After surgery, refractive surgeons follow up with their patients several times postoperatively. “We usually see our patients on day one, and then between days five and seven, and then we again see them around week four,” says Dr. Moshirfar. “Then, we see them on month three, and then we see them again on months six and 12. After that, we still tell them to come back and see us yearly.”
Dr. Dhaliwal follows a similar routine with her patients, but she goes on to add, “I always check their pressure before they leave the ambulatory surgery center where I operate. I do a one-to-two-hour check of their ICL position and the pressure.”
Besides checking the pressure and the position of the phakic lens, there are other postoperative measures that surgeons check with their patients. “We also evaluate the vault,” says Dr. Moshirfar. “Postoperatively, these patients are still getting diagnostic images using anterior segment OCT so that we can look at the level of vault, which is basically the space between the ICL and the natural crystalline lens. As the years go by, that vault or separation space gradually gets smaller and narrower.
Also, we like to look at the lens to make sure these patients aren’t developing pigmentary inflammation in their eyes,” continues Dr. Moshirfar. “We also want to make sure they’re not developing premature cataracts. This group of patients is also at a higher risk of retinal detachment and inherently they’re at a higher risk for glaucoma being high myopes.”
There are unique cases that will need close monitoring. “I did have a nystagmus patient where the ICL rotated a little bit,” says Dr. Dhaliwal. “Due to this, it was really hard to implant and readjust the lens, but I didn’t think that was a big deal. As long as you have the right size ICL, that rotation becomes less of an issue. You just need to follow up with them preoperatively.”
In most cataract cases, the ICL will need to be removed. “Anything in contact with the anterior lens capsule causes cataract formation,” says Douglas Grayson, MD, medical director and chief cataract and glaucoma at Omni Eye Services. “With the foldable ICLs, you cut the lens, you rotate it out, and do your phaco, and you can do everything through a 2.4-millimeter self-sealing wound.”
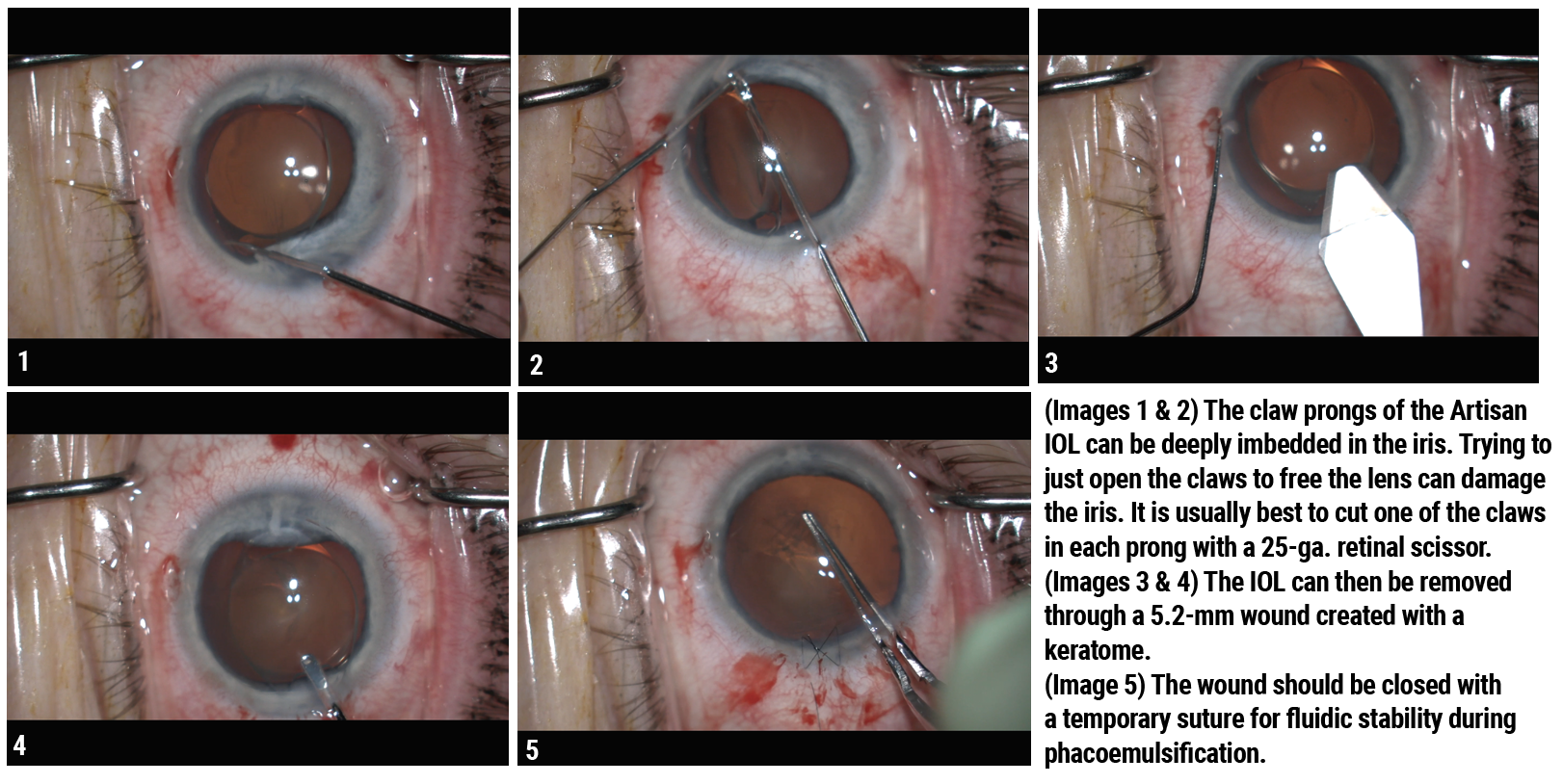
Artisan phakic IOLs aren’t easily removed before cataract surgery. Dr. Grayson explains how an Artisan lens could be explanted: “The rigid Artisan phakic lenses are tricky to remove because it’s very difficult to unclip the haptic from the iris,” he says. “Once you do that, you need a really large wound to take the lens out, because it’s rigid and it’s five millimeters. Then, after the lens is removed, you have to close that wound partially in order to perform phaco. So, you’ve got to suture the wound for phaco, then take that suture out and then go back in with sutures to close the wound after cataract surgery.”
Interestingly, for the EVO/EVO+ lens, Dr. Grayson has adopted a technique in order to perform femtosecond laser cataract surgery without removing the lens. “Femtosecond laser assisted cataract surgery is always a more advantageous way of performing cataract surgery, so just because an ICL is implanted, we didn’t want to deprive our patients of doing the femto.” To explain further, in a 2016 case report of two cases of cataract with phakic IOLs implanted, the surgeons concluded that the femtosecond laser can be used to create a capsulotomy and nuclear fragmentation through both anterior and posterior chamber PIOLs. Entrapment of cavitation bubbles beneath the ICL was noted in one case. The other case saw a successful femtosecond laser cataract surgery with an Artisan lens implanted. The surgeons explanted the phakic IOL at the end of the surgery by enlarging the temporal incision.8
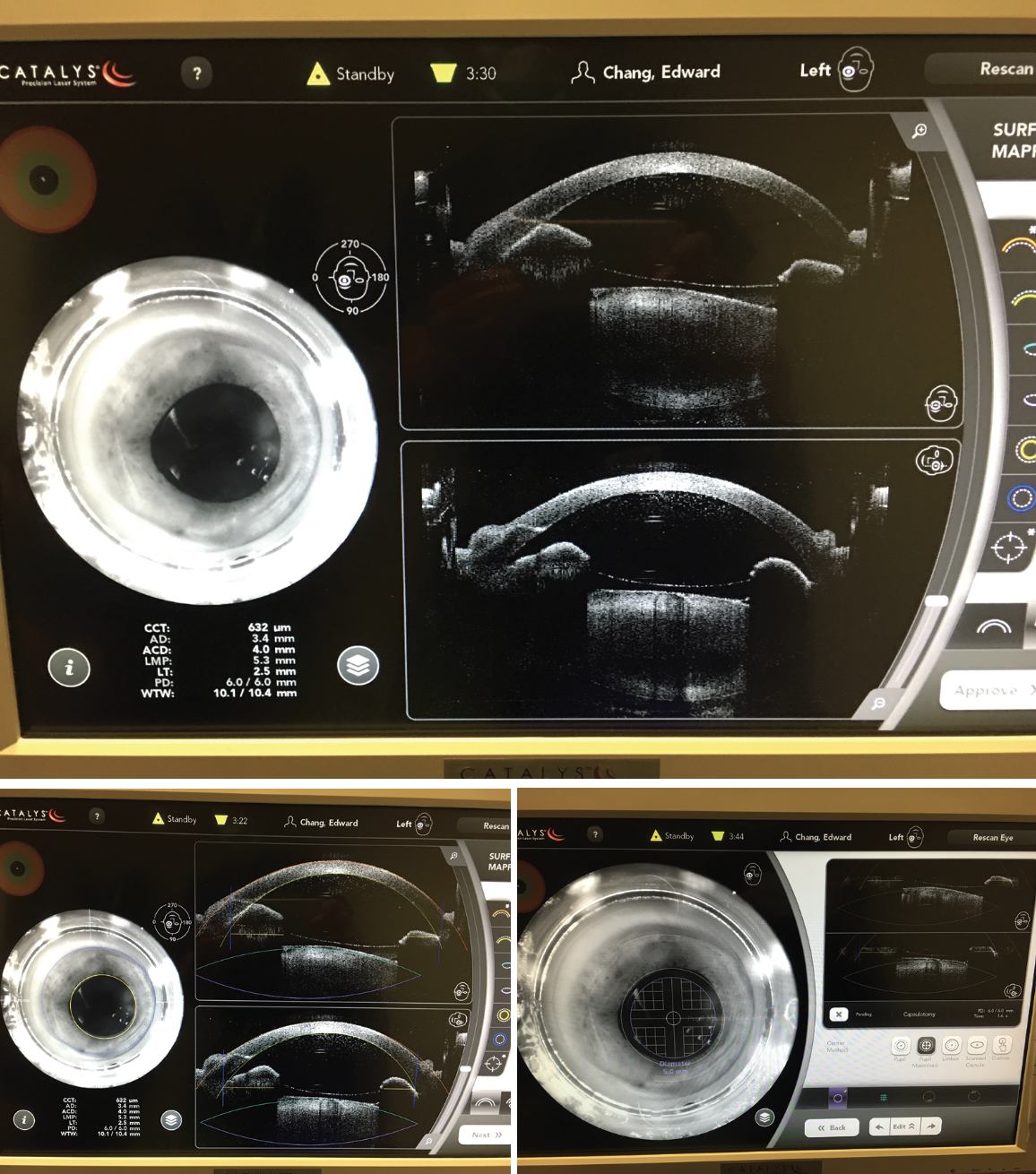 |
|
Femtosecond laser-assisted cataract surgery can be used in patients with ICLs. (Top) Initial scan shows a differentiation of the ICL and the anterior lens capsule. (Middle) ICL lying above the anterior capsule with green delimiting marker line synchronized with the anterior capsule. Manual readjustment of the anterior capsule delimiting line may be required. (Bottom) Successful femtosecond laser procedure including astigmatic cuts, capsulotomy, and lens softening. (Courtesy Douglas Grayson, MD) |
Future of Phakic Lenses
In other countries, Ophtec offers their Artiflex phakic IOL, a foldable lens for the treatment of myopia, which also comes in a toric platform. Currently undergoing FDA trials, Artiflex has been performing safely and effectively around the world for several years. In a 2012 study to evaluate the safety, efficacy and potential risks of the lens, researchers observed 78 eyes after a two-year period. After the time period, UCVA was 20/40 or better in 84 percent of the eyes. Adverse reactions such as pigmented and non-pigmented precipitates were observed in 17 eyes, which were treated with topical corticosteroids.9
According to Ophtec, the Artiflex requires a 3.2-mm incision. This product is mean to be “one-size-fits-all,” but Ophtec also notes that this treatment is reversible, therefore patients don’t have to commit to the lens. If the Artiflex were to make it to the United States in the future, the phakic lens market would have more unique treatments to treat high myopes.
Surgeons say perhaps the best practice is to thoroughly inform patients about the benefits and the risks of the surgery preoperatively. Says Dr. Dhaliwal, “I think the critical thing is preoperative management of these patients, so that you manage the expectations, because happiness equals postop reality minus preop expectations.”
Dr. Dhaliwal is a consultant for Staar Surgical. Drs. Moshirfar and Grayson have no financial interests to disclose.
1. STAAR Surgical’s VISIAN ICL(TM) receives FDA approval. STAAR Surgical 2005. https://www.staar.com/news/2005/staar-surgicals-visian-icltm-receives-fda-approval. (Accessed on 14 Nov. 2023)
2. STAAR Surgical announces U.S. FDA approval of EVO Visian implantable collamer lenses. STAAR Surgical 2022. https://investors.staar.com/press-releases/press-release-details/2022/STAAR-Surgical-Announces-U.S.-FDA-Approval-of-EVO-Visian-Implantable-Collamer-Lenses/default.aspx. (Accessed on 14 Nov. 2023)
3. Wang Y, Yang R, Huang Y, Zhang C, Liu H, Jia Z, Zhao S. Clinical observations of EVO-ICL implantation and changes in corneal astigmatism using a modified technique. BMC Ophthalmol. 2022 Sep 23;22:1:381.
4. 1792: Verisyse phakic IOL removal. Cataract Coach 2023. https://cataractcoach.com/2023/04/03/1792-verisyse-phakic-iol-removal/#:~:text=The%20first%20step%20is%20to,the%20eye%20(Figure%201). (Accessed on 13 Nov. 2023)
5. Saxena R, Landesz M, Noordzij B, Luyten GP. Three-year follow-up of the Artisan phakic intraocular lens for hypermetropia. Ophthalmology 2003;110:7:1391-5.
6. Rayner SA, Bhikoo R, Gray T. Spherical implantable collamer lenses for myopia and hyperopia: 126 eyes with 1-year follow up. Clin Exp Ophthalmol. 2010;38:1:21-6.
7. Zhu, QJ., Zhu, WJ., Chen, WJ. et al. A prediction model for sulcus-to-sulcus diameter in myopic eyes: A 1466-sample retrospective study. BMC Ophthalmol 2022;22:307.
8. Kaur M, Sahu S, Sharma N, Titiyal JS. Femtosecond laser-assisted cataract surgery in phakic introcular lens with cataract. Journal of Refractive Surgery 2016;32:2.
9. Ozertürk Y, Kubaloglu A, Sari ES, Koytak A, Capkin M, Akçay L, Evcili PS. Foldable iris-fixated phakic intraocular lens implantation for the correction of myopia: two years of follow-up. Indian J Ophthalmology. 2012;60:1:23:8.