These are just some of the results from this month’s e-survey on IOLs. The e-mail survey was opened by 1,315 of the 10,000 subscribers to Review’s electronic mail service (13 percent open rate) and, of those, 82 surgeons (6 percent) responded.
Presbyopic Lenses
Breaking down the popular option of presbyopic lenses, 46 percent use the AcrySof aspheric ReSTOR +3 D, 41 percent implant the Tecnis multifocal lens and 29 percent implant the Crystalens (some surgeons implant more than one of those lenses). Though they’re using the lenses, the surgeons aren’t implanting them with great frequency: On average, they implant an average of five ReSTOR lenses, eight Tecnis lenses and/or three Crystalens IOLs per month. The average charge for these premium IOLs on the survey is $1,884 for the ReSTOR, $2,015 for the Tecnis and $2,250 for the Crystalens.
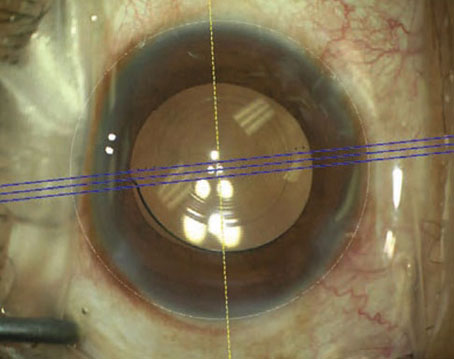
Surgeons appear to be satisfied with presbyopic lenses, with 31 percent saying they’re very satisfied, 36 percent identifying themselves as satisfied, 29 percent saying they’re somewhat satisfied and only 4 percent saying they’re unsatisfied. “Centration of multifocal lenses is key,” says Anil Shivaram, MD, of Claremont, Calif. “Also, do your due diligence to make sure the patient is a candidate in the first place. The current multifocals out there do have a gap in intermediate compared to near/distance. I certainly look forward to other IOL technologies like the FineVision lens. Crystalens is not always predictable and success seems predicated on mini-monovision at times. A truly accommodative lens will be a reality at some point, but until we fix the effective lens position problem ... it still remains elusive.”
Toric IOLs
Toric IOLs are a favorite premium lens for survey respondents, with 85 percent saying they implant them. Fifty-eight percent of the toric lens users rate their performance as excellent and a third describe it as good. Only 8 percent would rate it as fair.
“The toric lens is essentially a slam dunk for most patients,” says Dr. Shivaram. “However, the high-myope, floppy bag patients are still a challenge and I wish that the IOLs could be sized to take those diopter ranges into account.” Moultrie, Ga., ophthalmologist Terry Croyle also feels that patients respond to toric lenses. “These lenses really give the cataract patient the wow factor that can make the difference between a so-so subjective perception of the value of the surgery we perform and the uber-happy patient who can’t say enough good things about the surgery.”
One surgeon, who elected to be anonymous, says he uses the AcrySof toric currently, but is open to other options down the road. “I’m looking forward to implanting the Trulign,” he says. “However, I require a perfect corneal surface, perfect zonule integrity, perfect pupil function and very symmetrical central topography to offer a toric IOL. I also must have a patient with great patience to go through the wait to support his ocular surface properly.”
Some surgeons say toric lenses aren’t perfect, however. A surgeon from California says, “I’m using them less, now that I can do femtosecond laser arcuate incisions and get the other advantages in addition to the reduction of cylinder.” Another surgeon says he occasionally has “some difficulty with lens rotation in long eyes,” while a surgeon from North Carolina opines, “With toric lenses, there are many variables that can cause inconsistent results.”
Materials and Features
Surgeons on the survey also had opinions on the best IOL material, as well as what they like about the implants that they use for the majority of their cases.
When it comes to the monofocal lens surgeons use for most of their cases, 52 percent say they use the Alcon IQ Aspheric, 29 percent use the AMO Tecnis, 8 percent use B + L’s SofPort AO aspheric lens and 6 percent use the Lenstec Softec HD. The Rayner C-flex, Staar Nanoflex and B + L enVista were each chosen by 2 percent of the survey respondents.
“I use the Alcon IQ and the Softec HD Oval,” says Richard Phinney, MD, of Rock Island, N.Y. “With the IQ, I like the predictability of insertion, good centration. With the HDO, I like its depth of focus and the fact that it’s great for blended vision.” A Wisconsin surgeon says the IQ has several pluses as well as some drawbacks. “I like the fact that it is uniplanar, the AcrySof material keeps it adherent to the capsular bag and in position, the haptics are sized for bag fixation, the edge design minimizes posterior capsule opacification, it is aspheric and it has a yellow tint that I believe helps decrease the risk of ARMD,” he says. “The design also makes it easy to insert and manipulate directly into the bag. I don’t like the fact that 0.5-D steps are not offered at the lower and higher range of powers and that the range of powers is limited at both the high and low ends.”
Bruce Cohen, MD, of St. Louis, is in the Tecnis camp. “It’s a beautiful lens,” he says. “It’s got clear, aspheric optics without blue blockers or glistenings, is easily inserted through a 2.5-mm incision, and has no rapid capsule opacity.” Ellicott City, Md., surgeon Marjorie Warden also likes the Tecnis, saying, “It’s easy to implant, is one-piece acrylic and doesn’t have glistenings.” Dr. Shivaram likes the enVista lens. “It’s cryolathed and aspherically neutral,” he says. “It’s also the only lens to be shown as glistening-free. It has good centration and a low rate of PCO.”
Material-wise, 80 percent of the surgeons think acrylic is best, 8 percent prefer silicone, 5 percent like PMMA and 3 percent each go with collamer or hydrogel.
A surgeon in the acrylic group sums up his affinity for the material: “First, its slow folding and unfolding properties make IOL loading into the injection cartridge easier and IOL insertion into the eye safer—there’s no rapid release of energy as the IOL emerges from the injector,” he says. “Second, its material properties—tackiness—help keep the IOL centered and positioned in the bag (and on-axis, if using a toric IOL). Also, there’s no late IOL decentration with acrylic IOLs as is sometimes seen with three-piece silicone.” For his part, though, John Doane, MD, of Independence, Mo., likes silicone. “I like its ease of use,” he says. “Silicone also has essentially zero internal reflectivity, while acrylic has the highest internal reflectivity.”
Suturing and Explants
Surgeons say that, occasionally, an IOL will shift position and require some sort of intervention to re-align it. Sixty-three percent say that they have to go back in and suture one to three lenses per year, 7 percent need to suture re-fixate four to six lenses, 3 percent do it for seven to 10 lenses and another 3 percent have to suture more than 10 lenses each year. Twenty-four percent say they don’t suture any lenses during the year, either because of no complications or because they refer them to another surgeon.
Surgeons also reported the reasons they had to explant lenses and replace them with new ones in the past year. The reasons given on the survey included:
• glare and halo;
• incorrect lens power;
• waxy vision;
• pseudoexfoliation;
• uveitis/glaucoma/hyphema syndrome; and
• pigment on the lens.
“Improper power of the IOL is common,” says Dr. Taylor. “This is most commonly seen after cataract surgery in a previous refractive surgical patient.” One surgeon though, says he thinks a preop DIY approach lets you avoid explantations. “I’ve never had to explant a lens,” he says. “I choose the correct lens preop and don’t have my staff perform the exams.” REVIEW