Patient Selection
Since the ORange involves a perusage fee, surgeons say it may not pay to use it for every cataract patient.
“Here, we offer it on all premium lenses,” says Cleveland, Ohio, surgeon William Wiley. “We want to offer the best possible lens power to every patient who’s choosing presbyopic lens correction in order to decrease the chance of enhancement and minimize astigmatism. We also use it for all patients who are having astigmatism Corrected in order to make sure we’re treating the correct amount of cylinder with the correct procedure. We’ve also used it in some monovision patients.”
 Preop Prep
Preop Prep Factors such as the quality of the corneal surface and the nature of the anesthesia will impact ORange measurements. Here’s how to get the eye in the best shape.
“ORange patients are treated a little differently,” says Robert Weinstock, MD, of St. Petersburg, Florida. “Prior to me entering the room, the corneal surface has to stay healthy, and the epithelium has to stay lubricated. Before ORange, I used to use viscoelastic to keep the eye lubricated so the scrub technician didn’t have to constantly irrigate the eye. But now, with the ORange, I can’t do that. My staff has to use BSS for this. Also, you have to cut the drape such that the tears are able to drain out and don’t well up inside the speculum area.
“Also, make sure the lid speculum or the drape isn’t pressing down on the eye and distorting the globe,” adds Dr. Weinstock. “If you distort the globe, it will change the refraction that you get when you use the device.”
Next, surgeons say the ORange can’t be used effectively with nerve block anesthesia because the patient needs to maintain focus on the device’s fixation light. Topical anesthesia has to be used.
“Anesthesia is key,” says Dr. Wiley. “The way I do it is to mix lidocaine jelly with dilating and antibiotic drops in slurry that’s administered in the preop area. Then, by the time the patient’s back in the OR he’s not getting repeat lidocaine jelly. However, too much jelly can affect the readings, so it’s a fine line. I think having the jelly administered in the preop area also provides some lubrication to the cornea to prevent some drying or decrease of the tear film compared to other anesthetic drops such as tetracaine, which can cause a decrease in epithelial function and poor image quality during the use of the ORange.” Dr. Wiley says he also uses some IV sedation, but not too much. “Just like retrobulbar and peribulbar blocks can adversely affect fixation, if the patient is too deeply sedated it can affect fixation as well,” he says. “For good ORange image quality, you need patient participation.”
Venice, Fla., ophthalmologist Dee Stephenson uses lidocaine gel. “I make sure there aren’t any clumps of lidocaine gel on the eye and that I haven’t denuded or disrupted the epithelium,” she says. “If the corneal surface isn’t good, you won’t get good readings. The ORange v2.6 software actually won’t give you a reading if the corneal surface isn’t within certain parameters. In addition, if you have a patient with a lot of vitreous floaters or asteroid hyalosis, the system will notify you that it’s not a good reading.”
Intraoperative Variables
Though preoperative prep lays a good foundation for ORange readings, the factors that will make or break the measurements are often associated with the intraoperative period.
The proper use and management of the viscoelastic is important, say surgeons. “I’d advise surgeons to just use one type of viscoelastic, not a combination,” says Dr. Stephenson. “Don’t mix them, because they have different properties.” Dr. Stephenson says that Wavetec is working on improving calculations in the setting of mixed viscoelastics. Dr. Wiley also advises surgeons not to try to use an incision that’s too small. “I’ve found that if I use too small of an incision, I wind up stretching the incision during the case,” he explains. “And it’s been my experience that a stretched incision is more leaky than a larger incision.” He says a watertight incision is crucial later in the case when you make the ORange measurement, because the eye’s pressure will remain constant, rather than be decreasing because of a leak. Dr. Weinstock advises to monitor the cornea’s condition throughout the case, not just in the Prep phase. “During surgery, you can’t let the corneal surface dry out,” he says. “Also, you have to make sure no mucus washes up onto the anterior dome of the cornea. Many times while operating on an eye, there will be mucus that comes up from the conjunctiva and leaves stringy, fibrous-looking strands across the cornea. You have to manually remove these or flush them off the cornea before you take an ORange reading. Also, right before taking a reading, it’s helpful to put a squirt of BSS across the cornea to ensure an even, smooth tear film.”
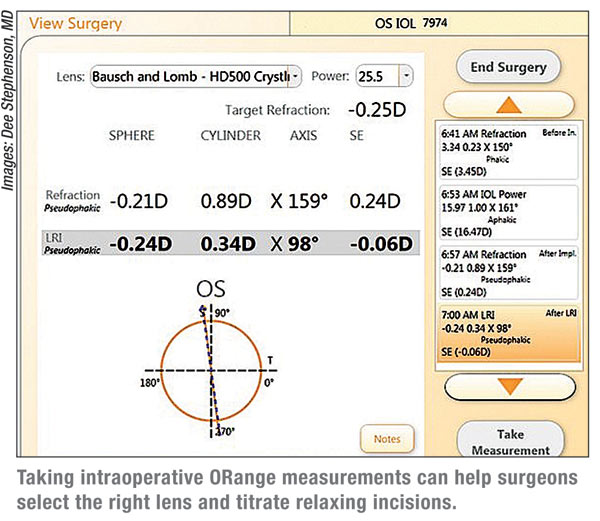
 The surgeons say they then proceed with the case as usual, and bring the
ORange in after the patient’s crystalline lens is removed. This
reading is important because it guides them toward which lens to
implant. “I usually walk into the OR with three lenses,” says Dr.
Wiley. “One lens is the one predicted as accurate by the IOLMaster
preop, one lens is above it in power and the third lens is below it. I
use the ORange to confirm the predicted lens or choose either of the
others. Finally, I’ll use the ORange reading to guide me for the axis
selection if I’m implanting a toric IOL.”
The surgeons say they then proceed with the case as usual, and bring the
ORange in after the patient’s crystalline lens is removed. This
reading is important because it guides them toward which lens to
implant. “I usually walk into the OR with three lenses,” says Dr.
Wiley. “One lens is the one predicted as accurate by the IOLMaster
preop, one lens is above it in power and the third lens is below it. I
use the ORange to confirm the predicted lens or choose either of the
others. Finally, I’ll use the ORange reading to guide me for the axis
selection if I’m implanting a toric IOL.”
“For the aphakic reading, you have to make sure you’ve removed all of the cortex and that there are no bubbles in the visual axis, because that can affect your reading,” explains Dr. Weinstock. “Make sure the viscoelastic has filled the anterior chamber and you don’t see different layers of viscoelastic in there because those will be different optical interfaces that can affect the ORange reading. You want it to be crystal clear through the cornea to the red reflex. It should be one mass of one consistency. Also, don’t squirt water in there because it can form little channels that you see in the anterior chamber.”
Surgeons say the intraocular pressure should be between 20 and 25 mmHg and remain constant. “One of the most common reasons for an unusual ORange reading is that the eye is actually collapsing and the pressure is decreasing as you’re taking the reading,” says Dr. Weinstock. “Over the 10 to 15 seconds it takes for the ORange to take and average its 40 readings, the wound is leaking, the chamber is shallowing and the corneal dome is changing shape. So, if I find that my measurement seems way off, the first thing I do is make sure the eye is sealed and firm. Often it’s soft when I touch it with a cannula, meaning it’s not sealed well enough. That’s when I either put a suture in or reseal the wound, then wait a second to make sure the eye is staying firm and maintaining pressure before taking a reading.”
The aphakic reading will also give you an accurate idea of how much astigmatism you actually have to deal with. “Technically, I’m using the aphakic reading to help confirm the use of the toric lens or an LRI,” says Dr. Wiley. “If I measure greater than 1.25 D of astigmatism, I’ll go ahead with a toric lens. If I’m measuring less than that, I’ll be using an LRI and the patient will receive a monofocal or, if they decided to have it, a presbyopia correcting IOL. I then use the aphakic refraction to fine-tune the spherical requirements for the lens.” Dr. Wiley says that, right before you take the reading, make sure the eye is properly exposed, and the chin, forehead and both eyes are on a parallel plane. “If the chin is rotated in an abnormal direction, tears can pool toward the nose and not drain adequately,” he says. “Too much of this can affect readings. You want the head slightly tilted temporally to allow for proper drainage during ORange readings.”
Dr. Weinstock says he gets good results with the aphakic readings because the viscoelastic really keeps the eye firm. “The viscoelastic tends not to force itself out of the eye so you know the eye is staying stable during the data capture,” he says. “The aphakic data tends to be more reliable as a result. That’s a tremendous advantage because, as we use the machine, we’re using the aphakic data more and more to make decisions. On all my refractive cataract cases, I compare my preop IOLMaster readings to intraoperative ORange readings and make IOL power decisions on the fly, sometimes up a little bit in power, sometimes down, and sometimes the same as the IOLMaster. But I’m finding that the ORange is giving me a tighter spread of refractive outcomes.”
Once the aphakic reading is done and the surgeon has implanted what he feels is the best-power lens, the pseudophakic reading is performed. This reading is especially helpful in getting the axis correct for a toric lens.
Surgeons say the main variable to try to control in this reading is the effective lens position. If anything temporarily affects the way the lens sits, the reading may not reflect the visual outcome after a week, a month or a year, since the position will have changed. To help get the most reliable lens position, surgeons offer several suggestions.
First, surgeons carefully remove all of the viscoelastic using irrigation/aspiration and re-inflate the eye with BSS. “I use I/A both in front and behind the lens to remove any viscoelastic that could induce lens tilt or an anterior lens shift,” says Dr. Wiley. “I want the eye as close to a physiologic state as possible. I inflate the eye with BSS to between 20 and 25 mmHg. Also, I try to use as little stromal hydration as possible to seal the wound, because if you over-hydrate the incision you can affect the cylinder power and axis. In fact, if I have to over-hydrate the wound, I may not pay that much attention to the cylinder power and axis of the pseudophakic reading, and I’ll have to go to my preop information for placement of an LRI or toric axis alignment. If the hydration is normal, however, I’ll use the pseudophakic reading for the toric axis alignment or, if I’m using a nontoric lens, it will guide my LRI placement. I can then adjust my nomogram for how large of an LRI to place and where it should go.”
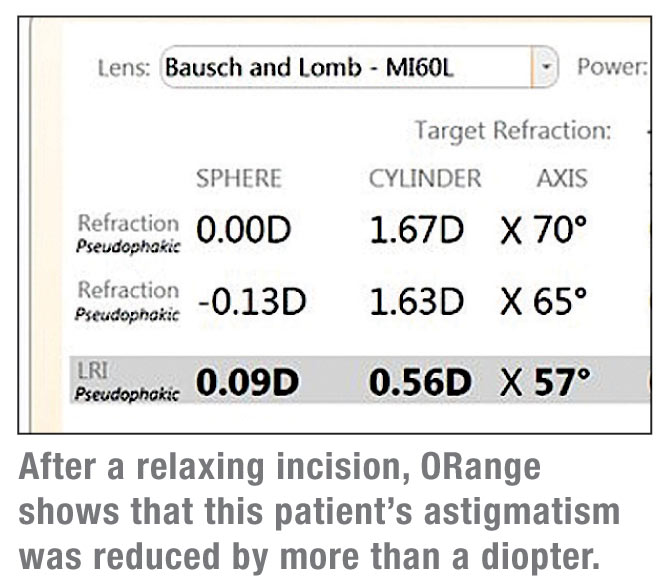
When performing LRIs, some surgeons will take several readings to titrate the incisions, while others will just take one. “When doing an LRI, I’ll capture information with the machine and see how much astigmatism there is vs. preop levels of cylinder and axis,” says Dr. Weinstock. “And if I feel the data is aligning with the preop data, I’ll go ahead and do the LRI. I’ll then recheck that the eye’s staying inflated and sealed and capture another reading to titrate the wound, if necessary. I’ll make an additional incision if it’s needed or even extend it and deepen it.” He says he uses the same principle for toric lens axis alignment. The ORange software will recommend which way to rotate the lens and by how much. He’ll make the rotation, reseal the eye and take another measurement. “You keep doing that until you feel you have the right lens position and ORange says you’ve neutralized the astigmatism,” says Dr. Weinstock.
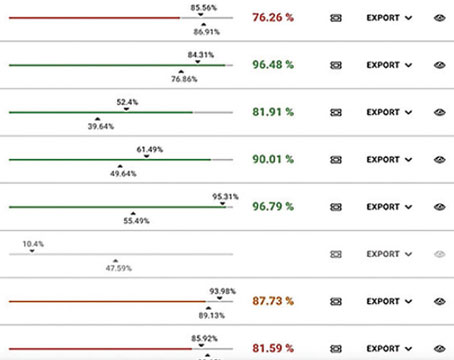
Dr. Stephenson says that, to get the most out of ORange, the surgeon has to track outcomes. “You have to be up for making your clinical results better,” she says. “If you don’t have something in place for outcomes analysis, using the ORange won’t be beneficial. Have a game plan based on your outcomes and follow through with it. If it doesn’t work, alter it and find out what works. It’s not an overnight success, but if you persevere, it will be a great addition to your armamentarium.”