A number of companies have been working on that premise, and while some of the products are not yet approved for sale in the United States (and others are still in development), the technology appears to be useful and promising. Here, surgeons familiar with several current options talk about their experience using them during surgery.
OCT in the Microscope
Carl Zeiss Meditec launched its Rescan 700 OCT system this spring. The Rescan 700, which is not approved for sale in the United States, is a real-time intraoperative SD-OCT that can be fully integrated into the OPMI Lumera 700 microscope; the surgeon doesn’t need to look up from the microscope to see the OCT data. Key functions of the OCT system can be controlled from the microscope’s foot pedal, so the surgeon can take videos, snapshots and 3-D OCT images without looking up or stopping the surgery. The Rescan allows the surgeon to see the surgical field in both a planar view and a cross-sectional view simultaneously, in real time.
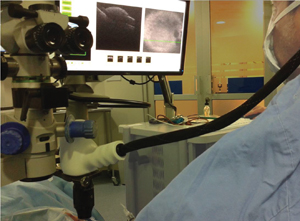
Justis P. Ehlers, MD, an assistant professor of ophthalmology at the Cole Eye Institute of the Cleveland Clinic in Ohio, is currently using Zeiss’s Rescan system under a research protocol. “The Rescan 700 can be used for any ophthalmic surgical procedure that requires the microscope, such as anterior segment surgeries like lamellar keratoplasty or vitreoretinal procedures such as epiretinal membrane peeling,” he says. “The OCT can be used for either live action monitoring or stop-action scans, and you can display the scans alongside the live microscope view with a heads-up display. The Lumera 700 has the Callisto video display system on the side; that can also display both images, so that anybody in the OR can see the surgical video and the OCT signal.
|
Dr. Ehlers says the biggest difference between this type of system design and previous intraoperative OCT systems is that a microscope-integrated system allows for real-time OCT without pausing the surgery to look away from the microscope. “There have been a few microscope-integrated systems developed, including one of the first systems designed at Duke University by Drs. Cynthia Toth and Joseph Izatt,” he notes. “Other systems include our prototype at the Cleveland Clinic. To my knowledge the only two systems that currently have a heads-up display system are the Cleveland Clinic prototype and Zeiss’ Rescan 700.”
A Touchscreen Display
Haag-Streit’s intraoperative iOCT system, developed by OptoMedical Technologies in Lübeck, Germany (also not approved for sale in the United States), attaches to the camera port of the microscope; data is displayed on a screen mounted on the microscope. The screen is also used to operate the system (to switch from anterior to posterior views, for example). The device follows the zoom and focus of the microscope so the scanned area matches the area being viewed, and scans and images can be saved for future review. Surgeons report that the device can reveal structure to a depth of about 4.2 mm in air and 3.1 mm in water, with a resolution of about 10 µm.
Prof. Claus Cursiefen, FEBO, managing medical director of the Center of Ophthalmology at the University of Cologne in Germany, has been using this system for several months. “Online intraoperative OCT is easy and convenient to use since it does not disturb normal operative flow,” says Professor Cursiefen. “One can see surgical details via the microscope and OCT details by looking onto the screen next to the oculars. It’s a new and fascinating experience since it adds a new dimension of visibility, showing things one cannot see through the operating microscope.”
Professor Cursiefen says this technology helps in difficult surgeries and in certain steps of standard surgeries. “For example, when performing DMEK on a very opaque cornea, it helps the surgeon determine whether the orientation of Descemet’s membrane is correct,” he says. “It helps with Boston keratoprosthesis surgery in terms of orientation, correct assembly and positioning of the device. In DALK it helps with monitoring the depth of the preparation, the interface fluid, the status of Descemet’s membrane and so forth. The only downside I see is the cost.”
|
Available in the United States
One intraoperative OCT system is currently available in the United States: Bioptigen’s Envisu C2300 Spectral Domain Ophthalmic Imaging System, designed for handheld or microscope-mounted use. (See picture, p. 18.) (In April, Bioptigen unveiled the Envisu IntraSurgical OCT, designed for real-time imaging during ophthalmic surgical procedures, compatible with most operating microscopes. The new system, which features independent focus and zoom control, is not approved.)
Cynthia Toth, MD, professor of ophthalmology at Duke University Medical Center and professor of biomedical engineering at Duke University’s Pratt School of Engineering in Durham, N.C., was one of the early pioneers of using OCT during surgery. “Surgeons are used to using OCT before and after their surgical cases to evaluate their work—particularly in macular surgery,” Dr. Toth says. “Using OCT in the operating room seems like a natural progression, both to identify endpoints and to see whether we’ve reached our surgical goals.”
Dr. Toth initially used the handheld OCT system from Bioptigen. “The Bioptigen device is approved for commercial use in supine imaging of adults and infants in the OR, but it’s not built into the microscope,” she notes. “The handheld portable OCT can go to the OR and be held over the patient’s eye, and there’s an attachment that hooks it on to the microscope. Of course, you still have to pause in order to look at it. But I’ve found that the more you see, the more you want to stop surgery and check things. I’ve peeled this internal limiting membrane, but is the hole still open? Should I use a gas bubble? How much of a gas bubble do I need?”
Clinical Impact
“There are a lot of questions out there regarding where intraoperative OCT is useful and how it can make a difference,” notes Dr. Ehlers. “Many of the surgeons at Cleveland Clinic use this technology in almost every macular case. Most of our corneal surgeons at Cleveland Clinic do almost all of their lamellar keratoplasties with intraoperative OCT guidance. They believe it’s a valuable tool in those procedures.
“To better assess the impact this technology is having on surgical decision-making, we’ve been prospectively assessing intraoperative OCT over the past three years,” he continues. “We’ve enrolled more than 800 patients in prospective studies. We’ve found that in a large number of cases intraoperative OCT appears to inform surgical decision-making. In fact, in 10 percent or more of cases, the OCT data actually causes surgeons to change their mind. For example, if the surgeons think they’ve peeled all of the membrane, they may look at the OCT and realize there’s residual membrane that requires peeling. Or the opposite: They think there’s more they need to peel, but when they look at the OCT the membranes are entirely removed and they’re able to finish the procedure.
“We’re still investigating how much difference this technology makes in terms of surgical efficiency and outcomes,” he says. “If it’s simply used to find out whether you accomplished what you set out to accomplish, it can be done very quickly, whether you’re using a microscope-integrated system or a portable system mounted to the microscope.”
In terms of potential downsides, one issue is whether the added information might become a distraction. “We don’t yet know for sure what to make of all the information this technology provides,” admits Dr. Ehlers. “One concern is information overload. When does this become too much information? I believe the answer will sort itself out as we learn the best ways to display the information. With that in mind we’ve been experimenting in our lab on different formats to show the data to the surgeon through a heads-up display feedback system. You want to be sure you’re providing information that’s helpful and not distracting. (The Zeiss system also provides some flexibility in its heads-up display options.)
|
Down the Line
“Using OCT to guide you in real time as you’re reaching and performing maneuvers is the way I think OCT will be used in the long run,” says Dr. Toth. “Right now, the speed of SD-OCT is probably not ideal for truly guiding the surgeon while performing maneuvers, but different technologies that will increase the speed are being developed. Swept-source OCT is coming down the pike; image-guided surgery is further down the line. But even at current speeds having SD-OCT in the microscope does make it much easier to capture images so you can stop and view the structure of the tissues.”
Dr. Toth is currently helping to develop a swept-source OCT system with a heads-up display at Duke University. “With our generation-one system, you had to look up at a screen; our generation-two system is inside the microscope,” she explains. “We’re trying different display options, including Google Glass. The current version of Google Glass probably wouldn’t be my favorite viewing option choice, but we’ve just begun exploring the alternatives.”
Professor Cursiefen says he’s looking forward to future advances in this technology, such as precise intraoperative measurement of tissue thickness for surgeries such as DALK, and high-resolution imaging of the angle during glaucoma surgery. “In fact, that’s one of the most exciting things about this technology: where it may lead in the future,” says Dr. Ehlers. “It could potentially open the door to procedures we haven’t been able to do without this type of information, such as intratissue-targeted delivery of pharmacotherapy.” REVIEW
Dr. Ehlers’ research includes equipment provided by Zeiss, and he owns intellectual property licensed to Bioptigen and Synergetics related to intraoperative OCT technology. One of Dr. Toth’s co-investigators has a financial interest in Bioptigen. Professor Cursiefen has no financial ties to any product mentioned.