(For an in-depth look at the latest point-of-care test, Sjö, see “Dry Eye: More Than a Symptomatic Disease” on p. 50.)
Inflammadry
The Inflammadry test from Rapid Pathogen Screening tests the tears for the enzyme known as matrix metalloproteinase-9. The company says MMP-9 on the ocular surface is a sign of inflammation, and that its presence means that a dry-eye patient may respond to anti-inflammatory therapy.
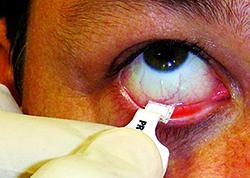
The Inflammadry test has been likened to a pregnancy test in that it doesn’t provide a quantitative result, just basically a yes or a no. To administer the test, the tech or physician collects a tear sample, then activates it with a buffer solution. In 10 minutes, the test will be ready, and will either show a solitary blue line, indicating a negative result, or a blue line accompanied by a red line, which is positive. The test uses 40 µg/ml of MMP-9 as a cutoff point; anything above that will yield the red line, anything below will register as negative. In a study partially sponsored by RPS, researchers analyzed 46 dysfunctional tear syndrome patients and 18 controls. They found significantly higher mean MMP-9 activity in the test groups (as high as 381.24 µg/ml for one group) than in the controls, which registered a mean of 8.39 µg/ml. The researchers say that the MMP-9 levels showed significant correlation with symptom severity scores, decreased low-contrast visual acuity, fluorescein tear breakup time, corneal and conjunctival fluorescein staining, topographic surface regularity and the percentage area of abnormal superficial corneal epithelia.1
|
Physicians say, though, that the test shows there’s ocular inflammation but you have to rely on other diagnostic information to drill down to the cause, if desired. “With the MMP-9 test, if it’s positive, I know there’s inflammation,” says Mina Massaro-Giordano, MD, co-director of the Penn Dry Eye and Ocular Surface Center at the University of Pennsylvania’s Scheie Eye Institute. “So the next question is: What’s causing it? Is it dry eye? If it is, what type of dry eye is it? Is there another reason for the abnormal ocular surface? It might not even be dry eye at all. For example, conjunctival chalasis can cause higher MMP-9 levels as that loose skin rubs up and down with blinking. But if you remove it, hopefully the inflammation will get better.”
Dr. Hannush says knowing there’s inflammation present is often helpful enough. “There’s only so much testing and examination you can do at each patient visit,” he says. “Often, the ophthalmologist has to decide what single additional diagnostic test would help direct the patient’s treatment. For most of us who do this type of work, it’s trial-and-error. If you perform one test and it’s revealing, you may not wish to further pursue the etiology of the dry eye, but instead recommend a treatment. So, if I do Inflammadry and find inflammation, I’m going to treat it and not keep looking for another problem. But there’s no doubt that there may be more than one cause for the dry eye. One of the benefits of a negative Inflammadry test is that it directs you away from inflammation as a cause of the dryness. This is helpful because then there’s no reason to spend the time and money on anti-inflammatories such as corticosteroids or cyclosporine A. Instead, you can concentrate on tear supplementation and/or occlusion of the puncta.”
Dr. Hannush says another group of patients who might benefit from dry-eye diagnostic testing is individuals coming in for a surgical procedure. “This would include laser vision correction and cataract extraction with premium intraocular lens implants, specifically multifocal lenses,” he says. “If you don’t diagnose a corneal surface problem accurately it can lead to suboptimal results in these patients. For their part, toric and accommodative IOLs may not have their performance compromised as significantly by the ocular surface as multifocal implants. Of course patients who are spending $1,000 or $2,000 out-of-pocket on any premium lens implant have very high expectations. Also, if a patient has a dense cataract, you may not be able to tell what his or her visual potential is until after removal of the cataract, so it would be helpful to eliminate the ocular surface problems ahead of time.”
Lactoferrin Testing
The Advanced Tear Diagnostics’ Tearscan system is designed to detect the levels of the protein lactoferrin, which is produced in the acinar cells of the lacrimal glands. The idea behind tracking this protein is that it reflects aqueous tear production. The company also makes a test kit for immunoglobulin E levels in order to detect allergic conjunctivitis.
Ken Greenberg, MD, a practicing ophthalmologist and ATD’s chief medical officer, says the test takes three to five minutes. “The lactoferrin test process involves taking a sample of tears and then putting the sample in a diluent,” he explains. “The mixture is then placed on a test strip. In terms of which patients undergo the test, if someone has symptoms such as foreign body sensation, burning, intermittent blurry vision or a scratchy sensation, we’d start to consider using the test. We sometimes use the Ocular Surface Disease Index, a validated questionnaire, to help decide who should undergo the test, as well. We also test patients who are contact lens intolerant.
“Lactoferrin is an interesting protein,” Dr. Greenberg continues. “It has anti-microbial and anti-inflammatory properties. So, by having an idea of the lactoferrin level in the tear film, we can assess what the tear production in the lacrimal glands is. This allows us to determine the underlying cause of the dry eye—whether it’s aqueous deficiency or evaporation—since the lactoferrin levels are reduced in patients with aqueous-deficient dry eye. The test has a sensitivity of 83 percent and a specificity of 98 percent.” A study of human tears found the average lactoferrin level to be 1.5 mg/ml (range: 0.9 to 2 mg/ml),2 so ophthalmologists who use the Tearscan test classify any result below 0.9 mg/ml as aqueous-deficient.
In an effort to determine lactoferrin’s correlation to patients with dry eye, researchers in Japan prospectively divided 103 dry-eye patients into three groups: Sjögren’s syndrome (n: 23); dry eye not associated with Sjögren’s (n: 71); and Stevens-Johnson syndrome (n: 9). Sixteen normal patients also had their tears tested. All patients had their concentrations of lactoferrin, epidermal growth factor and aquaporin 5 measured by enzyme-linked immunosorbent assay. The investigators found that the concentration of lactoferrin was significantly decreased in tears of non-Sjögren’s (p=0.0001), Sjögren’s (p=0.00005) and Stevens-Johnson syndrome compared to control patients. The study’s researchers say that the tear components in dry-eye patients apparently differ from those in normal patients both quantifiably and qualitatively.3
Dr. Greenberg says periodic checking of lactoferrin levels while a patient is undergoing therapy can be helpful, and is similar to other tests with which patients are already familiar. “We’ll initiate treatment, then bring them back in a month to three months,” he explains. “We do start to see the lactoferrin levels rise, though this hasn’t been officially studied and is just my clinical impression. I think it can be helpful for patients to have a quantitative test, because they’re used to undergoing lab tests and then hearing whether their cholesterol or anemia is better or worse since their last visit.”
There may be potential synergies in testing both lactoferrin and IgE at the same visit in patients whose symptoms seem to combine both the hallmarks of dry eye and allergy. “The signs and symptoms of dry eye and allergy sometimes overlap,” says Dr. Greenberg. “So, you may very well administer it at the same time. The classic case is the contact lens patient where the signs and symptoms of the two conditions can overlap quite a bit. The IgE test just adds another piece of information for the clinician.”
LipiView
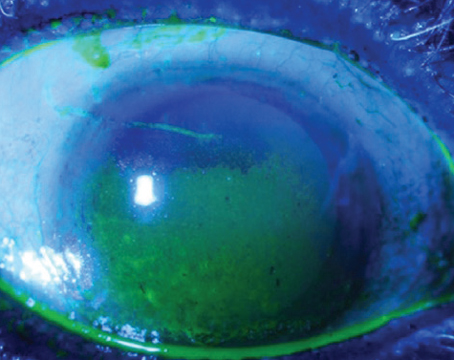
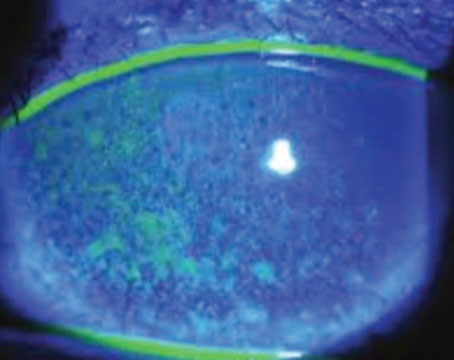
The TearScience LipiView system is the diagnostic arm of a pair of products, the other of which is the LipiFlow treatment device. LipiView combines digital interferometry imaging of the lipid layer of a patient’s eye with a quantitative measurement in an effort to suss out evaporative dry eye. If the lipid layer shows a certain amount of thinning, TearScience says, this indicates a problem.
| ||||
Duke cornea specialist Alan Carlson says that, by the end of 2014, ophthalmologists will have access to the LipiView II, a new device with additional ways to analyze a patient’s lids. “It actually gives you three different analyses of photos of the meibomian glands in the lower lid,” Dr. Carlson says. “The first one is an infrared photo. The next is a transillumination image. The third is a merged image of the first two methods. So, you’ll actually see if the glands are normal, dilated, if there are areas of dropout and even if there is some infection present.”
Dr. Carlson says LipiView can help him avoid undertreatment, and is useful for documentation. “Not everyone in my practice gets a LipiView exam,” he says. “Meibomian gland dysfunction is more frequently on my radar, though. Even Ed Holland and Donald Korb wrote an article on ‘non-obvious MGD,’ and if they can miss it, others certainly can as well. We still undertreat, but I’m becoming more sensitive in picking it up. It’s common for me to get several LipiView analyses on patients, but even that doesn’t always guide my decision making. Also, if patients are symptomatic and I see gland obstruction, I’m going to treat them, but I’ll also get documentation with LipiView. Now, with LipiView II, documenting the status of the lid morphology is going to be an added benefit.” Dr. Carlson adds that, as a refractive surgeon, he’s acutely aware of the issues posed by an inadequate ocular surface postop. “If you have a busy surgical practice, by definition you’re seeing dry-eye patients and have the potential to make them worse,” he says. “If he’s a non-symptomatic dry-eye patient to begin with and even has small-incision cataract surgery, he will be getting drops afterward that can irritate the eye. This can tip the patient over to symptomatic dry-eye while he’s recovering from surgery. So, I have a pretty low threshold for performing LipiView and LipiFlow on the patient preop.”
TearLab Osmolarity Testing
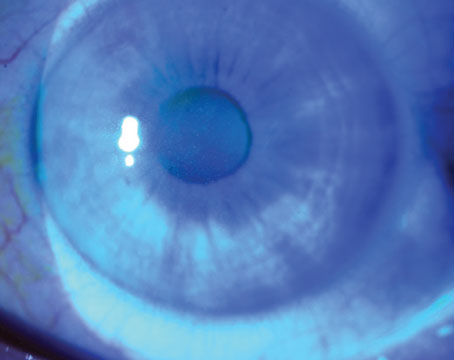
The TearLab test measures how concentrated the electrolytes in the tears are, with higher levels signifying that the aqueous component of the tears is low. To administer the test, the physician or technician takes a 50-µl sample of a patient’s tears from each eye using a special pen and sample card. The TearLab device analyzes the card and provides a readout of the osmolarity level in the sample. Experts say a reading of 307 mOsms/L or below is normal. Anything above that in one of the eyes is a sign of dry eye, the severity of which increases with increasing osmolarity. A difference between the eyes, where one is high and the other normal, is a red flag as well. The test takes about two minutes.
Experts say that, like the other dry-eye tests that have come online in recent years, osmolarity testing should be just a part of a clinician’s overall exam. Rhode Island ophthalmologist Michael Lemp, who helped develop the osmolarity test, says a questionnaire can be useful for identifying potential test candidates ahead of time. “To make sure you’re not overtreating but, at the same time, not missing anyone, as well as to not slow down the patient flow in your practice, we’ve recommended practices develop a questionnaire for patients,” Dr. Lemp says. “We recommend that it be one page, and that it contain a series of questions that will lead you to identify people who have a greater chance of having an abnormal osmolarity result. The questions can begin with, ‘Have you ever been diagnosed with dry eye?’ followed by a series of symptoms the patient can identify with, including symptoms that we now know are more common in relation to dry eye than we thought before, such as blurred vision during reading.”
|
Dr. Lemp says, logistically, physicians have learned it’s probably best to place the testing unit in a small room or area of its own, rather than in an exam lane. “We’ve found one of the worst things to do is put one of these in an exam lane,” he says. “If you decide a patient needs this test, the room the test is in will almost always be occupied, and the patient will have to wait for the room to be open.”
J. Daniel Nelson, MD, a professor at the University of Minnesota Regions Hospital, says acclimating a patient to the room can help get a valid result. “If a patient puts a drop in the eye soon before initiating the test, or you stimulate reflex tearing with bright room lights or by shining a slit lamp in his eye, it will probably influence the result of the test,” he says. “We acclimate patients to the room by having the tech ask them some questions first, to ensure that they’ve already been in the room for a few minutes before the test is started, and therefore they’re not going to undergo any change in environment that’s going to induce reflex tearing. If there’s reflex tearing, or you instill a drop, it will result in an artificially low osmolarity. However, if a patient has had a drop instilled in the eye beforehand or had reflex tearing and the result comes up high—that’s still a significant finding.”
In a poster by TearLab investigators presented at the 2009 meeting of the American Academy of Ophthalmology, researchers found that, out of 300 patients, osmolarity correctly identified 88 percent of normal subjects, 75 percent of mild to moderate disease patients, and 95 percent of severe disease patients. “While tear osmolarity is good for testing whether a patient has dry-eye disease or not, and periodically checking on the efficacy of treatments, it doesn’t differentiate between aqueous-deficient and evaporative dry eye,” notes Dr. Lemp. “So, you still have to perform an exam and determine whether there is lid disease present, also.”
Dr. Nelson says he frequently uses the test to identify patients with a normal result. “My particular practice is a little unusual in that I’m usually seeing people who have already been to two or three ophthalmologists for their irritated eyes and yet continue to have problems,” Dr. Nelson says. “So, one of the ways the test is useful to me is if it’s normal. A normal result becomes sort of an objective statement of, ‘You have eye pain but it’s not due to dry eye.’ This helps because previous physicians have often blamed the patients’ complaints on dry eye, but this tells me that probably isn’t the case.” REVIEW
Dr. Carlson is a consultant for TearScience and Dr. Hannush has a financial interest in Rapid Pathogen Screening. Dr. Lemp is the chief medical officer for TearLab. Dr. Massaro-Giordano has no financial interest in any of the products mentioned.
1. Chotikavanich S, de Paiva C, Quan Li D, et al. Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome. Invest Ophthalmol Vis Sci 2009;50:7:3203.
2. Zhou L1, Zhao SZ, Koh SK. In-depth analysis of the human tear proteome. J Proteomics 2012;75:13:3877-85.
3. Ohashi Y, Ishida R, Kojima T, et al. Abnormal protein profiles in tears with dry eye syndrome. Am J Ophthalmol 2003;136:2:291-299.