Approximately 5 to 10 percent of all skin cancers occur in the eyelid. Incidence studies indicate that basal cell carcinoma is the most frequent malignant eyelid tumor, followed by squamous cell carcinoma, sebaceous gland carcinoma, and malignant melanoma.1 Many therapeutic methods have been suggested to combat the morbidity and mortality associated with these lesions.
In this article, I will describe such clinical characteristics and clues to diagnosis of malignant eyelid lesions. I will also describe the most common and most effective methods of treatment once these lesions have been identified.
Clinical Characteristics, Clues to Diagnosis
• Basal cell carcinoma. Basal cell carcinomas originate as a neoplastic transformation of the basal cells of the epidermis. If the center of the tumor becomes necrotic as a result of insufficient blood supply, it may slough and bleed, and become more obvious to the patient. Some BCCs, however, may not have an ulcerated center or an elevated margin.
Basal cell carcinomas occur most frequently on the lower eyelid, followed in order of frequency by the medial canthus, upper eyelid and lateral canthus.1 The localized nodular and noduloulcerative subtype is the "classic" lesion and accounts for approximately 75 percent of all BCCs.2 A nodular BCC typically begins as a small translucent nodule or papule with pearly outer margins, often evolving into the characteristic lesion composed of a central ulcerated crater with pearly rolled margins. The less-common diffuse morpheaform or sclerosing type typically appears as a white-pink to yellow plaque with indistinct clinical margins and no obvious ulceration. Hyperpigmentation of either type of lesion may lead to confusion with malignant melanoma. A BCC of the right upper eyelid is shown in Figure 1.
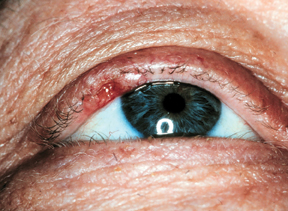 |
| Figure 1: Basal cell carcinoma of the right upper eyelid. Note the slightly pigmented area in the lateral right upper eyelid with central ulceration, rolled edges, and loss of eyelashes (madarosis) in the area of the lesion. |
• Squamous cell carcinoma. Squamous cell carcinoma of the eyelids and periocular region is a potentially lethal tumor. Its hallmark feature is extension into the underlying dermis. Actinic keratosis, Bowen's disease, and radiation dermatoses are all precursors to the development of squamous cell carcinoma.
Squamous cell carcinomas, like BCCs, occur most frequently on the lower eyelid. SCCs often appear as painless nodular or plaque-like lesions with irregular rolled edges, chronic scaling with roughened patches, fissuring of the skin, pearly borders, telangiectasia and central ulceration.3 An SCC of the right upper eyelid is shown in Figure 2. SCCs often mimic other lesions, and a biopsy is critical to establish the diagnosis. Often, examination of the face or extremities for other types of premalignant lesions will aid in the diagnosis. Unlike BCC, squamous cell carcinoma has a tendency to metastasize.
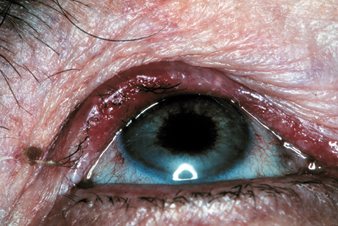 |
| Figure 2: Squamous cell carcinoma of the right upper eyelid. Note the violaceous red hue across the entire upper eyelid with areas of madarosis and trichiasis. |
• Sebaceous gland carcinoma. Sebaceous gland carcinomas preferentially develop in the eyelids because of the abundance of sebaceous glands in the tarsus (meibomian glands), eyelashes (Zeis glands), and the caruncle.
Sebaceous gland carcinomas may have varied clinical presentations, according to their site of origin. SGCs are more common in women than in men, account for less than 1 percent of all eyelid tumors, and the average age of a patient with SGC is 68 years. SGCs developing in the Zeis glands on the eyelid margin may appear as a small nodule and be mistaken clinically as a chalazion, an intradermal nevus or a BCC. The most common form of sebaceous gland carcinoma is the nodular type and can easily be mistaken for a BCC, SCC, chronic chalazion, or even as blepharitis. A second type of SGC is a nonnodular tumor that is more infiltrative and may present as unilateral blepharoconjunctivitis. Loss of eyelashes (madarosis) may help to differentiate it from benign lesions such as chalazia.
• Malignant melanoma. Primary malignant melanomas of the skin near the eye are rare, comprising 1 percent or less of all malignant eyelid tumors. Nodular melanomas typically have a blue-black color and a spherical configuration. They can be distinguished from superficial spreading melanoma by their more uniform color. Superficial spreading melanoma of the eyelid may display a wide variety of colors, including tan, black, gray, dull pink or rose.
The tumors typically are elevated above the skin and have a distinct (or discrete) border. Malignant melanomas, however, often assume irregular growth patterns and have a high incidence of metastasis.
Recommendations for Therapy
• Basal cell carcinoma and squamous cell carcinoma. As mentioned, ulceration, bleeding, or change in size, color, or appearance are worrisome for malignancy. If I am unsure of the potential for malignancy and I suspect either basal cell or squamous cell carcinoma, I often biopsy a small piece of the lesion for pathologic analysis.
After biopsy, if the lesion is interpreted as either a basal cell or squamous cell carcinoma, I will either remove the lesion entirely in the operating room using frozen-section control or send the patient to a Mohs' surgeon for removal with subsequent repair. In private practice, it is often more practical to have the lesion removed by a Mohs' surgeon with repair the same or the following day. In some cases where the lesion appears very small and well-localized, I will sometimes remove the entire lesion with a wedge resection (2-mm borders on each side with sutures marking left, right, and inferior borders). If one of the margins remains positive, I will either remove additional tissue or refer the patient to a Mohs' surgeon.
• Sebaceous gland carcinoma. Sebaceous gland carcinomas of the eyelid have long been considered the most lethal ocular adnexal tumors. I recommend Mohs' micrographic surgery or excision with frozen-section control combined with conjunctival map biopsies when sebaceous gland carcinoma is diagnosed on the eyelid. Although Mohs' micrographic surgery may examine all tissue planes to determine whether a tumor has extended beyond the excision plane, the potential for pagetoid conjunctival spread to noncontiguous areas exists. Excision with frozen-section control in the hands of a well-trained and experienced ophthalmic surgeon and pathologist, therefore, spare the most tissue and presents the least likely chance of recurrence. Exenteration may be necessary when the tumor has invaded orbital tissues. Sebaceous gland carcinoma possesses true metastatic potential, and patients should undergo medical and oncologic surveys after diagnosis of the eyelid lesion.
• Malignant Melanoma. Despite its low frequency (approximately 3 percent of all skin cancer), malignant melanoma has a relatively poor prognosis. There is considerable debate regarding the best treatment for malignant melanoma.
The World Health Organization Melanoma Program conducted a study in the 1980s that recommended the use of 1-cm to 3-cm surgical margins for malignant melanomas based upon Breslow thickness. The routine use of 1- to 3-cm margins on the eyelid and periocular skin obviously would yield large surgical defects. In practice, therefore, the customary and most tissue-conserving approach is to use either Mohs' micrographic surgery or narrow (4 to 5 mm) margins examined by a well-trained and experienced pathologist.
Overall, malignant eyelid tumors can present in either typical or atypical manners. I have found that sometimes there are subtle clues that the physician can use to help in diagnosis, but most often a biopsy is required to confirm or disprove the suspicion of malignancy. To excise most malignant eyelid tumors, I use either Mohs' micrographic surgery or surgical excision with frozen-section control. For sebaceous gland carcinoma, the surgeon must also use conjunctival map biopsies because of skip lesions.
Dr. Cook is in private practice at Charlotte Ophthalmology. Contact him at (704) 364-7400 or briggscook@ yahoo.com.
1. Cook BE Jr., Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology 1999;106:746 –50.
2. Riedel KG, Beyer-Machule CK. Basal cell carcinoma. In: Albert DM, Jakobiec FA, eds. Principles and Practices of Ophthalmology, 2nd ed. Philadelphia: Saunders, 2000; 3361–5.
3. Scott KR, Kronish JW. Premalignant lesions and squamous cell carcinoma. In: Albert DM, Jakobiec FA, eds. Principles and Practices of Ophthalmology, 2nd ed. Philadelphia: Saunders, 2000;3369–74.



