Small-incision lenticule extraction has many options for retreatment. Here, surgeons who are perfecting these retreatment methods share updates on their findings.1,2,3
The Current Options
One retreatment option after SMILE is photorefractive keratectomy. However, PRK after SMILE is associated with a slow visual recovery, patient discomfort and increased risk of corneal haze. Another is to convert the SMILE cap into a LASIK flap. The simplest way to do this is by performing a side cut only. The main drawback of performing just a side cut is that the optical zone is limited because the diameter of the new flap must fall within the diameter of the original SMILE cap.
CIRCLE is a proprietary retreatment software package developed for the VisuMax Femtosecond laser (Carl Zeiss Meditec; Jena, Germany).
CIRCLE has settings for converting the primary SMILE cap into a larger-diameter flap for excimer laser ablation. The CIRCLE software, not commercially available in the United States, lets surgeons choose from different settings to create lamellar rings and junction cuts that connect with the primary cap interface. CIRCLE can be a suitable option for caps 120 µm or thinner, according to Dan Z. Reinstein, MD, MA(Cantab), FRCSC, FRCOphth of London Vision Clinic, London, United Kingdom, who uses a cap thickness of 135 to 145 µm. This leaves enough residual stroma in the cap to perform a thin-flap LASIK retreatment in almost all cases.
Dr. Reinstein and colleagues published a retrospective study of consecutive LASIK-after-SMILE retreatments that underwent a primary SMILE procedure at their practice between September 2013 and January 2016 (116/2643).1,2 Mean postop spherical equivalent relative to the target was +0.19 D ±0.49 D (range: −0.88 to +2.13 D), with 74 percent within ±0.5 D. Postop uncorrected acuity was 20/20 or better in 81 percent of eyes. However, it was found that there was overcorrection in myopic retreatments of 1 D or higher, with a mean postop spherical equivalent of +0.99 ±0.64 D (range: -0.63 D to +2.13 D) in this group of 20 eyes. They concluded that myopic LASIK retreatment after primary myopic SMILE requires a different nomogram than that for myopic LASIK retreatment after primary myopic LASIK.
 |
| Surgeons disagree on the best way to enhance SMILE. |
Planning the Flap
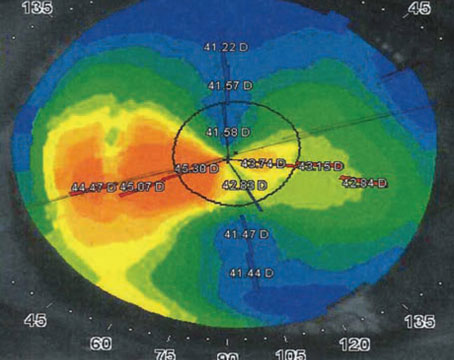
To determine the safety of LASIK after SMILE, Dr. Reinstein relies on very high-frequency digital ultrasound or optical coherence tomography to measure maximum epithelial thickness and minimum cap thickness. The investigators had previously determined that the Artemis Insight 100 (ArcScan; Golden, Colorado) measured cap thickness with a reproducibility of 4.4 µm.4
To prevent a buttonhole, Dr. Reinstein says that the flap thickness should be four standard deviations (18 µm) greater than the maximum measured epithelial thickness. To avoid tissue-sliver formation from the new flap crossing the SMILE interface, flap thickness should be four standard deviations (18 µm) thinner than the minimum cap thickness. Therefore, it’s safe to create a LASIK flap after SMILE if the difference between the maximum epithelial thickness and minimum cap thickness is at least 40 µm:
(maximum measured epithelial thickness + 18)<intended flap thickness<(minimum measured cap thickness -18)
The investigators found the residual stromal thickness (RST) threshold by subtracting the flap thickness and the ablation depth at the thinnest point of corneal pachymetry per VHF digital ultrasound or OCT for myopic retreatments. For hyperopic retreatments, it was determined by subtracting flap thickness and central ablation depth. A bias of four standard deviations (18 µm) was added to the planned flap thickness, and a minimum predicted residual stromal bed depth of 250 µm was required to proceed with flap creation.
The 100/116 eyes meeting these criteria were re-treated with LASIK. The nomogram used at the London Vision Clinic for LASIK after SMILE was the same as used for enhancements after LASIK, but the tendency towards overcorrection for LASIK after SMILE suggests that this procedure needs a unique nomogram.
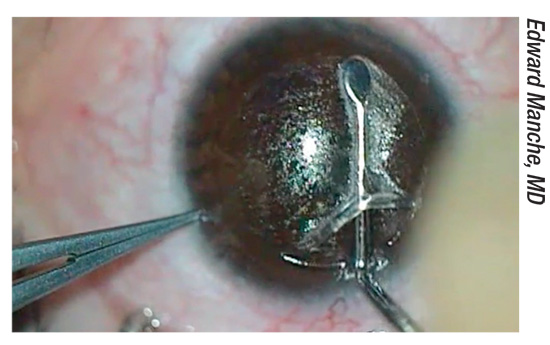
A second study analyzed SMILE retreatment cases spanning September 2013 to January 2017 (162/3,933) and describes a novel flap-lift technique developed to minimize the risk of tearing and/or accessing the small incision from the primary SMILE procedure.1 After initially using a standard bimanual flap lift used in primary LASIK, the investigators sought to lower the risk of penetrating the small incision left over from SMILE with an instrument tip.
After several iterations, Dr. Reinstein and colleagues landed on a bimanual fulcrum flap-lift technique. The first step is opening the flap side cut in the inferior third of the flap, away from the small incision. The instrument is inserted with gentle upward tenting to avoid the tip inadvertently accessing the original SMILE interface. After pushing the flap lifter across the flap, it’s used to open the side cut on the opposite side of the flap edge. This will be the entry point for the McPherson forceps. The forceps are inserted halfway through the flap and swept upward, so the region of the small incision is separated by the broadside of the instrument. The surgeon holds the flap lifter in place, relying on the lower, unseparated section of the flap for countertraction against the forceps. Finally, the forceps are held against the superior hinge to counter the force of the flap lifter, which separates the inferior portion of the flap.
The final 84 of 139 consecutive SMILE retreatments in this study used this flap-lifting technique: No intraoperative complications were reported, suggesting that careful flap planning based on direct measurement and the new bimanual inferior pseudo-hinge fulcrum flap-lifting technique can mitigate the risks of a LASIK retreatment after SMILE.
“By combining anatomical imaging of the epithelium and SMILE interface for flap thickness planning, and the inferior pseudo-hinge fulcrum flap-lifting technique, LASIK has become our preferred retreatment option after SMILE,” says Dr. Reinstein.
Secondary SMILE?
Another technique under investigation is performing a second SMILE under the primary procedure. Ahmed Sedky, MD, FRCOphth, chair of the Eye Subspecialty Center, Cairo, Egypt, and colleagues cited the first report of this technique by David Donate, MD, of Lyon, France, and colleagues,5 and reported on their own small case series of nine eyes in seven patients who required myopic SMILE retreatment.3 They performed “centered cap-preserving” Re-SMILE, dissecting the lower interface and removing a new lenticule through the primary incision: This new lenticule was 0.2 mm smaller in diameter than the primary lenticule. After Re-SMILE, 89.9 percent of study eyes achieved 0.3 logMAR (6/12).
Dr. Sedky uses surface ablation for SMILE retreatments under 0.75 D, but performs the new procedure on SMILE eyes needing more correction with a minimum residual stromal bed of 250 µm.“We are using this technique in all cases that need an enhancement, as long as they fit the required criteria of being myopic, with or without astigmatism, have enough residual corneal stroma and have myopia of at least 0.75 D. We are in the process of publishing another series of cases,” he reports. REVIEW
Dr. Reinstein is a consultant for Carl Zeiss Meditec and has a proprietary interest in the Artemis VHF ultrasound technology. Dr. Sedky has received speaker fees from Alcon and travel support from Abbott Medical Optics/Johnson & Johnson Vision.
1. Reinstein DZ, Carp GI, Archer TJ, Vida RS. Inferior pseudo-hinge fulcrum technique and intraoperative complications of laser in situ keratomileusis retreatment after small-incision lenticule extraction. J Cataract Refract Surg 2018;44:1355-1362.
2. Reinstein DZ, Carp GI, Archer TJ, Vida RS. Outcomes of re-treatment by LASIK after SMILE. J Refract Surg 2018;34:578-588.
3. Sedky AN, Wahba SS, Roshdy MM, Ayaad NR. Cap-preserving SMILE enhancement surgery. BMC Ophthalmol 2018;18:49.
4. Reinstein DZ, Archer TJ, Gobbe M. Accuracy and reproducibility of cap thickness in small incision lenticule extraction. J Refract Surg 2013;29:810-815.
5. Donate D, Thaeron R. Preliminary evidence of successful enhancement after a primary SMILE procedure with the sub-cap-lenticule-extraction technique. J Refract Surg 2015;31:708-710.