Having an intraocular lens decenter or drop into the anterior vitreous, days or years after cataract surgery, is an infrequent but onerous complication for surgeons to deal with. There are many options and plans of attack to consider, including the possibility of performing a limited vitrectomy. In this article, expert implant surgeons discuss the techniques that work best for them when they decide that a displaced IOL is worth salvaging.
Milder Malpositions
When approaching relatively mildly displaced intraocular lenses, surgeons often break them down into several categories:
• Decentered lens in the capsule. Here, the bag is in place but the lens is malpositioned inside it. “These are usually plate haptic lenses, or lenses in which there is a malformation of the haptic or a missing haptic,” explains Richard Hoffman, MD, of Eugene, Ore. “For this scenario, I’ll usually viscodissect the bag open and rotate the lens 90 degrees. Usually, at that point the lens will stay centered, especially if it’s a plate lens. If it doesn’t stay centered, you can capture the optic through the anterior rhexis and center it. However, I’ve never had to do that when the lens is in the bag and decentered.”
• Lens partially out of the capsule. In this scenario, one haptic is in the capsular bag while the other is outside of it. “Usually, these lenses have to be dealt with because the haptic that’s out of the bag is rubbing against the iris and causing problems,” Dr. Hoffman says. “However, the approach for this is similar to that for a decentered lens in the capsule: You can usually get the bag viscodissected open and then reposition the lens within the bag.”
|
“In this situation, if the anterior capsule is intact, I’ll prolapse the optic behind the anterior rhexis, which will center it,” says Dr. Hoffman. “However, if there isn’t an intact rhexis for doing that, I’ll fixate the haptics to the iris with sutures.”
Dr. Hoffman shares his iris suturing technique. “You can do it through two paracenteses,” Dr. Hoffman explains. “First, create a paracentesis and inject a small amount of viscoelastic in the anterior chamber and a small amount behind the optic. Then with a viscoelastic cannula you prolapse the optic forward in front of the iris, leaving the haptics behind the iris. Put some Miochol in the eye to constrict the iris behind the optic. Then, use either a 9-0 or 10-0 Prolene suture on a long curved needle and pass the needle through the paracentesis and then through the peripheral iris, incorporating the haptic.” He secures the sutures with a Siepser knot.
Surgeons warn that the commonly used single-piece, hydrophobic acrylic IOLs shouldn’t be refixated in the ciliary sulcus, due to the risk of uveitis glaucoma hyphema syndrome.1
• Partially malpositioned capsule and lens. Surgeons say long-term pseudoexfoliation is the most common reason for the capsule/lens complex to be displaced but that, in some mild cases, these malpositions can be remedied with a single suture. “One suture around a haptic through the sulcus, pulling the bag and lens in the direction from which it’s falling will be enough to support it,” says West Orange, N.J., surgeon Douglas Grayson. “In a mild decentration case, the eye tends to have intact zonules in the area that the capsule and lens are decentering toward. So the first thing I’ll do is try to suture it through the haptic from the side that’s most displaced. It’s not always easy to do, because you don’t necessarily want to blindly spear from inside to outside because you don’t know what you might be hitting with the needle.
“I always like to spear from the outside in with a double-armed Prolene suture on an STC needle,” Dr. Grayson adds, “and just try to get one suture above the haptic and one below it, come out of the clear corneal wound with the needles or right through peripheral cornea, use a Kuglen hook to externalize the Prolene through the paracentesis site, tie it down and secure it to the sclera in that manner.” Dr. Grayson says he prefers this method to iris fixation. “In my experience, iris fixation often causes a secondary pigment dispersion glaucoma from chafing,” he avers. “I’ve had one or two of these in which patients have developed intractable glaucoma and needed lens explantation, probably with a simultaneous glaucoma filtration procedure.”
Subluxated Lenses
In the more extreme cases of displacement, the bag/lens complex or the lens is in the anterior vitreous. This more complicated scenario will involve a limited vitrectomy and, if the surgeon feels the lens can be salvaged, fixating the lens in the eye. If the lens is sitting on the retina and a full vitrectomy is warranted, however, surgeons recommend the anterior segment surgeon get a retinal specialist involved to perform either the entire case or, at least, the vitrectomy portion.
For complicated dislocations, two of the newest methods for fixating the lens that have emerged over the past several years are the scleral pocket fixation of the sutures, developed by Dr. Hoffman, and fixating the haptics beneath scleral flaps using fibrin glue, described by Amar Agarwal, MD, of Chennai, India.
Before surgeons can use either of those techniques for the subluxed lens, however, a limited vitrectomy will need to be performed. Surgeons also emphasize the necessity of a meticulous retinal exam before and after the limited vitrectomy/lens refixation procedure in these patients, in order to catch any tears or other pathology. Here is how to proceed with the case.
• Pearls for anterior vitrectomy. Cincinnati Eye Institute retinal specialist Christopher Riemann says when the vitreous gets involved, anterior segment surgeons should ask themselves who is the best person or persons to fix it—themselves, the retina specialist or a combination? “This a bigger question than one might think,” he says. “Because there are a lot of surgical videos out there with very involved techniques. That doesn’t necessarily mean these are the right ways to take care of these patients.
“If the lens is decentered in the capsular complex and the eye has already had a complete vitrectomy, then I don’t have a problem with any anterior segment surgeon maneuvering the lens around and getting it where it needs to be,” Dr. Riemann continues. “But issues arise when there’s vitreous present and a limited vitrectomy is called for. Ask, ‘How limited is it going to be?’ ” He has three conditions for what he calls a limited vitrectomy: “If there are a couple strands of vitreous in front and the surgeon will just be cleaning out the front and blowing the rest back with viscoelastic; if the lens is already in the iris plane or ciliary sulcus plane; or if we don’t think it’s luxed posteriorly where its haptics are caught in the vitreous base—in which any tugging on the haptics will result in traction on the retina—then I think it’s fine for an anterior segment surgeon to perform the surgery,” he says.
Dr. Riemann believes there are two acceptable ways to perform the anterior vitrectomy. “First, surgeons can use bimanual anterior segment infusion and anterior segment vitrectomy port entry, both through two paracenteses,” he says. “This is much better than a coaxial, single-wound approach, which is probably the worst technique to use. This is because with the two-paracenteses technique, the vector of the irrigating fluid isn’t directly into the vitreous cavity as it is with coaxial. With two paracenteses, you can do a very nice job of cleaning up a little bit of vitreous in the anterior chamber. If you have to go behind the lens though, you have to kind of go fishing for vitreous, and that, in my mind, can be a little problematic.”
For the safest, most effective anterior vitrectomy, Dr. Riemann thinks surgeons should be working through the pars plana. “I’m a little biased as a retina surgeon, but I think the very best way is with an anterior infusion through a paracentesis and a single pars plana port,” he says. “That is absolutely the right way to do it, because the vector of fluid flow is from front to back in a way that doesn’t hydrate the vitreous. And, the default position is everything falls back to the cutter and puts the cutter where you need it, which is kind of right behind the IOL in that very anterior vitreous space.”
To get the best, safest results, Dr. Riemann recommends a few things. “First, use trocar-based ports,” he says. “They are clearly safer than non-trocar sclerotomies. When you’re using a trocar, the innermost point of the wound is often 3 to 4 mm inside the globe. In this way, you’ve moved away from the vitreous base, thereby reducing vitreous traction.
“Second, I think it’s very important to use the smallest gauge vitrectomy system possible,” Dr. Riemann continues. “There’s no reason for an anterior segment surgeon to use a 20-ga. or 19-ga. vitreous probe through a sclerotomy, when he or she could be using a 23-, 25-, or 27-ga. probe through an appropriately sized trocar. Not only do the smaller gauges seal better, but their risk of iatrogenic retinal breaks is much lower when used with the trocar entry port.
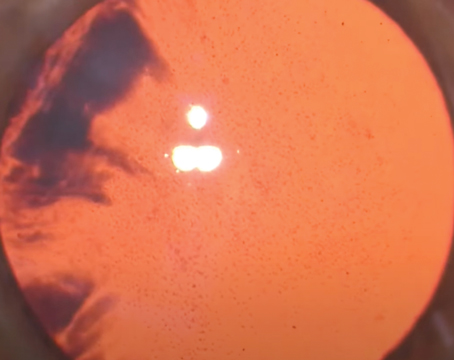
“Third, the highest possible cut rate is always better than the lowest, and very conservative vacuum settings should be used, because the more you pull, the more likely you are to create retinal breaks,” Dr. Riemann continues. “A good starting point for 20-ga. surgery would be a vacuum of 100 to 150 mmHg; for 23-ga. it’s 150 to 250; for 25-ga. it’s 300 to 400; and for 27-ga. it’s 400 to 500 mmHg.” Additionally, Dr. Riemann says that an injection of diluted triamcinolone before the vitrectomy will help mark the vitreous strands to make it easier to remove them.
For whichever suture technique follows, Dr. Riemann doesn’t feel 10-0 Prolene is appropriate. “10-0 Prolene has a high breakage rate after about 10 to 12 years,” he says. “After which you’re back in the eye trying to suture refixate. 9-0 Prolene is the minimum size. Another option is Gore-Tex, which isn’t actually approved for ophthalmic use, but has worked well for myself and many of my partners.”
• Scleral pocket technique. This technique has found favor with surgeons because it avoids the need for conjunctival dissection and scleral cautery that are used in previous techniques. It also has the potential to leave a healthy bit of sclera above the suture, to prevent erosion. Dr. Hoffman explains the technique:
| ||||||
“You make a 350-µm deep groove in a meridian that allows you to fixate the haptic to the sclera,” Dr. Hoffman continues. “Then you dissect that groove posteriorly in the plane of the sclera, going back about 3 mm. This creates the scleral pockets. Then you make a paracentesis in front of each pocket, and pass a double-armed, 9-0 Prolene suture through the paracentesis and dock it into a 27-ga. needle that’s passed through the full thickness of the globe corresponding to where that pocket is. (See Figure 1, p. 31) The first double-armed suture would go in front of the bag, or through it, and the second one would go the other way, so that one passes through the bag and the other passes in front of it. The pass going through the bag is really going behind the haptic, so that when you pull that suture into the eye, it’s looped around the IOL haptic. So you pass the 27-ga. needle about 2 mm posterior to the surgical limbus, which is perhaps 3 mm from where the conjunctival insertion is, and then you pass the second 27-ga. needle right next to that—or just in front of it—but I usually just do it next to it so that the suture’s going through the bag and in front of the bag and out through the full thickness of the globe. If you can’t visualize the capsular bag equator, you can put a hook in through the paracentesis that’s just in front of the pocket while you’re passing the needles from the opposite paracentesis and docking the sutures into the 27-ga. needles.
“Then, you take the needles off the sutures,” Dr. Hoffman explains, “go into the pocket with a Sinskey hook and pull both ends out so that they’re externalized through the opening in the scleral pocket, and then tighten and tie those. That allows the knot to slide under the protective roof of the scleral pocket so that it’s less likely to erode through the sclera and the conjunctiva. You then do the same thing for the other side. The docking technique isn’t my technique, and has been described by several other surgeons, including Javier Moreno-Montañés, MD; Ike Ahmed, MD; and Alan Crandall, MD. My contribution to this is the scleral pockets—which have the advantage that you don’t have to dissect the conjunctiva. Therefore, I believe that the tissue is healthier and is much less likely to erode over the underlying knot that’s created.” For a video of the technique as performed by Los Angeles surgeon Sam Masket, visit
https://www.youtube.com/watch?v=McwNhj-PMmo.
• Glued haptic technique. Dr. Agarwal says adding glue to the scleral incarceration of the haptics results in a more stable lens. (The technique of scleral incarceration, but without glue, was originally described by Recklinghausen, Germany’s Gábor Scharioth, MD, PhD.) “There is no pseudophacodonesis as might occur if the haptics were just sutured,” Dr. Agarwal says. “Since the haptics are glued under scleral flaps rather than sutured, the lens doesn’t move postop. As a result, the quality of vision is very good. The only instance in which I can’t use the glue technique is if it’s a single-piece, foldable IOL. In that case, I’ll explant the lens and refixate a new lens in the eye.”
|
In this technique, Dr. Agarwal says it’s crucial to grab the tip of the trailing haptic when externalizing it, since grasping the middle of the haptic and trying to pull it out of the eye could break it. To make this easier, Dr. Agarwal developed the “handshake” technique. In this technique, the surgeon flexes the second haptic into the anterior chamber and into the grip of the second forceps introduced through the other sclerotomy. He then passes the haptic from one forceps to the other until the tip is properly grasped for externalization.
In terms of complications, Dr. Agarwal recently completed a study of eyes done with the glued-IOL technique with an average follow-up of 17 months. In 191 foldable lenses, the most common complication was optic capture (5.7 percent). IOL decentration occurred in 2.6 percent of eyes. Haptic-related complications in the late postop period were haptic displacement (2 percent), tip extrusion (0.5 percent) and subconjunctival haptic (1.5 percent).2
“By and large, these eyes are very quiet postop,” says Dr. Agarwal. “This is because the lens doesn’t move. Because of that, the vitreous and other structures remain quiet when compared to an iris-sutured IOL, a scleral sutured lens or an anterior chamber IOL.” For a video of the technique, visit
https://www.youtube.com/watch?v=UYZkHPojJ7Y.
• Snyder half-hitch suture. Dr. Grayson says working with externalizing the haptics and creating channels can be technically complex, and is not for everyone. “I do a lot of precision surgery because I’m primarily a glaucoma specialist, so I’m used to suturing and manipulating in the eye, and I still find some of these maneuvers difficult to do,” he says. Instead, he’s had success with rotational knots such as those used in a half-hitch suture technique described by Cincinnati Eye Institute’s Michael Snyder, MD. Dr. Riemann, who works with Dr. Snyder, also uses the technique.
“You make two beveled sclerotomies into the ciliary sulcus that are quite some distance apart,” Dr. Riemann explains. “Personally, I use vitrectomy trocars instead of sclerotomies. You then place a half-hitch suture around the haptic and move in a radial direction from the knot, which creates tension that tends to pull the lens parallel. You come out through the sclerotomies, or the trocars, then tie the knot and rotate the lens in such a way that it is rotated as far counterclockwise as possible, then tie the knot on the outside of the eye over the most counter-clockwise sclerotomy.
Once the knot is tied and secured, you can rotate the entire knot into the eye through the sclerotomy. In that way, you’re actually sliding the haptic in a clockwise fashion—actually slightly rotating the lens clockwise—so not only does that make the suture knot disappear on the inside of the eye, completely burying it, it also lets you adjust the centration of the lens by rotating each knot.” For a video of the technique, visit
revophth.com/Snyder_Suture.
Whichever technique you choose to use for managing a malpositioned lens, Dr. Grayson says that education and practice are key. “These are complex procedures, and are almost a dying art,” he says. “I’m not sure how many times during a residency a resident is taught these suture techniques, because there is no suturing left in cataract surgery, but you need to get the feel of regularly handling sutures.” REVIEW
1. LeBoyer RM, Werner L, Snyder ME. Acute haptic-induced ciliary sulcus irritation associated with single-piece AcrySof intraocular lenses. J Cataract Refract Surg 2005;31:7:1421-7.
2. In press: Kumar DA, Agarwal A. Glued intraocular lens: A major review on surgical technique and results. Curr Opin Ophthalmol 2012;23.