|
The Advantages
The laser uses near-infrared light to cut corneal tissue via photodisruption, which provides nonplanar cuts at a precise depth and pattern with minimal damage to surrounding tissue. The femtosecond laser cuts are consistent and reproducible, allowing for the creation of a variety of incision types using combinations of lamellar and vertical cuts. Additionally, the femtosecond laser has the ability to create straight cuts in complex shapes, such as decagonal and circular.
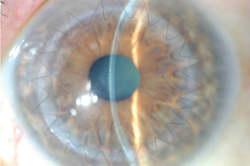
The “top-hat” was the first customized trephination pattern using the femtosecond laser. Studies have shown that this shape led to increased biomechanical wound stability with a sevenfold increase in resistance to leakage and possibly less astigmatism than traditional trephination PKP wounds.1,2 Today, corneal surgeons have a variety of trephination patterns to choose from, including the top-hat, mushroom, zigzag and Christmas tree shapes. All of these wound configurations create more surface area for healing and have better biomechanical strength than the traditional butt joint. The increased surface area of these incisions leads to improved tensile wound strength, which improves patient safety and allows for earlier suture removal, when indicated.
Factors preventing optimal outcomes in PKP include donor-host misalignment of the anterior surface; rotational misalignment and poor tissue distribution; excess and uneven suture tension; and slow and uneven wound healing. Using the femtosecond laser has allowed for certain improvements in these variable factors and has improved optical and mechanical outcomes.
Femtosecond laser-assisted PKP has demonstrated better natural alignment of the donor and host anterior surface, reducing one source of distortion. Additionally, improved sealing of the incision allows surgeons to use only enough suture tension to keep the incision apposed, which reduces distortion from the suture itself. Studies have also shown that femtosecond laser-assisted PKP provides rapid visual recovery and astigmatism amounts comparable to or slightly better than traditional blade trephination PKP.3-7
Patient Selection for PKP
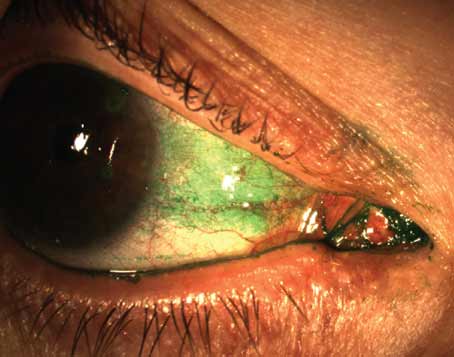
Careful patient selection is the key to successful outcomes. Patients who have conditions that prevent proper laser applanation and suction are not good candidates for this procedure. Additionally, although the femtosecond laser has excellent cut penetration even through dense scars, severe peripheral corneal neovascularization may be a contraindication in certain cases. Small orbits or narrow palpebral fissures may not be able to accommodate the limbal suction ring required for laser use.
|
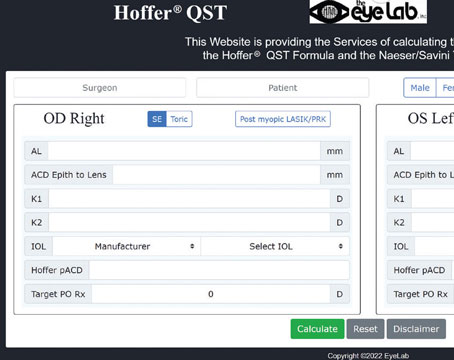
When choosing the graft size, consider the host corneal diameter (especially vertical), location of thinning or active corneal infection, and the presence of prior graft. In patients with ectasia, especially pellucid marginal degeneration, large or eccentric grafts may be needed. After the laser cut and before tissue removal, a posterior bridge of uncut tissue will maintain a closed eye and a formed anterior chamber. Therefore, accurate preoperative pachymetry is often crucial in cases where deep anterior lamellar keratoplasty is to be attempted, or, as is usually the case, in cases where the femtosecond laser is not located in the operating suite and corneal stability is required during the time between laser cut and corneal removal. Optical coherence tomography, Pentacam or ultrasound is used to check and program depth settings for the femtosecond laser incision.
Cutting the Graft and Surgery
The next step is graft cutting. The tissue is mounted on an anterior artificial chamber, and donor corneas are cut by the femtosecond laser using preprogrammed parameters set by the surgeon. Another option is to order the tissue from the eye bank pre-cut with the same laser parameters as those to be used on the patient. The donor tissue diameter should be the same size as the host. The host laser cut can be performed under topical or retrobulbar anesthesia. However, more complex cutting patterns and alignment marks have increased the amount of time the suction ring remains on the eye, so many surgeons prefer using a preoperative retrobulbar block to ensure patient comfort.
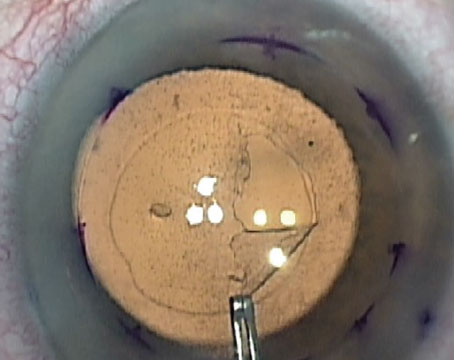
Proper centration of the suction ring is the key to proper centration of the graft. The surgeon chooses a customized trephination pattern and programs it into the laser computer. The laser pattern always starts from the deepest part of the cornea and moves anteriorly. The IntraLase laser allows for a maximum diameter of 9 mm, with the ability to vary the side-cut angle from 30 degrees to 150 degrees.
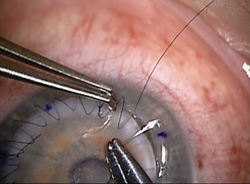
As an example, with a zigzag incision, the laser parameters are a posterior side cut from deep stroma to anterior stroma at 30 degrees to the periphery and a second lamellar cut at a depth of 320 μm from the anterior surface. The second incision is intersected by the third incision, which is an anterior side cut that advances toward the anterior corneal surface at 30 degrees. The zigzag cut can have an anterior diameter of 8, 8.5 or 9 mm, based on the patient’s corneal diameter and the surgeon’s preference. Additionally, radial alignment marks are made on the host and donor corneas that facilitate precise suture placement and improved tissue distribution.
|
If the surgeon sees small bubbles when the laser treatment is started, then the laser energy is in the anterior chamber fluid, and a full-thickness incision is under way. If this was not your intention, just lift your foot off the foot pedal, and the laser will stop. As long as the laser has not reached Descemet’s membrane, then the posterior depth can be reset, and the laser can be restarted within the posterior corneal stroma to maintain a bridge of uncut tissue.
If it is necessary to move the patient to the operating room after the laser corneal cut, globe stability can be ensured via a posterior bridge of uncut corneal tissue. Studies have shown that side-cut bridges are stronger than lamellar bridges. However, both types of bridges are stronger than full-thickness cuts. Posterior side-cut bridges are preferred over anterior side-cut bridges to minimize irregularities in the anterior contour and poor anterior graft-host fit. Additionally, posterior side-cut bridges offer the benefit of being easily extended with a blade into the anterior chamber without compromising the laser cut shape.
After the incision is made, the eye is treated with antibiotic drops and is shielded. Then, the patient is moved to the operating room. The host corneal button is separated with a blunt lamellar dissector to reveal lamellar and side-cut incisions made by the laser. Laser incisions usually separate cleanly; however, in some cases with dense corneal scarring, limited sharp dissection with a surgical blade or scissors may be needed. After blunt dissection, the blade enters the anterior chamber, and the corneal bridging tissue is cut with corneal scissors. The surgeon then sutures the donor cornea into place using his pattern of choice. Make sure to match the depth of the suture in the donor and host to ensure a lock and key fit.
Multiple studies have shown that endothelial cell loss, postoperative astigmatism and best spectacle-corrected visual acuity in femtosecond-laser assisted PKP are better than or equal to conventional PKP.5-7
The top-hat and zigzag incision patterns are the most popular. One main advantage of femtosecond laser-assisted keratoplasty compared with traditional PKP is the accuracy of the fit between the donor and the host corneas. For this reason, the zigzag pattern may be the most biomechanically sound because it allows for consistent suture placement at approximately 50 percent depth, where the posterior side-cut and lamellar incisions intersect. In contrast, with the top-hat pattern, suture placement can vary, allowing the possibility of posterior wound gape. With the zigzag pattern, sutures are placed at the inner point of the Z, which provides good wound apposition at the deeper layers and anterior cornea.
At my institution, in a review of 173 eyes having undergone femtosecond laser keratoplasty, the average manifest astigmatism was less than or equal to 3 D, and average topographic astigmatism was less than or equal to 4 D as early three months postoperatively. This remained the case throughout the two-year follow-up period.
Femto Lamellar Keratoplasty
In addition to full-thickness keratoplasty, the femtosecond laser can be used for other forms of corneal transplantation, such as DALK, anterior lamellar keratoplasty (ALK), Descemet’s stripping endothelial keratoplasty (DSEK), and deep lamellar endothelial keratoplasty (DLEK).
|
DALK for stromal corneal pathology and ectatic corneal disease provides many benefits, making it preferable to traditional PKP. Benefits include the safety of extraocular surgery, no risk of endothelial rejection due to preservation of the host endothelium, and a shorter postoperative course of topical corticosteroids. Although epithelial and stromal rejection is rare, surgeons still need to look for it.
Unfortunately, DALK with the zigzag pattern has a high failure rate of big bubble dissection. One solution is femtosecond laser pre-Descemet deep lamellar dissection. A smooth dissection is obtained by an ultralow energy multipass technique with the 150 kHz iFS IntraLase laser. The irregular ridges of previous deep corneal lamellar FS dissections are avoided.
ALK can be used for patients with relatively anterior pathology, including scars and anterior dystrophies. A sutureless technique using the femtosecond laser to create smooth lamellar dissections just inferior to the corneal pathology has been described.8
DSEK allows surgeons to replace diseased host endothelium while retaining normal stroma and epithelium. The procedure offers decreased healing time, decreased astigmatism and a predictable change in corneal power.
Additional studies are under way to assess various energy and spot size patterns of the femtosecond laser and to use multiple passes to create a smoother donor bed. REVIEW
Dr. Steinert is the Irving H. Leopold Professor and Chair of Ophthalmology, professor of biomedical engineering, and director of the Gavin Herbert Eye Institute at the University of California, Irvine.
1. Ignacio TS, Nguyen TB, Chuck RS, et al. Top-hat wound configuration for penetrating keratoplasty using the femtosecond laser: a laboratory model. Cornea 2006;25:336-340.
2. Steinert RF, Ignacio TS, Sarayba MA. Top-hat shaped penetrating keratoplasty using the femtosecond laser. Am J Ophthalmol 2007;143:689-691.
3. Farid M, Kim M, Steinert RF. Results of penetrating keratoplasty performed with a femtosecond laser zigzag incision: initial report. Ophthalmology 2007;114:2208-2212.
4. Buratto L, Böhm E. The use of the femtosecond laser in penetrating keratoplasty. Am J Ophthalmol 2007;143:737-742.
5. Price FW, Price MO. Femtosecond laser shaped penetrating keratoplasty: One-year results utilizing a top-hat configuration. Am J Ophthalmol 2008;145:210-214.
6. Cheng YY, Tahzib NG, van Rij G, et al. Femtosecond laser-assisted inverted mushroom keratoplasty. Cornea 2008;27:679-685.
7. Bahar I, Kaiserman I, Lange AP, et al. Femtosecond laser versus manual dissection for top-hat penetrating keratoplasty. Br J Ophthalmol 2009;93(1):73-78.
8. Yoo SH, Kymionis GD, Koreishi A, et al. Femtosecond laser assisted sutureless anterior lamellar keratoplasty. Ophthalmology 2008;115:1303-1307.