Ophthalmologists can agree on one point: The bottom line for patients is how their visual symptoms affect their daily tasks. While eyesight can be devastated by diseases such as cataract and macular degeneration, the ocular surface changes brought on by dry eye can also be an obstacle to a patient’s visual functioning and can severely affect what we now know is one critical aspect of disease management: quality of life. Dry eye-induced changes in visual function are more subtle and transient compared to permanent vision loss, yet tasks such as driving, watching television and especially reading can be profoundly affected,1 and these detrimental effects on visual function are now widely accepted.1-4 Among daily tasks, reading remains one of the most important.
In this article, we’ll take a look at how we assess reading performance, how objective reading tests differ and which tests may be more applicable to measuring subtle changes incurred by ocular surface damage.
Dry Eye’s Effects
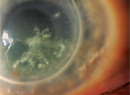
Three phenomena account for visual disturbances in dry eye: tear-film breakup; increased blink rate; and corneal desiccation. The tear film is necessarily transparent, a complex and dynamic cocktail of lipids, water, solutes and mucins that is constantly refreshed with every blink, spreading over the exposed anterior surface of the eye and ensuring clarity, comfort and defense against infection. Dysfunction of any single component will destabilize the tear film, causing it to thin and eventually break up on the corneal surface, leading to evaporation and visual distortion.5 This degradation occurs even in normal individuals in states of prolonged staring or in tasks of heightened concentration that necessitate suppressing blink rate,6 and we all know shortened time to tear-film breakup is a routine diagnostic indicator for dry eye. The drying cornea sends out signals stimulating blinking, in a defensive effort to refresh tears. When tear-film instability occurs repeatedly, the cornea is compromised and cells begin to die, becoming observable with fluorescein staining. These areas of damage, particularly in the central cornea,7 can chronically disturb visual function already hindered by an increased blink rate.8
How do we measure these subtle changes in visual function in dry eye? How can we determine that a tear substitute or disease-modifying therapeutic is improving visual function? One endpoint is blurred vision, a symptom patients are routinely surveyed about in clinical trials as part of an overall visual assessment. The other widely implemented instrument is the QoL questionnaire, which includes questions addressing visual function as well as other symptom assessments. Examples of questionnaires include the Ocular Surface Disease Index,7 the National Eye Institute Visual Functioning Questionnaire,8 the Standard Patient Evaluation of Eye Dryness,9 the Impact of Dry Eye on Everyday Life10 and the Dry Eye Questionnaire.11 All are used quite frequently in clinical trials. We have developed a simple five-part questionnaire, the Dry Eye Quality of Life Questionnaire, in which one domain specifically queries the disturbance in visual tasking graded by frequency and severity of occurrence. (Pollard S, et al. IOVS 2004;45:ARVO E-Abstract 82) The daily activity most influenced by dry eye was found to be reading, as reported by 73.5 percent of dry-eye patients. Despite their value, a drawback of all these questionnaires is that they rely on subjective memory, much like patient diaries.
Reading as a Clinical Endpoint
Recent work has taken visual function assessment one step further by comparing reading tasks in dry-eye and normal subjects. Previous studies at Ora have examined blink alterations in dry eye and visual acuity decay at distance vision using the interblink interval visual acuity decay test.12 Other studies assessed menu and normal reading rates as possible links to visual function, particularly in subjects with central corneal staining.13 One recently published study by Fullerton, Calif., researcher William H. Ridder, OD, PhD, confirmed our previous finding that reading rates were lower in dry-eye versus normal subjects.14 Tokyo’s Katzuo Tsubota, MD, and co-workers have also recently published studies demonstrating that their visual acuity decay metric is modifiable with treatment.15,16
Reading tests can be broken down into three main categories: 1) those that are used in education to gauge linguistic development, in which reading comprehension and reading age are important metrics; 2) those that assess reading acuity, or critical print size at which a subject can accurately read text, and which might be more applicable to low-vision contexts; and 3) reading speed, which appears to be the endpoint that might most accurately reflect subtle changes in visual function.
Reading acuity tests include the Sloan M cards,17 the Pepper Visual Skills for Reading Test,18 the Minnesota Low Vision Reading Test (MNREAD)19 and the Radner Reading Charts.20 The Sloan M cards were designed to measure reading at the subject’s acuity print size, and are not intended for use with magnification, and are, therefore, of limited use in low-vision assessments. The Pepper Visual Skills for Reading Test evaluates reading in the subject’s preferred lighting, magnification and viewing distance (character size) to provide a more accurate assessment of how low vision interferes with everyday reading in situ.
The MNREAD is the most cited of the acuity tests, and consists of single simple sentences with equal numbers of characters. The sentences use a syntactical structure and vocabulary at the second to fifth grade level to minimize cognitive and lexical demands, and are repeated in decreasing order of size. By plotting reading speed against print size, a function is created with a large plateau of peak reading speed and a decline for text presented at smaller or very large print sizes. The MNREAD is computer-based, although a printed card version is also available.20 This test is aimed at low-vision readers and might not be sensitive enough for assessments of normal-range, dry-eye readers.
The Radner Reading Charts were developed on the basis of the concept of reading optotypes for the standardized measurement of both reading acuity and speed. Print sizes are logarithmically scaled (logRAD) to permit statistical analysis, and results obtained can be compared to other logarithmically scaled vision systems (e.g., logMAR). To guarantee accurate, reproducible and standardized measurements of reading acuity and speed at every viewing distance, these sentence optotypes were created to minimize variation and to keep the geometric proportions as constant as possible at all distances. A series of test sentences was developed. The sentences are highly comparable in terms of the number of words (14 words), word length, number of syllables, position of words, lexical difficulty and syntactical complexity. The Radner test has an advantage over other reading acuity tests in that it can also be used to define reading speed.20
Standardized paragraph texts, known as IReST, have been developed in multiple languages by Susanne Trauzettel-Klosinski, MD, and co-workers at the University of Tubingen in Germany.22 This test might be a more appropriate standardized means of assessing reading speed than sentence-based tests. The argument is that continuous text is a better predictor of real-world reading performance, though sentences must be standardized and homogenous in syntax and character length. Texts have been developed by linguistic experts to obtain low within-subject variability among passages. The authors suggest their use as an endpoint before and after interventions. Standardization across languages is an added advantage that allows this tool to be used in international clinical trials.
The Wilkins Rate of Reading Test consists of a paragraph of simple words without context or punctuation, read out loud, with time and errors counted.23 It was originally developed for the testing of disabled readers or children, and to gauge the effect that colored overlays have on reading. Many visual difficulties with reading seem to emerge when text is presented in a long paragraph with closely spaced lines and letters. The theory of visual stress, proposed by Arnold Wilkins, PhD, at the University of Essex in England, is based on the fact that certain patterns or stripes can induce seizures, migraine and perceptual distortions in susceptible subjects. The test is designed to compare an individual’s performance under one set of conditions with that of another, and thus might be suitable for evaluation before and after an adverse environmental challenge or therapeutic manipulation.
At Ora, we implement a Controlled Adverse Environment to exacerbate a patient’s signs and symptoms of dry eye under highly controlled conditions, testing how these and associated endpoints like reading are affected by treatment. The Wilkins test is unique in that it is not designed to compare one individual subject with others of the same age or ability. In fact, reading tests are generally most useful when performed before and after treatment, and not across parallel groups, unlike the conventional, statistical comparative method used in most clinical trials in dry eye. A change from baseline reading rate as a primary endpoint would eliminate the considerable internal variables inherent in reading rate.
We have studied dry-eye and normal subjects using the MNREAD, Radner, Wilkins and IReST tests, modifying them to our specific needs. Changes include assessing blink rates during testing, measuring signs and symptoms of dry eye before and after tests, or the addition of forced-stare and altered contrast sensitivity reading tests. One problem when entering the realm of visual function tests is the potential confounding variability that lies in the psychomotor and neurocognitive functioning of subjects.24 Factors such as age, education, depression, mild neurocognitive loss24 and fatigue and/or sleepiness in particular25 must therefore be carefully monitored, as they can affect the outcome of these visual function tests, particularly in the aging dry-eye population. To assure a stable baseline and minimize these known confounding variables, we combine these reading tests with tests of sleepiness, fatigue, depression and basic neurocognitive function. Results have been promising, demonstrating not only the ability to distinguish between dry-eye and normal subjects but also to detect improvements in testing after tear substitute use.
With Food and Drug Administration recognition of the dissociation of symptom alleviation from significant sign improvement in dry eye,26 and the extreme difficulty in proving that a dry-eye therapeutic is effective for either of these conventional endpoints, reading might prove to be a clinically relevant future endpoint in dry-eye clinical trials. The unique combination of quality of life, patient-reported outcomes and signs such as tear-film breakup and keratitis that coalesce in a global assessment such as reading could provide us with a concrete way to gauge improvement in a patient’s life; and that, ultimately, is what patients are searching for when they step into our offices.
REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Ms. Smith is a medical writer at Ora Inc.
1. Milanovic B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol 2007;143:409-415.
2. Li M, Gong L, Chapin WJ, Zhu M. Assessment of vision-related quality of life in dry eye patients. Invest Ophthalmol Vis Sci 2012;53:5722-7.
3. Le Q, Zhou X, Ge L, et al. Impact of dry eye syndrome on vision-related quality of life in a non-clinic-based general population. BMC Ophthal. 2012;12:22.
4. Mizuno Y, Yamada M, Miyake Y, Dry Eye Survey Group of the National Hospital Organization of Japan. Jpn J Ophthalmol 2010;54:259-65.
5. International Dry Eye Workshop. The definition and classification of dry eye disease: Report of the International Dry Eye Workshop (2007). Ocul Surf 2007;5:75-92.
6. Cadona G, Garcia C, Seres C, Vilesca M, Gispets J. Blink rate, blink amplitude, and tear film integrity during dynamic visual display terminal tasks. Curr Eye Res 2011; 36:3:190-197.
7. Schiffman RH, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol 2000; 118:615-621.
8. Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD, for the NEI-VFQ Field Test Investigators. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NE)-VFQ). Arch Ophthalmol 1998; 116:1496-1504.
9. Ngo W, Situ P, Keir N, Korb D, Blackie C, Simpson T. Psychometric properties and validation of the Standard Patient Evaluation of Eye Dryness questionnaire. Cornea 2013;32:1204-10.
10. Abetz L, Rajagopalan K, Mertzanis P, Begley C, Barnes R, Chalmers R, for the impact of dry eye on everyday life (IDEEL) Study Group. Health and Quality of Life Outcomes 2011; 9:111.
11. Begley CG, Chalmers RL, Abetz L, et al. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity. Invest Ophthalmol Vis Sci 2003;44:11:4753-61.
12. Torkildsen G. The effects of lubricant eye drops on visual function as measured by the Inter-blink inverval Visual Acuity Decay test. Clin Ophthalmol 2009; 3:501-6.
13. Walker PM, Lane KL, Ousler GW 3rd, Abelson MB. Diurnal variation of visual function and the signs and symptoms of dry eye. Cornea. 2010; 29:6:607–612.
14. Ridder WH, Zhang Y. Evaluation of reading speed and contrast sensitivity in dry eye disease. Optom Vis Sci 2012; 90.
15. Kaido M, Ishida R, Dogru M, Tsubota K. The relation of functional visual acuity measurement methodology to tear functions and ocular surface status. Jpn J Ophthalmol 2011; 55:5:451-9.
16. Hirayama M, Murat D, Liu Y, Kojima T, Kawakita T, Tsubota K. Efficacy of a novel moist cool air device in office workers with dry eye disease. Acta Ophthalmol 2012 Dec 24. doi: 10.1111/j.1755-3768.2012.02485.x.
17. Sloan LL, Brown DJ. Reading cards for selection of optical aids for the partially sighted. Am J Ophthalmol 1963; 55:1187.
18. Baldasare J, Watson GR, Whittaker SG, Miller-Schafer H. The development and evaluation of a reading test for low vision individuals with macular loss. J Vis Impairment and Blindness 1986;80:785-789.
19. Legge GE, Ross JA, Luebker A, LaMay JM. Psychophysics of reading. VIII. The Minnesota Low-Vision Reading Test. Optom Vis Sci 1989;66:12:843-853.
20. Stifler E, Konig F, Lang T, et al. Reliability of a standardized reading chart system: Variance component analysis, test-retest and interchart reliability. Graefes Arch Clin Exp Ophthalmol 2004;242:1:31-9.
21. Ahn SJ, Legge GE, Luebker A. Printed reading cards for measuring low vision reading speed. Vision Res 1995; 35:13:1939-1944.
22. Trauzattel-Klosinski S, Dietz K, and the IRsST Study Group. Standardized assessment of reading performance: The new international reading speed texts IReST. Invest Ophthalmol Vis Sci 2012;53:5452-5461.
23. Wilkins AJ, Jeanes RJ, Pumfrey PD, Laskier M. Rate of Reading Test: Its reliability, and its validity in the assessment of the effects of coloured overlays. Ophthal Physiol Opt 1996;16:6:491-497.
24. Soederberg Miller LM. Age differences in the effects of domain knowledge on reading efficiency. Psychol Aging 2009;24:1:63-74.
25.Schleicher R, Galley N, Briest S, Galley L. Blinks and saccades as indicators of fatigue in sleepiness warnings: Looking tired? Ergonomics 2008;51:7:982-1010.
26. Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease. Cornea 2004;23:8:762-70.