A group of surgeons from Los Angeles, Seoul, South Korea and Milan say that, though cataract surgery tends to lower patients’ intraocular pressure, it doesn’t seem to have a similar beneficial effect on glaucoma patients’ visual field progression postop.
In the study, consecutive open-angle glaucoma patients who underwent cataract surgery and who had at least four visual field tests and at least three years of follow-up before and after surgery were retrospectively reviewed. Mean deviation (MD) rate, visual field index (VFI) rate, pointwise linear regression (PLR), pointwise rate of change (PRC), and the Glaucoma Rate Index (GRI) were compared before and after cataract surgery.
A total of 134 eyes of 99 patients were included. Median (interquartile range) follow-up was 6.5 (4.7 to 8.1) and 5.3 (4.0 to 7.3) years before and after cataract surgery, respectively.
All intraocular-pressure parameters (mean IOP, standard deviation of IOP, and peak IOP) significantly improved (p<0.001) after cataract surgery, but all VF indices indicated an accelerated VF decay rate after cataract surgery:
• MD rate (-0.18 ±0.40 dB/year vs. -0.40 ±0.62 dB/year, p<0.001);
• VFI rate (-0.44 percent ±1.09 percent/year vs -1.19 percent ±1.85 percent/year, p<0.001);
• GRI (-5.5 ±10.8 vs -13.5 ±21.5; p<0.001); and
• PRC (-0.62 percent ±2.47 percent/year before and -1.35 percent ±3.71 percent/year after surgery; p<0.001); and PLR (-0.20 ±0.82 dB/year before and -0.42 ±1.16 dB/year after surgery; p<0.001) for all VF locations.
Worse baseline MD and postoperative peak IOP were significantly associated with the postoperative VF decay rate and the change in the decay rate after cataract surgery.
The researchers concluded that cataract surgery didn’t slow the rate of visual field decay when compared to the rate before cataract surgery was performed.
Am J Ophthalmol. 2019;201:19-30
Kim JH, Rabiolo A, Morales E, et al.
Unilateral Endothelial Keratoplasty and Quality of Life
 |
|
|
In the primary Descemet Endothelial Thickness Comparison Trial, Descemet’s membrane endothelial keratoplasty led to superior postoperative visual acuity compared with ultrathin Descemet’s stripping automated endothelial keratoplasty. Investigators aimed to determine the effect of DMEK and UT-DSAEK on vision-related quality of life.
A prespecified, secondary analysis of a two-surgeon, patient- and outcome-masked randomized clinical trial was conducted at the Casey Eye Institute in Portland, Oregon, and Byers Eye Institute in Palo Alto, California. The study was conducted between January 20, 2015, and April 26, 2017. The study enrolled 38 individuals and included 50 eyes with isolated endothelial dysfunction. Study eyes were randomized to receive either UT-DSAEK or DMEK. Responses to the National Eye Institute Visual Function Questionnaire-39 administered at baseline, and three and 12 months postoperatively were analyzed using the NEI-defined traditional subscales and composite score on a 100-point scale and with a Rasch-refined analysis.
The second eye from a single participant was excluded, along with any questionnaires relating to the first eye after second eye surgery, for evaluation of 38 eyes at baseline and three months, and 26 eyes at 12 months. Mean baseline visual acuity was 0.35 ±0.31 logMAR in the DMEK arm and 0.28 ±0.22 logMAR in the UT-DSAEK arm. Each arm consisted of 19 participants: 18 individuals with Fuchs’ dystrophy and one participant with pseudophakic bullous keratopathy.
More women participated in both arms of the study (UT-DSAEK: 12 [63 percent]; DMEK: 11 [58 percent]); and mean age was 68 ±11 years in the UT-DSAEK arm and 68 ±4 years in the DMEK arm. Here are some of the findings:
• Overall, study participants experienced a 9.1-point improvement in NEI VFQ-39 composite score at three months compared with baseline (n=38; CI, 4.9 to 13.3; p<0.001), and an 11.6-point improvement at 12 months compared with baseline (n=26; CI, 6.8 to 16.4; p<0.001).
• Eyes randomized to DMEK had only 0.9 points more improvement in NEI VFQ-39 composite score at three months compared with UT-DSAEK after controlling for baseline NEI VFQ-39 (-6.2 to 8.0; p=0.80).
Investigators concluded that improvement in vision-related quality of life wasn’t shown to be greater with DMEK than with UT-DSAEK.
JAMA Ophthalmol 2019; May 2. [Epub ahead of print]
Ang MJ, Chamberlain W, Lin CC, et al.
Anterior Chamber IOL vs. Sutured PC-IOL Post Vitrectomy
Surgeons from the East and West Coasts contributed another datapoint to the perennial debate about anterior chamber intraocular lenses vs. scleral-sutured posterior-chamber IOLs after pars plana vitrectomy.
The study was a retrospective, interventional case series of eyes undergoing combined PPV and IOL placement for retained lens material, aphakia or dislocated IOL. Eyes with a history of amblyopia, corneal opacity or retinal or optic nerve disease were excluded. Outcome measures were change in visual acuity, and occurrence of postoperative complications with minimum follow-up of a year.
The investigators identified 63 eyes of 60 patients. Thirty-three eyes underwent combined PPV and ACIOL placement, while and 30 eyes underwent combined PPV and scleral fixation of a PCIOL using a Gore-Tex suture. Mean follow-up was 502 ±165 days (median: 450, range: 365 to 1,095 days).
In the ACIOL group, mean visual acuity improved from 20/914 preoperatively to 20/50 postoperatively (p<0.001). In the scleral-fixated PCIOL group, mean visual acuity improved from 20/677 preoperatively to 20/46 postoperatively (p<0.001). No difference in visual acuity was noted between groups at one year (p=0.91) or at the final follow-up (p=0.62).
In terms of complications, eyes undergoing ACIOL placement had a significantly higher rate of transient corneal edema (30.3 vs. 6.7 percent, p=0.02) compared with eyes undergoing scleral fixation of a PCIOL.
In light of the results, the surgeons say that both modalities resulted in similar visual outcomes.
Retina 2019;39:5:860-868.
Khan MA, Gupta OP, Pendi K, et al.
Acanthamoeba Co-infection More Common than Expected
Researchers from the Aravind Eye Hospital and Post-graduate Institute of Ophthalmology in Coimbatore, India say that Acanthamoeba co-infection appears to be more often associated with microbial keratitis than some might think.
In this prospective cross-sectional study, patients presenting with stromal keratitis were additionally tested for Acanthamoeba, regardless of the clinical diagnosis. The investigators used culture positivity as the gold standard.
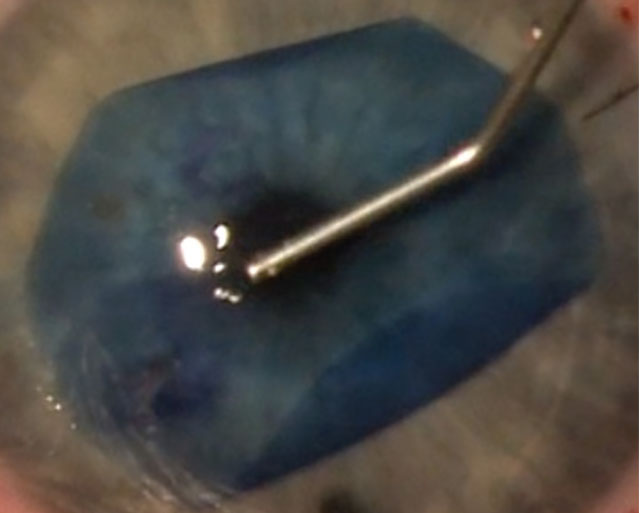
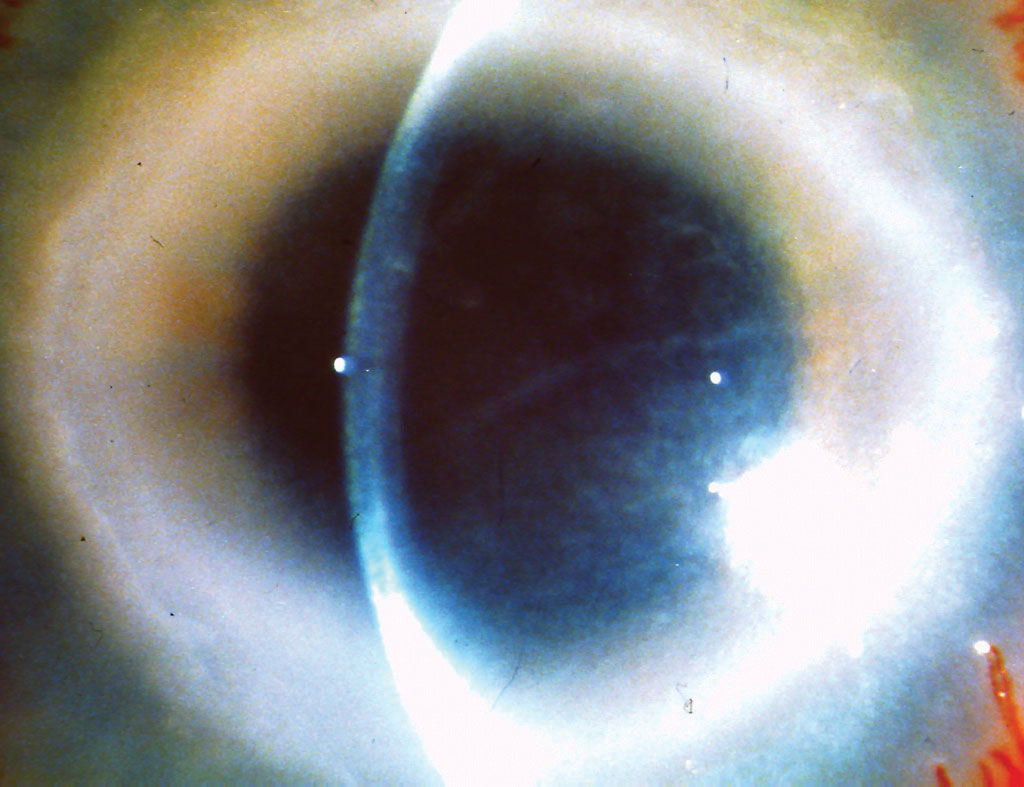 |
|
|
Of the 401 cases included in the study, 40 were positive for Acanth-amoeba (10 percent); of these 40, 16 were positive for both Acanthamoeba and fungi (4.5 percent of the study group was Acanthamoeba- and fungal keratitis-positive); five (1.2 percent) were positive for Acanthamoeba and bacteria; and two (0.5 percent) had a triple infection with Acanthamoeba, fungi and bacteria.
The physicians say that ring infiltrates and stromal edema are frequently associated with Acanthamoeba keratitis, as well as Acanthamoeba coinfections. Ring infiltrates in particular were more frequently seen in the Acanthamoeba and fungal keratitis group (8/16) and they were often yellowish with hyphate edges (vs. ring infiltrates only, which are seen in the patients with Acanthamoeba alone). Only two patients were contact lens wearers: however, they presented with history of trauma.
The researchers say that the results appear to show that Acanthamoeba infections are much more frequent than most think, and aren’t just restricted to contact lens wearers. They add that anticipating coinfections is necessary for establishing a diagnosis, as well as a proper therapy.
Am J Ophthalmol 2019;201:31-36.
Raghavan A, Baidwal S, Venkatapathy N, Rammohan R
Retinal Characteristics in Eyes With Early AMD
Researchers assessed the features of the retinal pigment epithelium in eyes with early age-related macular degeneration and subretinal drusenoid deposits using optical coherence tomography.
They classified the eyes into three types: nonundulating RPE; undulating RPE; and wedge-shaped RPE. They compared the retinal vessel densities, retinal thickness and choroidal thickness of a 3-mm-diameter zone. Their findings included the following:
• A total of 33 eyes were classified as having nonundulating RPE; 27 eyes were classified as having undulating RPE; and 20 eyes were identified as having wedge-shaped RPE.
• The vascular densities of the superficial and deep capillary plexuses showed differences: nonundulating RPE group 23.93 ±2.26 percent and 23.54 ±1.78 percent; undulating RPE group 22.29 ±2.80 percent and 21.94 ±2.42 percent; and wedge-shaped RPE group 21.93 ±2.7 percent and 20.63 ±2.42 percent (p=0.010 and p<0.001).
• Mean retinal thicknesses and choroidal thicknesses were also different. The respective findings were: nonundulating RPE group, (298.26 ±13.81 µm and 180.08 ±55.49 µm); undulating RPE group, (285.29 ±21.88 µm and 148.45 ±55.08 µm); and wedge-shaped RPE group, (274.86 ±20.62 µm and 135.75 ±39.77 µm) (p=0.001 and p=0.007).
Researchers reported that altered features of the RPE on optical coherence tomography might indicate advancement in disease and be part of an overall degenerative process in these eyes.
Retina 2019; Apr 2. [Epub ahead of print].
Jang S, Park SY, Ahn SM, et al.
Beta Blockers and AMD Progression
Researchers from the University of Pennsylvania’s Scheie Eye Institute say surgeons and their patients probably don’t need to worry about the risk of progression to wet age-related macular degeneration if the patients are using beta blockers.
In a retrospective cohort study of patients from 2000 to 2014, using data from a large national U.S. insurer’s claims database, researchers identified 18,754 beta blocker patients and 12,784 calcium channel blocker patients who met the criteria for inclusion.
After controlling for covariates, patients on beta blockers were at lower risk for neovascular AMD at both 90 and 180 days than patients on calcium channel blockers (HRs: 0.67-0.71; p<0.01 for both) or diuretics (HRs: 0.55-0.62; p<0.01). Patients on beta blockers, versus angiotensin-converting enzyme/angiotensin receptor blocker at all time points, and beta blockers versus calcium channel blockers and diuretics at 365 days, didn’t have a significantly lower association with neovascular AMD (HR: 0.73-0.85; p>0.06 for all).
A sensitivity analysis yielded similar results, with patients on beta blockers significantly less likely to develop wet AMD at 90 and 180 days (HR: 0.70-0.76; p<0.049 for both) but not at 365 days (HR: 0.88; p=0.30) compared with patients on calcium channel blockers.
Ultimately, the researchers say there was no evidence that beta blocker use increased the risk of wet AMD vs. other antihypertensive meds. REVIEW