Researchers used Mendelian randomization (MR) analysis to determine genetic causal associations between myopia, glaucoma and glaucoma-related traits to overcome the effects of external confounders.
The study doctors analyzed bi-directional genetic associations between myopia or refractive spherical equivalent (RSE), POAG and POAG-endophenotypes. They analyzed data from a genetic bank (n=216,257 to 542,934), and used multiple Mendelian randomization models and multivariate genomic structural modeling to identify significant mediators for the relationship between myopia and POAG.
Here are some of the findings:
- Researchers found consistent bi-directional genetic associations between myopia and POAG, and between myopia and intraocular pressure using multiple MR models at Bonferroni-corrected levels of significance.
- IOP had the most significant mediation effect on RSE and POAG (Sobel test: 0.13; CI, 0.09 to 0.17; p=1.37×10-8).
Researchers found a strong bi-directional genetic causal link between myopia and POAG, which was mainly mediated by IOP. The findings suggested IOP-lowering treatment for glaucoma may be beneficial in myopic eyes, despite the challenges of establishing a clear clinical diagnosis, they added.
Ophthalmology 2022; Dec 6. [Epub ahead of print]
Chong RS, Li H, Cheong AJ, et al.
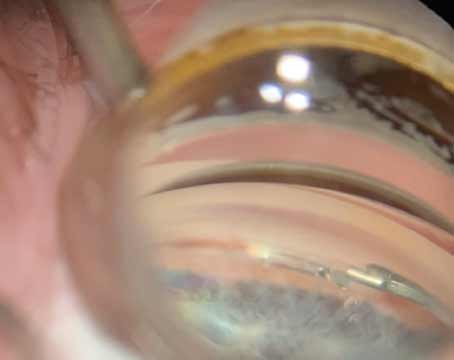
Changes after Aflibercept Treat and Extend
Investigators examined the morphological changes in macular neovascularization secondary to age-related macular degeneration after two years of aflibercept treatment under a treat-and-extend regimen.
This retrospective study analyzed the medical records for 26 eyes of 25 patients diagnosed with treatment-naïve neovascular AMD and treated with aflibercept under a T&E regimen for two years. The areas of the MNV and vascular structures were assessed using swept-source optical coherence tomography angiography at baseline and after two years of treatment.
Here are some of the findings:
- The mean MNV area increased significantly from 0.65 ±0.42 mm2 at baseline to 0.78 ±0.45 mm2 at two years.
- At two years, the mean change in the MNV area from baseline was 22 percent (interquartile range: 4 to 60 percent).
- The baseline MNV area was negatively correlated with the change ratio of the MNV areas at two years and baseline (R=-0.68; p<0.001).
- Nine of 26 eyes (34.6 percent) showed newly formed mature vessels, and seven eyes (26.9 percent) showed prominently developing preexisting mature vessels.
Investigators determined MNV expanded and showed vascular maturation under aflibercept treatment with a T&E regimen. They added, the smaller the MNV at baseline, the greater was its expansion in two years.
Retina 2022; Nov 17. [Epub ahead of print].
Nakano Y, Takeuchi J, Horiguchi E, et al.
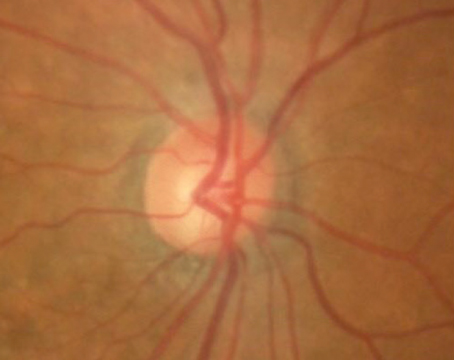
Detecting Optic Disc Drusen
Researchers evaluated the most accurate diagnostic imaging modality to detect optic disc drusen (ODD) between B-scan ultrasonography (U/S), fundus photography, fundus autofluorescence (FAF) and enhanced depth imaging optical coherence tomography (EDI-OCT).
The comparative diagnostic analysis included 205 eyes of 105 patients with suspected ODD. Of these, 108 had ODD. All eyes received a full in-person ophthalmic exam with 3D view of the optic nerve and all four imaging modalities.
Here are some of the findings:
- EDI-OCT had the highest sensitivity (95 percent) and accuracy (97 percent) to detect ODD, compared to:
— FAF (sensitivity, 84 percent; accuracy, 92 percent);
— U/S (sensitivity, 74 percent; accuracy, 86 percent); and
— fundus photography (sensitivity, 38 percent; accuracy, 66 percent).
- All image modalities had high specificity (>97 percent) and precision (>93 percent).
- Enhanced depth-imaging OCT had the highest examiner confidence (96 percent) compared to the others (88 percent).
Researchers determined that, among the four imaging modalities, enhanced depth-imaging OCT had the highest diagnostic utility for the detection of optic disc drusen and suggested it should be considered the preferred initial diagnostic modality.
Am J Ophthalmol 2022; Dec 11. [Epub ahead of print]
Youn S, MFE B, Armstrong JJ, et al.