The most commonly used method of applying mitomycin-C during glaucoma surgery is to soak a Weck-Cel sponge in a solution of the drug and then apply the sponge to the ocular tissues for a few minutes. However, many surgeons, including those in our practice, use a different approach; we inject the mitomycin-C directly into the conjunctival tissue. Our surgical results have been just as good since switching to this method, and it appears to have some potentially significant advantages over the sponge method. Here, I’ll discuss the benefits and limitations of each technique.
Injecting Mitomycin-C
Although a number of surgeons have injected mitomycin-C for many years, it has not yet achieved wide acceptance. This undoubtedly reflects the fact that it hasn’t been well-studied or discussed in the literature (many surgeons aren’t even aware that it is an option). Of course, surgeons understand that mitomycin-C has
potential downsides, so it’s not surprising that even those who are aware of this approach would be cautious when considering a new method of delivery.
To help clarify the reasons for considering this approach, I’d like to begin by describing how we use this technique in our practice. First of all, in order to inject mitomycin-C in trabeculectomy surgery safely, it is important to pay attention to your dosages. The dose we use is more dilute than that used when applying mitomycin-C with the sponge method. With a sponge, surgeons generally use 0.1 mg/ml to 0.4 mg/ml of mitomycin-C, but when injecting it, a lower concentration of 0.05 to 0.1 mg/ml is used because of the direct injection into Tenon’s layer.
|
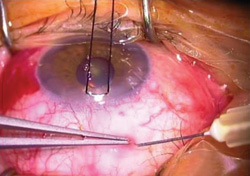
Once the solution is prepared, it is drawn up into a 1-cc syringe with a 30-ga. needle. We start the surgery by placing a traction suture in the cornea; then we inject approximately 0.1 ml total volume into the Tenon’s layer, about 8 to 9 mm posterior to the limbus and a little off to the side to avoid the superior rectus muscle. The injection of fluid raises a little blister at the injection site. We irrigate the conjunctiva with balanced saline solution and then take a muscle hook and gently spread the injected bolus of mitomycin-C around the superior conjunctiva and Tenon’s layer. The fluid remains contained within the tissue as we spread it. Then we make our first incision and proceed with the surgery the way we normally would. (You can watch a video of our technique on YouTube at: youtube.com/watch?v=LxmHd136FOs.)
It’s worth noting that some surgeons choose to inject the mitomycin-C prior to entering the operating room, when the patients are in the preoperative holding area. Toronto surgeon Ike Ahmed, MD, has posted videos on Eyenet demonstrating this approach. In our practice, however, we do it all in one step in the operating room at the beginning of surgery.
Another debate concerns whether it is necessary to irrigate the eye following the injection. Many surgeons don’t believe it is. My feeling is that even with an injection, it is quite possible that some mitomycin-C seeps out from the tissue. I therefore irrigate to ensure that any remaining unbound medication doesn’t remain on the ocular tissues. However, omitting this step has not appeared to result in a higher complication rate for my colleagues.
The Pros and Cons of Injecting
There are a number of advantages to injecting the mitomycin-C rather than applying it with a sponge:
• It takes less time. On average, surgeons leave the mitomycin-C sponge sitting on the eye for three minutes or so. (Some leave it longer.) Although three minutes doesn’t sound like much, when you’re trying to be efficient, sitting in the OR for three minutes with nothing else to do is like watching a pot of water boil—it feels like an eternity. You don’t spend that time waiting if you inject the mitomycin-C.
• You’re not dealing with sponges. Reports of losing mitomycin-C sponge fragments have appeared in the literature.1 Sometimes a piece of a sponge breaks off and the surgeon doesn’t realize it is still inside the eye, which can result in infection and necrosis. If you inject the mitomycin, this is not an issue.
• You know exactly how much mitomycin-C was delivered to the eye. You’re injecting a known dose and volume, so you can calculate the exact amount of drug that is delivered to the eye. This can be a big advantage, especially for research purposes. When you soak a sponge in fluid and leave it on the eye, you really don’t know how much drug you’re delivering.
• The mitomycin-C can be spread as diffusely as you wish. When you apply mitomycin-C, the hope is that you will end up with a final bleb morphology that is very low-profile and diffuse—not focal, thin, avascular and cystic. The latter type of bleb is prone to leakage and infection. Peng T. Khaw, MD, PhD, at Moorfields Eye Hospital, promotes a fornix-based conjunctival incision that allows for the diffuse application of mitomycin-C sponges.2 He believes that this methodology results in a lower profile, diffuse bleb. Likewise, with the injection technique, there’s no border or restriction as to how diffusely you can spread the mitomycin-C.
• Outcomes may improve. Perhaps the most compelling reason to consider switching to injecting mitomycin-C is that early data suggests it may have a positive effect on surgical outcomes. So far, no one has conducted a prospective, randomized study comparing sponge application of mitomycin-C to injection, but our group was able to conduct a retrospective study of both techniques. We presented some of the results of that study at the 2013 meeting of the American Glaucoma Society and are currently preparing to submit the data for publication.
In our study we looked at patients who had received a trabeculectomy with mitomycin-C at the University of California, Davis. Fifty-seven eyes were treated with sponges; 126 received mitomycin-C delivered by injection. We assessed IOP reduction, IOP success rates, medication use and complication rates at one month and at one to three years after the initial surgery. The data indicated that the two groups were statistically similar in most respects, including visual outcomes. However, several findings were noteworthy:
— Despite our finding of no significant difference in the amount of pressure reduction between the groups, at 36 months the injection group was taking significantly fewer glaucoma medications than the sponge group.
— When we looked at procedures performed within a month after trabeculectomy surgery we found that the number of postop 5FU injections was significantly lower in the mitomycin-C injection group than in the sponge group.
— When we looked at complications occurring more than a month after surgery, we found a significantly higher rate of tense, vascularized or encapsulated blebs (signs of excessive scarring) in the mitomycin-C sponge group (7 percent vs. 0 percent in the injection group).
• It doesn’t appear to harm the tissue. We didn’t find any postoperative differences between the groups in terms of complications such as choroidal effusion, hypotony, bleb leak or overfiltration. This is noteworthy, since one may worry that injecting the mitomycin-C will result in overtreatment, thus injuring or destroying conjunctival and Tenon’s tissues. However, if that were the case, these complications would be more frequent in the injection group.
These results are encouraging, but of course these data are retrospective and should be interpreted with caution. Nevertheless, the differences we found indicate that this alternative technique might turn out to offer advantages over the sponge technique. At the very least, it is worthy of further study and a randomized, controlled, clinical trial is indicated.
In terms of downsides, there is always some danger of perforating the eye during the injection if the patient were to suddenly move, although we’ve never had anything like that occur.
A Promising Alternative
One thing about this technique that surgeons seem to appreciate is that it is very easy to do; it is not like learning a more complex procedure such as canaloplasty. Injecting mitomycin-C is a technique that anyone can do, since it is identical to giving subconjunctival injections of antibiotics or corticosteroids at the end of a surgical case.
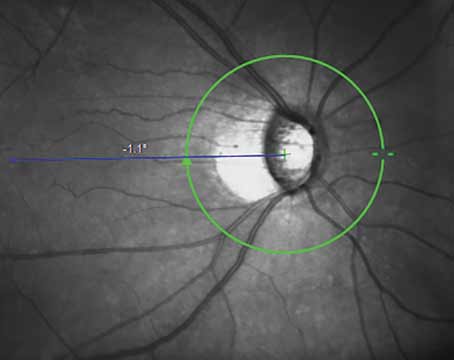
One key question that our study did not answer is whether the injection technique actually produces better bleb morphology. A prospective, randomized study of this technique versus sponge application of mitomycin-C, employing a bleb grading scheme such as the Indiana Bleb Grading Scale,3 would help to answer this question. REVIEW
Dr. Lim is a professor of ophthalmology and vice chair and medical director of the University of California, Davis Health System Eye Center in Sacramento. She has no financial ties to any products mentioned.
1. Shin DH, Tsai CS, Krupin TH, Olivier MM. Retained cellulose sponge after trabeculectomy with adjunctive subconjunctival mitomycin-C. Am J Ophthalmol 1994;118:1:111-112.
2. Wells AP, Cordeiro MF, Bunce C, Khaw PT. Cystic bleb formation and related complications in limbus- versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin-C. Ophthalmology 2003;110:11:2192-7.
3. Cantor LB, Mantravadi A, WuDunn D, Swamynathan K, Cortes A. Morphologic classification of filtering blebs after glaucoma filtration surgery: The Indiana Bleb Appearance Grading Scale. J Glaucoma 2003;12:3:266-271.