Glaucoma patients more frequently report high costs as a reason for nonadherence to medication compared with non-glaucoma patients.1 Often, this is in addition to other issues that impact compliance such as medication tolerance, side effects and health literacy. I see these concerns in my clinic all the time. Patients ask, “How much will this treatment cost me? Is it affordable?”
As glaucoma specialists, we must be cognizant of the financial burden patients face and how this affects their ability to adhere to treatment. Though topical medications are considered a mainstay of glaucoma management, and we’re fortunate to have an array of these effective therapies to choose from, they’re not necessarily simple options for patients. Here, I’ll discuss some strategies for tackling the cost burden of medications so patients can remain compliant.
The Consequences of Nonadherence
Medication adherence among the nearly 3 million Americans with glaucoma has been reported to be as low as 20 percent.2 Barriers to adherence include affordability, treatment complexity and lack of disease knowledge, as well as self-reported barriers such as self-efficacy, forgetfulness, fear of side effects and dosing ability.2
Unfortunately, medication adherence less than 80 percent has been associated with worsening visual field defect severity.3 A study of 6,343 patients in the Kaiser Permanente Southern California health system reported a 73-percent average treatment adherence, with a significantly reduced mean deviation progression of 0.006 dB per year for each 10-percent absolute increase in adherence, after controlling for confounders and the interaction between time and baseline disease severity. The model used in the study estimated time to glaucoma progression (as a -3 dB-change in mean deviation from baseline) was 8.3 and 9.3 years for patients with 20-percent and 80-percent adherence levels, respectively.4
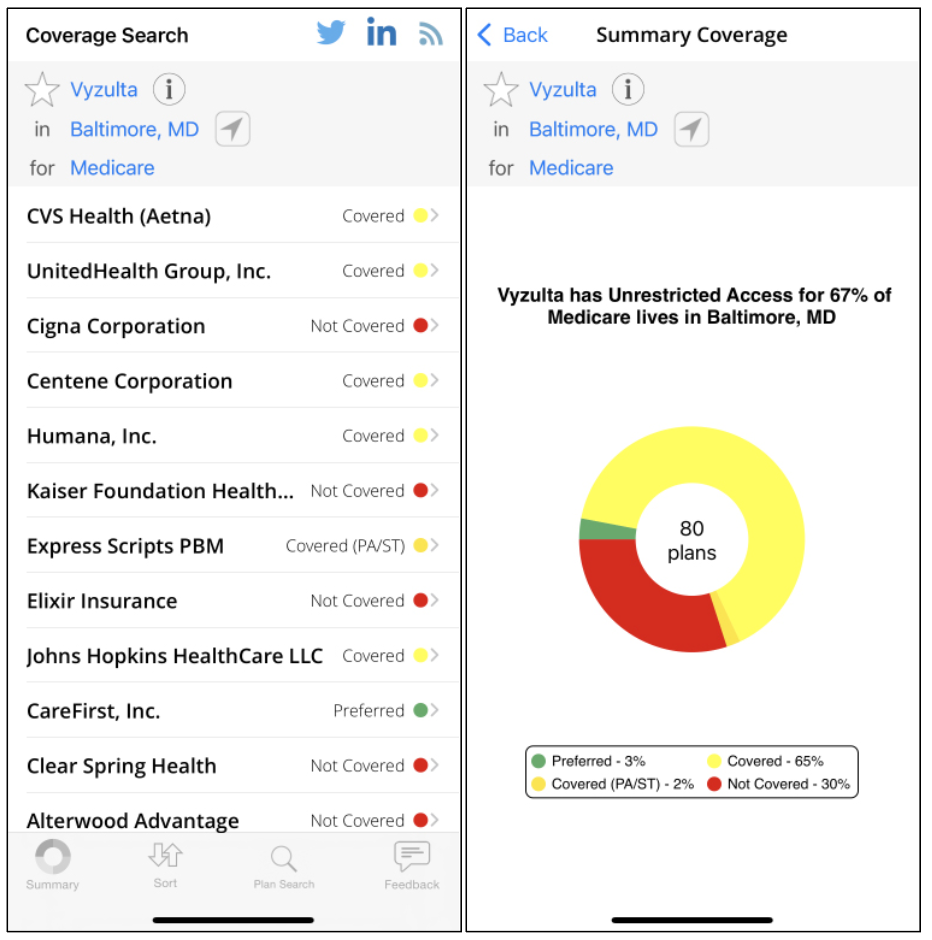 Figure 1. In Coverage, I can see Vyzulta is covered by the vast majority of Medicare plans, but about 30 percent of plans don’t cover it. These are OK odds, so I know there’s a good chance it’ll be covered. However, if a certain medication had a lower chance of being covered by Medicare, say 5 percent, it may not be the first medication I choose for a patient. |
Cost-saving Strategies
Medication costs present a significant burden to patients and the problem of affordability can have devastating consequences. We’ve seen a 59-percent increase in the price of brand-name glaucoma medications in the United States between 2013 and 2019.5
Here are some strategies you can consider to help your patients deal with drug costs:
• Generics. Using generic medications as first-line treatments is a common approach to the problem of affordability. Though brand-name drug prices have been increasing, the same study reported that generic medication prices dropped by 22 percent between 2013 and 2019.5 Oftentimes, insurance companies will require that a generic be trialed before you can switch the patient to non-generics or brand-name medications. Recent additions to the generics marketplace include travoprost and brinzolamide.
Patients may have questions about the efficacy of generics versus brand-name medications. In the United States, generic medications are required to have the same active ingredients as the brand-name medication and should work in the same way.6 Numerous studies have demonstrated similar efficacy, but generics may vary in their side effect profile, so it’s important to discuss all options with the patient. For patients with significant side effects and inadequate IOP control, brand-name medications may be preferred.
• Combination drops. Combination drops can reduce the burden on patients with regard to purchasing and remembering to take multiple different drops. In addition to fixed dose combination medications such as Cosopt (dorzolamide-timolol) or Combigan (brimonidine-timolol), compounding pharmacies such as SimpleDrops/ImprimisRx, offer various combinations of medications at a fixed cost that’s often affordable even to those individuals without adequate insurance coverage.
Though this option may simplify the patient’s regimen and lower costs, one caveat is that many of these combination medications haven’t been studied to determine whether their combined efficacy is just as good as taking each medication individually.
• Mail-order pharmacies. The cost of a generic medication on the same insurance plan may be very different if a patient were to pick it up at a point-of-care pharmacy versus if it were delivered by mail, especially if you prescribe a 90-day mail-order supply. This may also aid compliance since the patient receives a three-month supply directly to their home instead of having to go to the pharmacy each month to pick up medicine.
• Copay assistance. If the patient has commercial insurance, many of the larger pharmaceutical companies provide copay assistance cards or manufacturer coupons, which act as discounts to reduce the actual cost the patient pays out of pocket. These options are typically available only for brand-name medications.
Copay assistance isn’t limited to glaucoma drops. Many companies also provide copay assistance for steroids and antibiotics, so if a glaucoma patient requires postop medications, copay assistance may be an option as well.
• Prescription discount cards. Prescription discount cards from companies such as GoodRx, SingleCare, Optum Perks, RxSaver and ScriptSave WellRx are available for anyone to use, regardless of insurance status. (For those with insurance, the out-of-pocket costs won’t go toward the deductible.)7 These companies negotiate bulk purchases with pharmacies and pass the savings on to customers through the discount card programs.
• Preservative-free drops. Medication intolerance is another commonly cited barrier to adherence. The same medications are often available in preservative-free form, and many of these preservative-free medications are now generic, such as PF dorzolamide timolol. Other medications, even if they aren’t preservative-free—such as Travatan Z, Xelpros or Alphagan P, have gentler preservatives or preservatives that break down faster at the tear film. These drugs are often better tolerated and are good options to consider for patient tolerability and increased compliance.
• Administration aids. Pricey glaucoma medications also come in tiny bottles. Some patients, because of their medical conditions or an inability to get the drop directly into the eye, may be wasting one or more drops each time they attempt to instill their medications. Using a device like the Nanodropper reduces the medication dose from a standard 30 to 50 µl to a 10-µl drop. This nanodrop still provides the same efficacy in terms of IOP-lowering, but it potentially allows the patient to stretch their bottle of medication a little longer and reduce local and systemic side effects from the medication as well.
 |
|
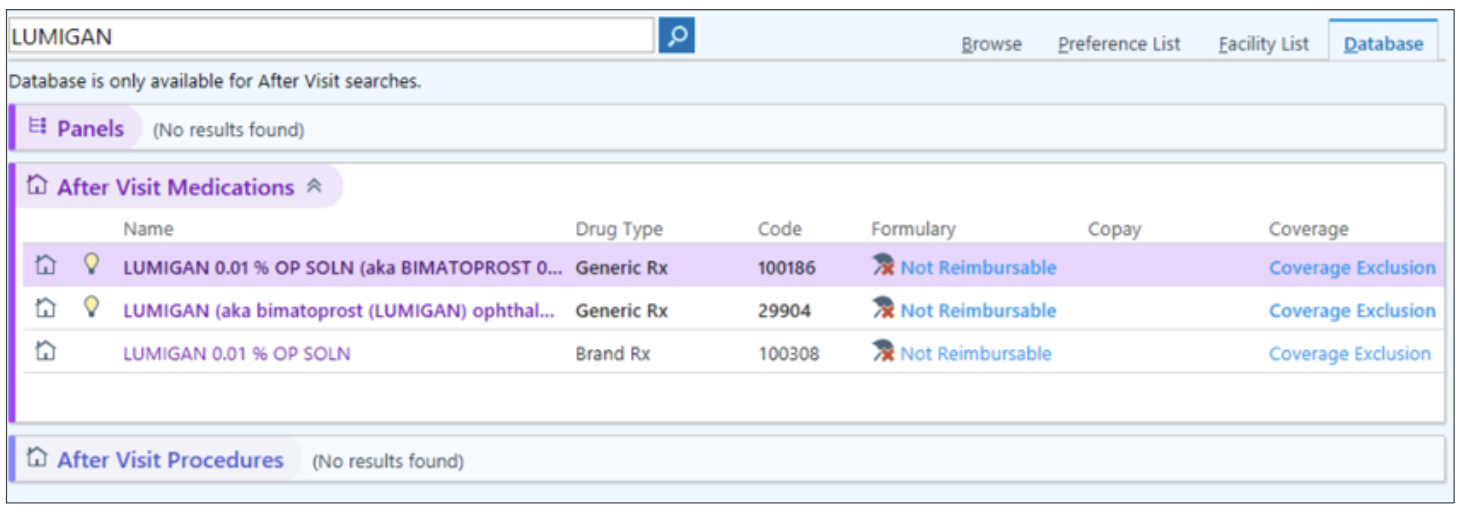
Figure 2. Epic displays at-a-glance insurance coverage for various medications. This information is good to consider for patients who are concerned about drug prices. |
Harness Technology
Smartphone apps can give you an idea of what a patient may pay out-of-pocket for a glaucoma medication. They’re easy to download and readily accessible. I’ve used an app called Coverage, which searches coverage for a particular medicine in a city or zip code for a given commercial insurance or for Medicare. This enables the prescribing provider to get a sense of the lay of the land (Figure 1).
Electronic medical records often house your patient’s insurance and pharmacy information in their systems, which can also give you an idea of how much a patient may have to pay or at least provide a starting point to counsel the patient.
I currently use Epic at my university practice and EMA (Modernizing Medicine) at one of my satellite offices. In Figure 2, if I were to prescribe Lumigan—a brand-name prostaglandin analog—Epic tells me that for this particular patient’s insurance, the drug is non-reimbursable under the different formularies it exists under. When I counsel the patient, I may say, “I believe this is the right medication for you, but it might be more expensive, or your insurance may initially deny it.” This gives the patient a heads-up that they might encounter some issues when obtaining the medicine.
Though the EMR may say a certain medication is non-reimbursable, that doesn’t necessarily mean the insurance won’t pay for it eventually. A prior authorization may be necessary (more on that below). That said, this tool lets me know there may be some hoops to jump through if I were to prescribe that medication, versus if it had said the medication was “preferred.”
Some EMRs will show non-insurance-based coupons that are available to the patient. In Figure 3, if I were to prescribe Lumigan for the same patient, EMA brings up the active insurance plan and says that if the patient were to use a coupon from GoodRx and pick up their prescription from a Walgreens near them, the cost would be approximately $33.
There are limits to these technologies though. Insurance plans are complex—there might be 50 different plans a patient could participate in within Blue Cross. One might be a PPO where there’s no issue about coverage and the patient pays a standard copay. Another patient might be on a high-deductible plan where they’re on the hook for 100 percent of the cost until they meet their deductible. It’s hard for a provider or the EMR to tease out some of these details, especially considering that a patient’s deductible isn’t limited to ophthalmology but encompasses their entire health-care utilization.
Taking the time to search out medication coverage for drugs you’re less familiar with may also take a few extra minutes of chair time. Additionally, there could be extra time needed after the clinic visit if the patient calls back and says they can’t afford their medicine and need an alternative. While these tools aren’t always accurate, they can give you a rough idea. In the past, this type of cost-estimate was a “black box” of sorts. Being able to offer patients this information is particularly beneficial for many older patients and others who are on a fixed income.
Prior Authorization
As I mentioned, even if a medication isn’t preferred by insurance, it may eventually be covered with prior authorization—and that presents another barrier. A 2016 American Medical Association survey found that prior authorization could delay care more than 90 percent of the time and each prior authorization could cost the practice or physician’s office an extra $100 in indirect costs, whether that’s time a technician spends away from their regular duties, paperwork or other associated costs.8 Studies have shown that the vast majority of prior authorizations are approved, making this process an onerous burden.
What can glaucoma specialists and their staff do?
• Designate a staff member. Having a dedicated staff member to deal with prior authorization for the practice the majority of the time can help. Learning the language of what to say in prior authorization requests, knowing what numbers to call and what paperwork to fill out will streamline operations instead of having a new person learn to tackle this each time.
• Have a dedicated phone line. Nobody enjoys phone tag. Having a single phone number that pharmacies or insurance companies can use to call back will make this process smoother.
• Consider outsourcing. Many online pharmacies will manage or provide support for prior authorizations, figure out whether the patient may qualify for additional financial assistance, coordinate medication delivery and check in with the patient about issues such as side effects, questions and refill scheduling. I’ve used a Baltimore-based online pharmacy called Medly to relieve some of my clinic’s prior authorization burden. The Philadelphia-based Capsule Pharmacy is another. Amazon and Cost Plus drugs aim to be bigger players in the low-cost marketplace as well.
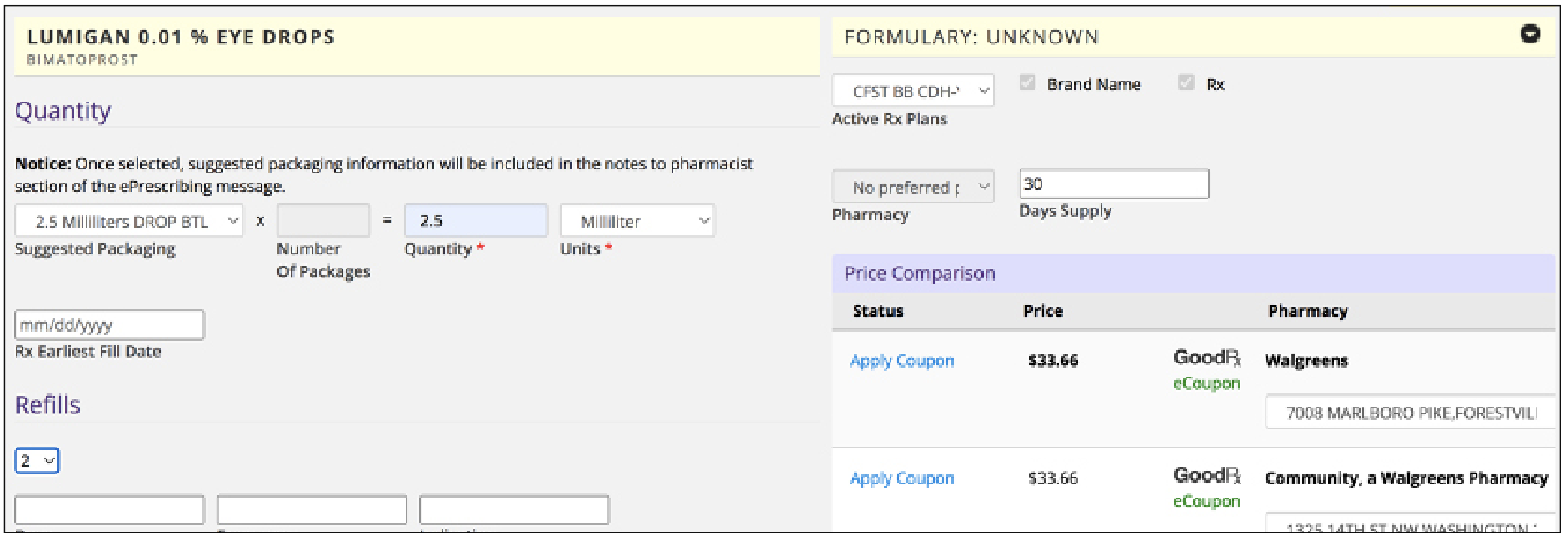 Figure 3. Other EMRs such as Modernizing Medicine’s EMA display coupons or cost-saving programs patients can use to obtain their medications for a lower price. |
Talk to Patients About SLT
Selective laser trabeculoplasty is a good alternative to topical medication for those with stable disease who experience ocular surface irritation from preserved drops or those who are unable to use drops due to cost. Early intervention with laser can reduce the number of topical drops patients eventually need to go on as well. I have long offered this as a first line treatment to many of my patients but some may be resistant to the idea of a laser treatment. Here are some pearls for introducing SLT to patients in a way that puts them at ease:
• Mention SLT’s long track record. I start off by telling patients that there’s a great treatment that’s been around for decades. This helps them understand that SLT isn’t new or experimental.
• Point out that it’s a covered procedure. Cost is often the next question patients have. This treatment is covered by insurance when medically necessary to treat their glaucoma, such as when topical medications are intolerable, or the patient isn’t able to use topical medications.
• Choose your words carefully. While conveying accurate information, try to use words such as “laser” and “surgery” sparingly when discussing SLT because those words tend to be jarring to patients. Instead, point out that the treatment is minor, non-invasive and is done in the clinic. I often say, “It’s light energy that’s delivered in a non-invasive way to encourage the eye’s natural drain to function better.” This helps patients understand that SLT helps to reset what their eye is meant to do. This seems to de-escalate fears and negative associations patients may have with lasers.
• Emphasize the published outcomes. Explaining the results of the LiGHT study in a way that’s understandable to the patient may also help assuage fears. I tell patients that the data shows this is a great treatment, especially when done early as first-line, and tends to treat glaucoma better in the long term.
• Keep the options open. If patients are still reluctant, I give them a break and let them know that if they want to think about it or aren’t ready to decide yet, we can try medications. I still bring up SLT frequently at future follow-up visits, so they know it’s still an option for them. Oftentimes, those who were initially reluctant will begin topical drops and see the issues that come with medication—side effects and tolerability, cost, adherence issues—and return six or eight months later saying they’d like to give laser a try.
While not everyone will be convinced about SLT, particularly older patients who are used to taking multiple medications, a combination of these pearls—highlighting the benefits and low risk profile—can lessen patients’ fears while still accurately conveying information.
In summary, there are many ways we can help patients navigate glaucoma medication costs, from switching to generics when appropriate and counseling patients about potential out-of-pocket expenses and available savings programs to recommending SLT. Though affordability is only one aspect affecting medication compliance, it’s a major hurdle for many. We can contribute to improved adherence by taking steps to discuss costs and find solutions with patients.
Dr. Singh is a professor of ophthalmology and chief of the Glaucoma Division at Stanford University School of Medicine. Dr. Netland is Vernah Scott Moyston Professor and Chair at the University of Virginia in Charlottesville.
Dr. Swamy is an associate professor of ophthalmology and visual sciences and the director of the Ophthalmology Residency Program at the University of Maryland School of Medicine. She has no relevant financial disclosures.
1. Gupta D, Ehrlich RJ, Newman-Casey PA, et al. Cost-related medication nonadherence in a nationally representative US population with self-reported glaucoma. Ophthalmol Glaucoma 2021;4:2:126-130.
2. Gatwood J, Brooks C, Meacham R, et al. Facilitators and barriers to glaucoma medication adherence. J Glaucoma 2022;31:1:31-36.
3. Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology 2011;118:2398–2402.
4. Shu Y, Wu J, Luong T, et al. Topical medication adherence and visual field progression in open-angle glaucoma: Analysis of a large US health care system. J Glaucoma 2021;30:12:1047-1055.
5. Barayev E, Geffen N, Nahum Y, et al. Changes in prices and eye-care providers prescribing patterns of glaucoma medications in the United States between 2013 and 2019. J Glaucoma 2021;30:3:e83-e89.
6. Generic drug facts. FDA. https://www.fda.gov/drugs/generic-drugs/generic-drug-facts. Accessed January 5, 2023.
7. 2020 Update: Things to know about prescription discount cards. Scriptdrop. https://scriptdrop.co/2020/07/15/things-to-know-about-prescription-discount-cards/. Accessed January 6, 2023.
8. Patient clinical outcomes shortchanged by prior authorization. American Medical Association 2018. https://www.ama-assn.org/press-center/press-releases/survey-patient-clinical-outcomes-shortchanged-prior-authorization. Accessed January 6, 2023.



