Ever since it first appeared, optical coherence tomography has been evolving. In particular, the scanning speed of commercially available OCT units has steadily increased, allowing the technology to be used for an ever-longer list of clinical tasks. (Faster scanning rates means more sampliing and denser data per volume scanned.)
Anterior segment OCT has been feasible for a number of years, but it’s been slow to achieve widespread use in the United States. Here, surgeons discuss its advantages, how it compares to other technologies used for this purpose, and why they believe it’s taking a while to become popular. In addition, they offer some pearls for surgeons who are adding this to their list of clinical tools.
The Advantages of AS-OCT
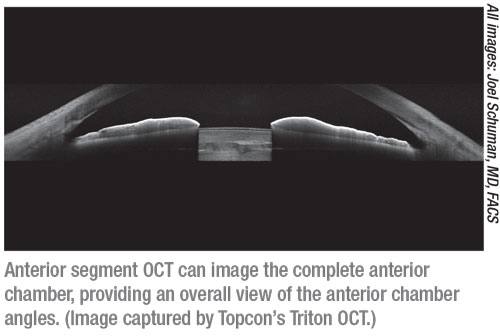
“Anterior segment OCT can measure almost anything in the front part of the eye,” says Joel S. Schuman, MD, FACS, Elaine Langone Professor and vice chairman for research in the department of ophthalmology, and professor of neuroscience and physiology, at NYU Langone Health, NYU Grossman School of Medicine, in New York City. “Depending on the wavelength, you may or may not be able to see deep into the angle or behind the iris, but you can see the various corneal layers in high detail, and there are ways of looking at the cornea’s anterior and posterior curvature. For that reason, this technology should have great value for an anterior segment surgeon, especially in cases of corneal pathology, or as a pre- or postoperative tool when performing various types of corneal surgery that involve the endothelium or Descemet’s membrane.
 |
“Some OCT instruments [outside the United States] are able to get a 360-degree view of the anterior segment, and some can give you essentially a video of the angle, as if you’re sitting inside the eye looking at it,” he continues. “If you’re interested in looking at the palisades of Vogt, you can see that with anterior segment-OCT; in fact, our group recently received a patent for using anterior segment OCT to evaluate the stem cell niche. (We think that area will be important going forward, in terms of making clinical decisions regarding a patient’s stem cell capacity, which will have implications for corneal transplants and other procedures.) When managing keratoconus you can look at the tissue thickness and confirm the corneal structure, especially in the area of the cone. And of course, one of the great powers of OCT is measuring the axial length.”
David Huang, MD, PhD, the Peterson Professor of Ophthalmology, and a professor of biomedical engineering at Oregon Health & Science University in Portland, notes that an important advantage of OCT is that it has excellent resolution compared to ultrasound or Scheimpflug imaging. “For example, it can measure the thickness of the epithelium—in some systems also the endothelium—which would be beyond the capability of other technologies,” he says. “It also has a wide field of view; some systems can scan a 20-mm area. Confocal microscopy, in comparison, has a very narrow view and requires contact with the eye. I think it’s in a sweet spot in terms of resolution and field of view.”
Vikas Chopra, MD, medical director of the Doheny Eye Centers Pasadena, and an associate professor of ophthalmology at the David Geffen School of Medicine at UCLA, notes other advantages. “Anterior segment OCT is non-contact, which is even more important now due to the COVID-19 crisis limiting contact with the patient,” he explains. “It can be done with standardized lighting conditions, including complete darkness, and it provides precise measurements that have been shown to have excellent reproducibility and repeatability. In contrast, a procedure like gonioscopy requires contact with the patient’s eye, hands-on-training to learn—and sometimes years of practice to master—and it provides subjective measurements. It also requires some light to visualize the angle.”
Drs. Chopra and Huang note the pros and cons of AS-OCT compared to ultrasound biomicroscopy. “UBM is harder to use because it requires eye contact, it’s messy and it’s not as good at measuring shape,” Dr. Huang points out. “I think UBM should be limited to situations where you really need penetration, such as when you want to look through a uveal or iris tumor or evaluate a ciliary body problem. Some biometry measurements, like sulcus-to-sulcus width, need that kind of penetration. But I think OCT will be used a lot more because it’s non-contact and it’s versatile. There’s more justification for buying one.”
“UBM allows visualization of the ciliary body and structures posterior to the iris, which anterior segment OCT typically hasn’t been able to image well,” notes Dr. Chopra. “However, this is now changing. The Heidelberg Anterion can provide stunning 360-degree anterior segment images, along with good imaging of the ciliary body.” Dr. Chopra says that he and his colleagues presented a poster at the recent virtual AAO meeting showing how this technology can visualize ciliary muscles and how they behave during active accommodation.
Of course, AS-OCT has other noteworthy limitations. “Anterior chamber OCT scans spot-by-spot, so until you have a very fast system, or a parallel system, it doesn’t cover as much area as quickly as some of the other technologies,” says Dr. Huang.
Practical Uses in the Clinic
Surgeons are now using anterior segment OCT for several purposes:
• When performing LASIK. “AS-OCT is helpful for determining the quality of the corneal surface, and can clearly delineate an existing LASIK flap,” notes Dr. Chopra.
Dr. Huang points out that it’s a highly sensitive way to detect forme fruste keratoconus when evaluating a potential LASIK patient. “I also use it before any retreatment to look at the flap thickness and rule out ectasia,” he says.
• When performing cataract surgery. “AS-OCT can help measure the anterior chamber angle area, which can help determine better approaches for cataract surgery,” says Dr. Chopra. “It also measures the anterior lens vault, which can help determine the level of phacomorphic cataract and the expected improvement.”
• When managing keratoconus. “When you combine anterior topography, posterior topography, the epithelial map and the pachymetry map, corneal OCT provides comprehensive information about the cornea, and it can pick up very subtle changes,” says Dr. Huang. “The problem is that the topography capability hasn’t been FDA-approved and people aren’t familiar with the other maps, so there’s an educational process that needs to take place for clinicians to be comfortable using this relatively new technology. I use it a lot for this purpose, and I teach it, but it hasn’t taken off yet.”
Dr. Chopra says he also uses AS-OCT to monitor corneal thinning in keratoconus patients. “Its detailed corneal pachymetry measurements are very good for this purpose,” he notes.
“I also use corneal OCT before performing crosslinking on keratoconus patients, to make sure the cornea is thick enough,” Dr. Huang adds.
• When treating corneal opacities or irregularities with PTK. “In my practice I do transepithelial PTK and topography-guided PTK,” says Dr. Huang. “Much of the treatment planning is based on OCT scans, looking at the epithelial thickness map and opacity depth measurement to see how deep the ablation needs to go to get the benefit of epithelial masking.”
• When calculating IOL power. “This is very helpful for eyes that have previously had LASIK,” says Dr. Huang. “Many regression-based formulas are specialized for that, and they work pretty well. But I also use the OCT corneal power measurement that includes the posterior surface refractive power. If the two IOL calculations disagree, often the best result comes from averaging them.”
Dr. Chopra agrees. “AS-OCT can reveal the differences between anterior corneal curvature and posterior corneal curvature,” he says. “That can be useful for IOL measurements when the patient has had refractive surgery.”
• When performing laser procedures on the iris. “Angles can be assessed before and after laser procedures such as iridotomy and iridoplasty, and [the technology can] even confirm the patency of a laser PI,” notes Dr. Chopra.
• Measuring astigmatism for toric IOLs. “The speed of current OCT systems is fast enough to be able to use the corneal map scans to measure topography, astigmatism and aberrations,” explains Dr. Huang. “This has been approved outside the United States for several years, but it’s more of a research application in the United States right now. We have an NEI grant to study the measurement of astigmatism and topography with corneal OCT, and we’re finding it’s more accurate than other technologies.”
 |
Angle Evaluation in Glaucoma
Anterior segment OCT has multiple potential uses relating to managing glaucoma:
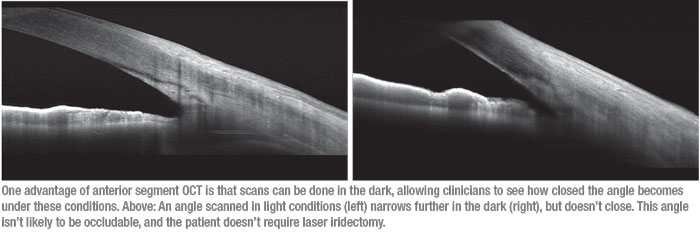
• Evaluating potential angle closure. “Anterior segment OCT can be very helpful if you want to know whether an angle is going to close in the dark,” Dr. Schuman points out. “This is one of the real advantages of AS-OCT technology. You can do an anterior segment-OCT with the lights off, if your environment will permit that, and determine how much the angle closes. Imaging it in dark conditions is probably the best way to determine whether it’s occludable.”
Dr. Chopra says he uses AS-OCT to examine patients suspicious for narrow angles or angle closure. “We regularly use AS-OCT in our clinic on the first visit, along with assessing the RNFL and performing macular ganglion cell analysis,” he explains.
Dr. Chopra points out that AS-OCT and gonioscopy can be quite comparable when analyzing the angle. “However, anterior segment OCT typically finds angles to be narrower than gonioscopy,” he says. “That’s probably because some pupillary constriction occurs during gonioscopy, since light is used to look at the angle, while an AS-OCT scan can be done in complete darkness. However, surgeons can’t use AS-OCT to perform indentation to try to open narrow angles to assess for peripheral anterior synechiae. Nevertheless, AS-OCT can usually distinguish between narrow angles and PAS if an expert evaluator examines the images.”
Dr. Schuman believes the tide may be shifting regarding whether gonioscopy or anterior segment imaging is the more reliable tool for evaluating the angle. “Tin Aung, MD, PhD, spoke at the September 2020 FDA Collaborative Communities on Ophthalmic Imaging conference,” he says. “One of the things he suggested was that gonioscopy—currently the gold standard for judging things like how open or closed the angle is—probably shouldn’t be the gold standard. Imaging should be. It’s hard to argue with that, because gonioscopy involves a subjective judgment made by the observer. The observer may or may not be expert, and even expert observers make mistakes.”
• When performing MIGS procedures. Dr. Chopra says he routinely uses AS-OCT when patients are undergoing angle-based minimally invasive glaucoma surgery. “I use it both before and after surgery,” he explains. “It’s especially useful for teaching residents and Fellows. It lets them see if their targeted procedures have achieved the desired surgical outcomes, in terms of targeting the correct anatomy.”
• For patient education. “The images are incredibly useful for teaching patients about their iridocorneal angle anatomy, especially if they’re asymptomatic,” says Dr. Chopra. “In my opinion, this greater understanding allows a much-more-informed consent for proceeding with laser iridotomy, laser iridoplasty or cataract extraction to treat angle closure.”
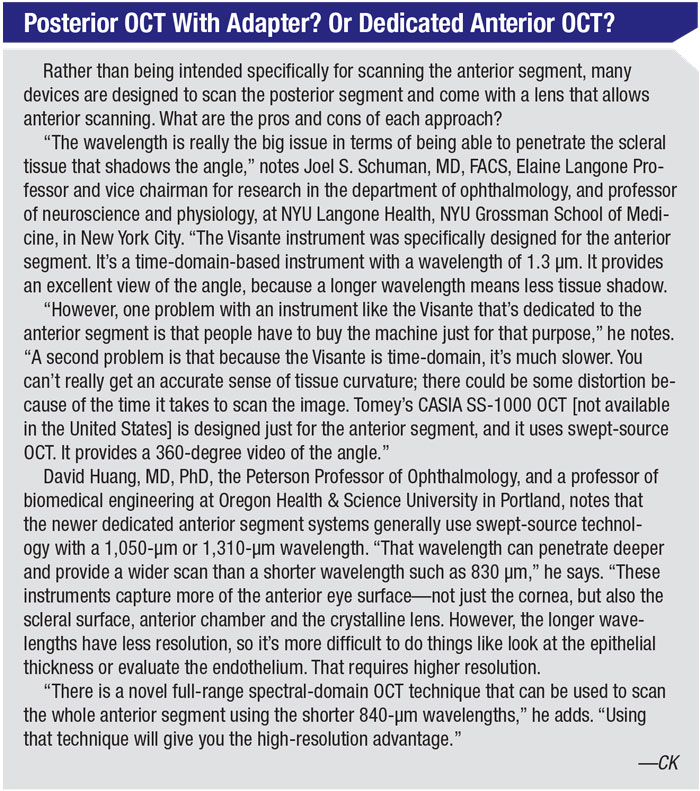
• When evaluating the condition of the angle. While this technology offers some advantages for this purpose, it also has notable limitations. Dr. Schuman says that one potential problem when trying to visualize the angle with OCT is that you can have shadowing from the scleral structures of the angle itself. “Sometimes you can see almost the whole angle, but you lose the most posterior portion that’s really of interest,” he explains. “How much shadowing you see depends on how the images are acquired and the wavelength of the light; the longer the wavelength, the deeper into the angle you’ll be able to see. If you’re using swept-source OCT with wavelength around 1 µm, then you’ll see deeper than with a standard near-infrared OCT.
“I think this has limited the applicability of anterior segment-OCT for viewing the angle, although you can still get a pretty good idea of what’s going on,” he continues. “If you really want to see the angle structure, the ciliary processes and the relationship of the ciliary process to the iris, UBM is a better technology in most cases. The drawback with UBM is that it requires contact. In many cases anterior segment OCT will provide you with sufficient information to be able to make a clinical decision, so it’s worth trying. With it, I can spare the patient some time, and also the contact procedure. However, there may be cases where you won’t be able to get an adequate view using AS-OCT.”
Dr. Schuman adds that when it comes to visualizing the angle, gonioscopy has some capabilities that anterior segment imaging doesn’t. “Those capabilities have to do with what you can see, rather than the openness or closedness of the angle,” he explains. “You can see if there are vessels; you can see pigmentation; you can see the color and character of the tissue. But what most people are looking at when they’re evaluating the angle is whether the angle is open or closed. Are there synechiae? Is it just appositional when it’s closed? Those questions, for the most part, can be answered with imaging. A lot of the value of gonioscopy at this point lies in revealing things that imaging can’t reveal.
“The other advantage of gonioscopy is that you can visualize the angle 360 degrees,” he adds. “It’s awkward and tedious to try to capture 360 degrees with most conventional OCTs that we have in this country. Of course, that’s just a matter of engineering. Obviously it can be done, since it’s already possible using instruments available outside the United States.”
 |
What About Angiography?
Dr. Huang notes that anterior segment OCT angiography is still embryonic, with only a few publications relating to it. “Using this technology you can see corneal, conjunctival and episcleral blood vessels with much higher contrast than you see at the slit lamp,” he points out. “You’ll be surprised by how many vessels there are! It can also evaluate iris vessels to some extent, unless the eye is heavily pigmented. We’re currently looking at iris melanoma and other tumors with longer-wavelength swept-source OCT angiography, which penetrates the tumor better. Tumor vasculature is very sensitive to radiation treatment, making OCT angiography a useful measure of treatment effectiveness.”
“The added benefit of using OCTA in the anterior segment is still being investigated,” says Dr. Schuman. “In most cases, if an eye has enough neovascularization to be considered abnormal, you’ll be able to see it. But OCTA could be useful in some situations, and there are a number of areas to be explored, including cases of neovascularization or tumors.”
Dr. Chopra agrees that it’s not clear yet how useful anterior segment OCT angiography will be. “Currently, the images tend to be filled with artifacts because the vasculature is in so many planes,” he says. “Of course, the software provided by various manufacturers hasn’t been optimized for this purpose. That being said, we’re currently using AS-OCT angiography in our research setting.”
“Anterior segment OCT angiography may be developing more slowly because the diseases it would help to manage are less common than retinal diseases like macular degeneration,” Dr. Huang adds. “Companies aren’t competing to provide software to perform this kind of imaging or provide automated analysis and measurements. But I think eventually these useful applications will be developed. It will just take a little longer to catch on.”
Pearls for Clinical Use
Surgeons offer these tips for those just beginning to use AS-OCT:
• Take advantage of the software provided with your instrument. “Many devices have software that can help you analyze anterior segment images,” Dr. Schuman points out. “That can provide a lot of useful information you couldn’t pick up without it.”
• When measuring depth, measure perpendicularly. “I see a lot of people measuring depths such as opacity depth on OCT cross-sections incorrectly,” notes Dr. Huang. “If you section the cornea at an oblique angle, you can’t measure the depth accurately. You have to have a perpendicular section. The easiest way to do that is to have your technician get a cross-section that goes through the center of the cornea, defined by either the vertex or pupil center, or limbal centering. Then you need a caliper that measures depth perpendicular to the anterior surface.”
• When looking at the angle, be as perpendicular to the tissue as possible. Dr. Schuman makes a related point. “Most surgeons just scan right across the eye, with the eye looking straight ahead,” he says. “However, that will give you a distorted view of the angle. When looking at the angle, you want to be as perpendicular to the tissue as you can be. Try different positions, so you can get the best possible image.”
• Remember to apply the de-warping software correction to depth measurements. “This gets rid of the distortion due to the index transition at the air-cornea interface,” Dr. Huang explains. “If you do a corneal map scan, the measurements are automatically corrected for those distortions. But if you take a cross-section by doing a line scan, perhaps to measure the depth of a corneal lesion, it will measure it as being much deeper than it really is unless you use the dewarping correction.”
• Start by working with healthy eyes. “Practice makes perfect,” notes Dr. Chopra. “Those doing imaging with this technology should start by imaging healthy patients with open angles. That will help the surgeon perfect the techniques that can then be used easily and reliably in more challenging patients with angle narrowing or other angle abnormalities.”
• Expect a learning curve. “Using anterior segment OCT correctly is a learning process,” Dr. Huang observes. “You have to learn what to look for in order to evaluate different things. For example, if you want to diagnose forme fruste keratoconus with the existing corneal mapping software that’s available in the United States, you’ll be looking for epithelial and pachymetric thinning patterns that are different from the patterns you see on topography. So you’ll have to take a course or read up on it to learn to do that.”
What Lies Ahead?
Given the advantages of AS-OCT, it’s worth asking why it’s catching on so slowly. “Anterior segment OCT isn’t turnkey or routine in most offices at this point, unlike posterior segment OCT imaging,” Dr. Schuman points out. “Ophthalmologists are very busy, and any time you do something outside of your routine it takes longer to do it and to interpret it. Also, the number of people who will benefit from this use of OCT will be smaller than the number who benefit from posterior segment OCT imaging, at least initially.
“So, it’s not that anterior segment OCT isn’t useful—it is,” he says. “You can get beautiful images and extract a lot of useful information with it. It’s just that the utility of this technology hasn’t yet been fully exploited. I do think there will eventually be a paradigm shift. However, it may take doctors a long time to accept machine classification of angle status.”
“I think many glaucoma specialists believe that gonioscopy is easy and simple to perform,” Dr. Chopra says. “That may be why they haven’t incorporated anterior segment OCT into their clinic flow.”
“Given the unique advantages of anterior segment OCT,” Dr. Huang notes, “it has a lot of room to grow, in terms of being more widely used. That’s especially true now that there are high-speed systems available that can do topography and widefield scanning of the entire cornea and beyond. I think it will rapidly progress as a technology.” REVIEW
Drs. Schuman and Chopra report no financial ties to any product discussed. Dr. Huang reports that Opto-Vue provides research support to his laboratory and licenses some of the algorithms and technology developed by his research group. He has stock ownership in the company.



