 |
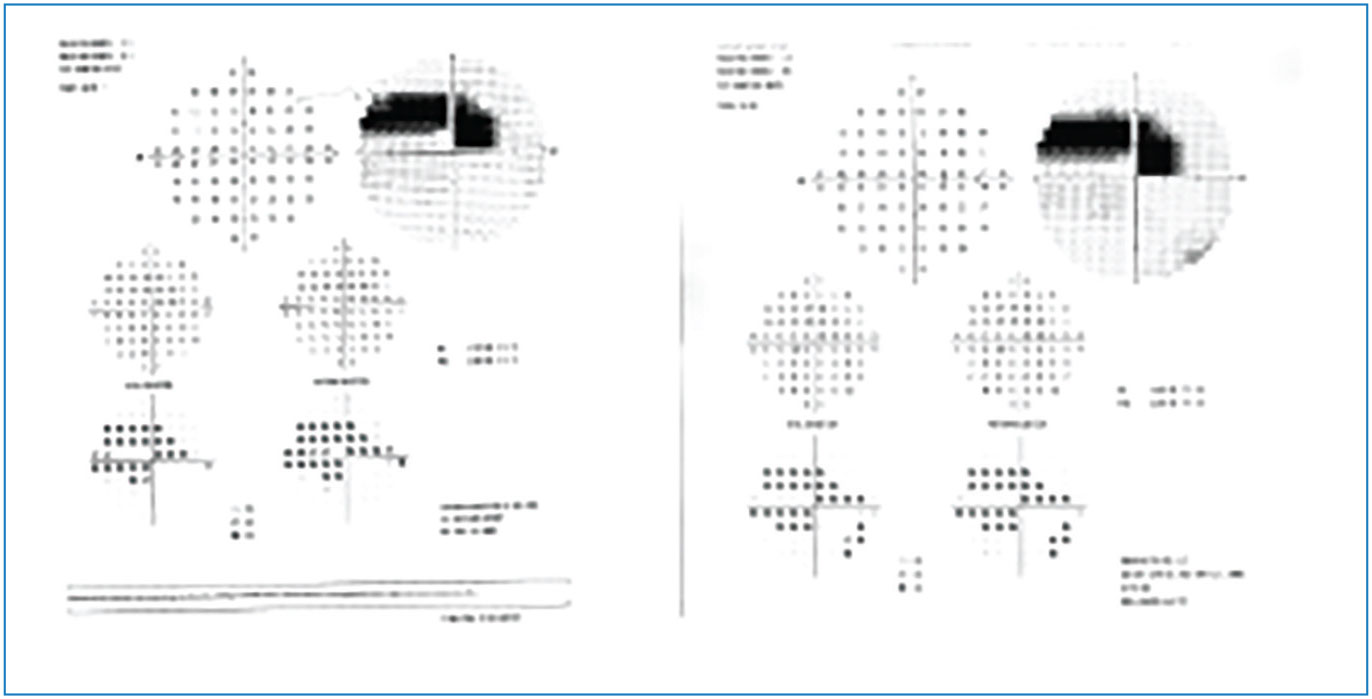
Study shows 10-2 VF testing doesn’t detect any additional defect not already seen on 24-2 testing, but it provides sufficient additional information for patients with a repeatable defect within the central 12 locations of the 24-2 VF test.
In a new Ophthalmic Technology Assessment by the American Academy of Ophthalmology, researchers evaluated the current published literature on the utility of the 10-2 visual field (VF) testing strategy for the evaluation and management of early glaucoma, defined here as mean deviation (MD) better than -6 decibels (dB). They concluded that 10-2 VF testing may not be the most useful routine test for patients with early glaucoma, but would provide sufficient additional information for patients with a repeatable defect on the pupillary distance (PD) plot among the central 12 points on the 24-2 or 24-2C VF test. Their results were recently published in Ophthalmology.
After review, 26 articles in the PubMed database were selected; the panel methodologist rated them for strength of evidence. Thirteen articles were rated level I and eight articles were rated level II, while five level III articles were excluded. Data from the 21 included articles were abstracted and reviewed.
Results from the study found that the central 12 locations on the 24-2 VF test grid lie within the central 10 degrees covered by the 10-2 VF test. In early glaucoma, defects detected within the central 10 degrees generally agree between the two tests. Defects within the central 10 degrees of the 24-2 VF test can predict defects on the 10-2 VF test, although the 24-2 may miss defects detected on the 10-2 VF test.
“In addition, results from the 10-2 VF test show better association with findings from OCT scans of the macular ganglion cell complex,” the authors noted in their report. “Modifications of the 24-2 test that include extra test locations within the central 10 degrees improve detection of central defects found on 10-2 VF testing.”
The authors explained that central VF defects may be underappreciated in the evaluation of early glaucoma. “Although less common in cases in which MD is better than -6 dB, central defects may have a profound impact on a person’s visual function and quality of life. Thus, detection of central VF defects is essential in the diagnosis and management of glaucoma even at the earliest stages,” they explained.
With the extra central test locations, the Zeiss 24-2C or the Octopus G1 test strategies can improve detection of central defects over the standard 24-2 VF, the authors added. Although the 10-2 VF is considered the gold standard for detecting central VF defects, it’s more involved for both the patient and clinician, as it entails additional time, cost and effort, and it may not always detect any additional defect not already seen on 24-2 testing.
The authors say the evidence doesn’t support routine testing using 10-2 VF for patients with early glaucoma. “Recent studies provide some evidence on additional VF testing in some cases, however,” they add. “Early 10-2 VF testing would provide sufficient additional information for any patient with a repeatable defect on the PD plot among the central 12 points on the 24-2 or 24-2C VF test or with a depressed average and/or minimum mGCIPL thickness on SD-OCT. A defect on SAP 10-2 VF warrants confirmation and potentially a lifelong commitment to serial 10-2 VF testing.”
1. WuDunn D, Takusagawa HL, Rosdahl JA, et al. Central VF testing in early glaucoma. Ophthalmology. December 8, 2023. [Epub ahead of print.]
Daily Smoking Linked to Visual Impairment in NTG
Though the relationship between smoking and glaucoma is controversial, current evidence does suggest that tobacco smoke plays a role in the development of ischemia and oxidative alterations in ocular tissues. A recent study was conducted in Serbia to determine whether smoking patterns might be related to vision-related disability among the different subtypes of glaucoma. It found that a higher number of cigarettes smoked daily was associated with poorer visual impairment only among people with normal-tension glaucoma, but not the other subtypes.
The cross-sectional study included 283 patients with primary open-angle glaucoma, primary angle closure glaucoma, normal-tension glaucoma and pseudo-exfoliative. Information about the duration and quantity of smoking was self-reported. To quantify vision-related impairment, each patient completed a validated Glaucoma Quality of Life-15 questionnaire.
After adjusting for nine confounding variables, including age, gender, glaucoma severity, IOP level and lifestyle, the data revealed that the number of cigarettes smoked per day was negatively correlated with vision-related quality-of-life among people with normal-tension glaucoma subtypes. Smoking duration (in years), on the other hand, did not show the same association in normal-tension glaucoma patients.
“It is believed that normal-tension glaucoma is a distinctive subtype of glaucoma that is characterized by a somewhat different pathogenesis compared to other glaucoma subtypes,” the researchers wrote in their paper on the study, published in Ophthalmic Epidemiology. This unique pathogenesis may involve ocular blood flow disruption and vascular dysregulation, which also describes the suspected effect of tobacco on ocular tissue, they pointed out.
 |
Oxidative stress may be another nicotine-dependent mechanism at the sub-cellular level that could contribute to worsening visual function. “It has been identified that tobacco smoking can induce cell inflammation and apoptosis in the eye tissue,” the researchers noted in their paper. “This finding is in accordance with the notion that, in glaucoma, retinal ganglions and cells of the trabeculum die by apoptosis.”
Regarding the lack of an association found between smoking duration and worse visual functioning in normal-tension glaucoma patients, the researchers note that some literature describes a protective effect of nicotine on the optic nerve and suggests it may improve the structure’s blood supply. “This could potentially explain why long and moderate cigarette smoking wasn’t found to be a risk factor for the onset of glaucoma [and] could also be the underlying reason as to why there are so many controversies when the association between tobacco and glaucoma is being assessed,” the study authors wrote.
Limitations of this study include the self-reporting of smoking habits and visual impairment, which introduces inherent bias, as well as the fact that the majority of participants were Caucasian, despite the higher prevalence of certain glaucoma subtypes in people of Asian and African descent.
In conclusion, the authors wrote, “Our findings highlight the need to examine smoking habits among people with glaucoma, especially among people with normal-tension glaucoma, during their health checks and address the issue of smoking as a potential harmful factor that may further damage their vision-related functioning.”
1. Sencanic I, Dotlic J, Jaksic V, Grgurevic A, Gazibara T. Association of smoking patterns with vision-related disability according to glaucoma subtypes. Ophthalmic Epidemiology. December 12, 2023. [Epub ahead of print].
Consumption of Vitamin B1 and Advanced AMD
Investigators studied the association between vitamin B1 consumption and the prevalence of late age-related macular degeneration in a representative U.S. sample.1
Data from the National Health and Nutrition Examination Survey (NHANES) between 2005 and 2008 were used for this cross-sectional analysis. The logistic regression model was used to evaluate the association between vitamin B1 consumption levels and late AMD.
The study included 5,107 people ages 40 and older. Vitamin B1 intake levels were inversely associated with the prevalence of late AMD, with OR being 0.40 (CI, 0.26 to 0.62) for crude model 1; 0.53 (CI, 0.29 to 0.94) for adjusted model 2; and 0.55 (CI, 0.31 to 0.99) for the fully adjusted model 3.
Investigators found that vitamin B1 intake levels were inversely associated with the prevalence of late AMD in the United States. They suggested that further randomized clinical trials among multiple centers is warranted to investigate the longitudinal and causal relationship between vitamin B1 intake and late AMD.
1. Zheng Q, Shen T, Xu M, et al. Association between dietary consumption of vitamin B1 and advanced age-related macular degeneration: A cross-sectional observational study in NHANES 2005-2008. Ophthalmic Res 2023; Nov 3. [Epub ahead of print].
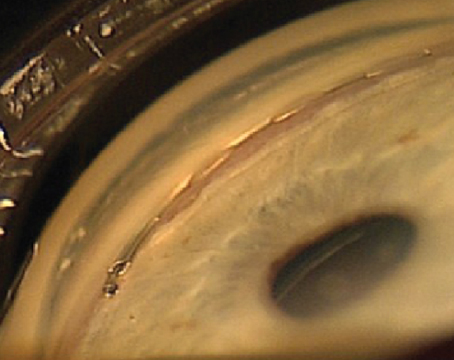
AS-OCT Helps Define Late Ectasia After PK Procedures
The subtype of ectatic disease following penetrating keratoplasty (PK) has been defined poorly in the literature, with the terminology not being consistent. In contrast to Scheimpflug tomography, measurements with anterior segment optical coherence tomography AS-OCT are also possible in corneas with opacity. A research team based in Germany has used this imaging modality to describe morphological parameters of ectatic corneas after PK.1 They noted an acute graft-host interface angle, steep keratometry value, deep AC and a stromal thinning at the interface as significant signs of ectasia. A ratio calculated by the relationship between the thinnest point at the interface and the central corneal thickness was significantly lower in ectatic eyes.
The team included 50 eyes of 32 patients with a history of PK at an average of 25 years earlier were included, 35 ectatic and 15 not. Mean age at time of examination was 63, mean interval between PK and time of AS-OCT examination was 25 years. PK had been performed at an average age of 38. The control group consisted of 30 healthy age-matched eyes (mean age: 62). They assessed steep and flat keratometry readings obtained with AS-OCT (CASIA-2, Tomey) and Scheimpflug tomography (Pentacam, Oculus). OCT findings were correlated with clinical grading of ectasia.
The interval between PK and examination was significantly longer in eyes with ectasia compared with non-ectatic eyes in the study. There was a highly significant difference in lowest corneal thickness at the interface, graft-host interface angle and anterior chamber depth (in pseudophakic eyes) between the groups. The ratio calculated by the quotient of lowest corneal thickness at the interface divided by central corneal thickness (CCT) was significantly lower in ectatic than non-ectatic eyes. In eyes with a ratio of ≤0.7, the odds ratio for the occurrence of a clinical detectable ectasia was 2.4. Steep keratometry values were significantly higher in ectatic eyes.
The researchers thought it was interesting that there was a significant difference of several morphometric and keratometric parameters between the healthy control eyes and the post-PK eyes classified clinically as non-ectatic. “This could be explained either by the steep and thinned corneal recipient rim in keratoconus eyes or by early manifestation of ectasia, which is clinically not yet visible,” they wrote in their paper.
“The value of the morphological characterization of ectatic corneas using AS-OCT is limited insofar as the decision whether to perform surgical or other intervention is based on reduced visual function rather than altered corneal morphology,” the team pointed out. “Since objective and subjective measurements of refraction might prove to be difficult in ectatic eyes, AS-OCT measurements could serve as surrogate markers for progressive ectasia over time but should not be used for surgical decision-making.”
1. Weller JM, Hübner L, Kruse FE, Tourtas T. Characterization of ectasia after penetrating keratoplasty in keratoconus eyes using anterior segment optical coherence tomography. Br J Ophthalmol. March 20, 2023. [Epub ahead of print].
Vision Screening Needed in Parkinson’s Disease
For individuals living with Parkinson’s disease, maintaining good visual function is key for continued ability to work. However, this condition can affect vision, and the findings of a recent survey study showed that few people are aware of this. The paper, published in the American Journal of Occupational Therapy, reported that vision dysfunction affects occupational performance and that greater education about vision difficulties in Parkinson’s disease is needed.
The cross-sectional analysis included 92 persons with Parkinson’s disease who self-reported visual difficulties, diagnosed eye conditions and general awareness of disease-related visual dysfunction in an electronic survey.
The researchers found that almost half of respondents were unaware that Parkinson’s disease could affect vision. They also found that awareness wasn’t associated with disease duration, and that individuals who reported awareness also tended to report vision difficulties. They reported mild impairment for functional activities requiring vision. The frequency of ophthalmologic symptoms was low. These were mostly related to ocular surface disease. However, the researchers reported that a higher frequency of ophthalmologic symptoms was positively associated with a higher degree of disability in activities of daily living.
“If the effect that Parkinson’s disease can have on visual function is not understood by persons with Parkinson’s disease or is overlooked by their health-care provider, the underlying cause of difficulties engaging in daily occupations may be missed or mistaken,” the researchers pointed out in their paper. “Assessing and evaluating visual function in persons with Parkinson’s disease may aid in elucidating changes in occupational performance and help guide targeted treatment approaches as they become available.”
1. Tester NJ, Liu C, Shin Y, et al. Visual dysfunction and occupational performance in persons with Parkinson’s disease. Am J Occupational Therapy 2023;77:7706206060. [Epub ahead of print].
The Benefits of MIGS Plus Cataract Surgery
As many surgeons have suspected, combining a MIGS procedure with cataract surgery may produce meaningful results over time for open-angle glaucoma patients, according to a recent report by the AAO’s Ophthalmic Technology Assessment Committee Glaucoma Panel, which reviewed the current literature on combined trabecular MIGS procedure/cataract compared with cataract surgery alone. While both approaches show good track records for lowering pressure, the combined approach may offer patients a small edge.
The researchers’ PubMed literature search returned 279 articles, of which 20 were graded for quality and 10 of those studies (all level I randomized controlled trials) were included in the final assessment. The researchers noted that all 10 of these studies were “subject to potential industry-sponsorship bias.”
They reported that based on medication washout studies with two-year data in patients with hypertensive, mild to moderate OAG, adding a trabecular procedure to cataract surgery resulted in an additional 1.6 to 2.3 mmHg IOP reduction—i.e., 4 to 9 percent IOP reduction, resulting in an average reduction of about 0.4 medications; vs. cataract surgery alone, which on its own reduces IOP by approximately 5.4 to 7.6 mmHg or by about 21 to 28 percent, possibly eliminating 0.8 to 1 glaucoma medications.
“The three most studied trabecular procedures [iStent/iStent Inject, Hydrus Microstent and excisional goniotomy via Kahook Dual Blade] appear to produce similar results among hypertensive mild to moderate OAG subjects with modest IOP reduction or medication reduction over cataract surgery alone at two years,” the researchers wrote in their paper. “There is no clear benefit of adding one trabecular procedure to cataract surgery over another based on these available data.”
Future research should focus on standardizing outcome definitions, avoiding sponsorship bias and studying efficacy in normotensive OAG, since all studies were in patients with pretreatment IOP of 21 mmHg or less, the researchers pointed out in their paper.
“Although the primary goal for MIGS surgeons is often to reduce the medication burden, the mild mean IOP reduction of approximately 2 mmHg by a trabecular procedure is estimated to result in a mean reduction in number of medications of 0.4 at two years.” Therefore, they wrote that it’s good to tell patients that adding a trabecular procedure can further decrease their medication burden.
1. Richter GM, Takusagawa HL, Sit AJ, et al. Trabecular procedures combined with cataract surgery for open-angle glaucoma: Ophthalmic Technology Assessment. Ophthalmology 2023;1-13.
Letter to the Editor To the Editor: I’d like to comment on the December 2023 article: “The Ins and Outs of Customized LASIK.” It’s my clinical impression that topography-modified refraction isn’t widely used. Phorcides is used by more than 500 surgeons worldwide to make Contoura planning more efficient and far more accurate. The prospective study, published in JCRS (https://pubmed.ncbi.nlm.nih.gov/35171146/), shows results far better than those quoted in the article. Also, prospective studies are considered more powerful and meaningful than retrospective. Phorcides improved results of Contoura in both the retrospective and prospective studies over the FDA study, which is remarkable because the FDA study only used ‘perfect’ corneas, but the studies [with Phorcides] used real-world corneas that have topographic irregularities.
Mark Lobanoff, MD Minneapolis (Disclosure: Dr. Lobanoff is a consultant for Alcon and the CEO and owner of Phorcides) |