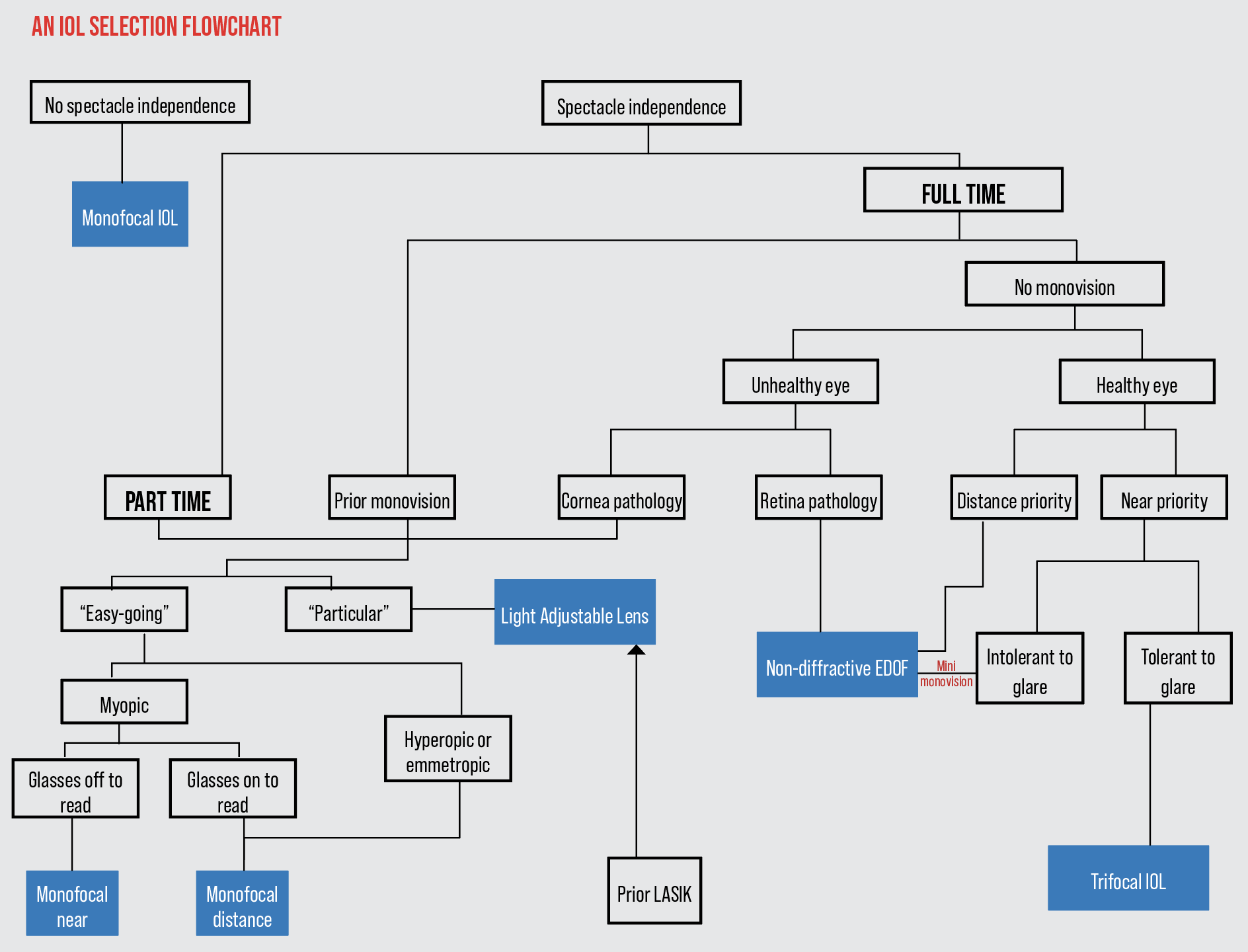
Selecting the most appropriate implant for a patient can sometimes feel like being a matchmaker. Will the patient love the lens you recommend for years to come? Will the lens enrich their life and support them in the activities they love? Cataract surgeons say this process begins with a thorough conversation to get to know the patient. Here, they break down the IOL selection process and discuss several criteria they use when narrowing down their patients’ options.
Patient Personality
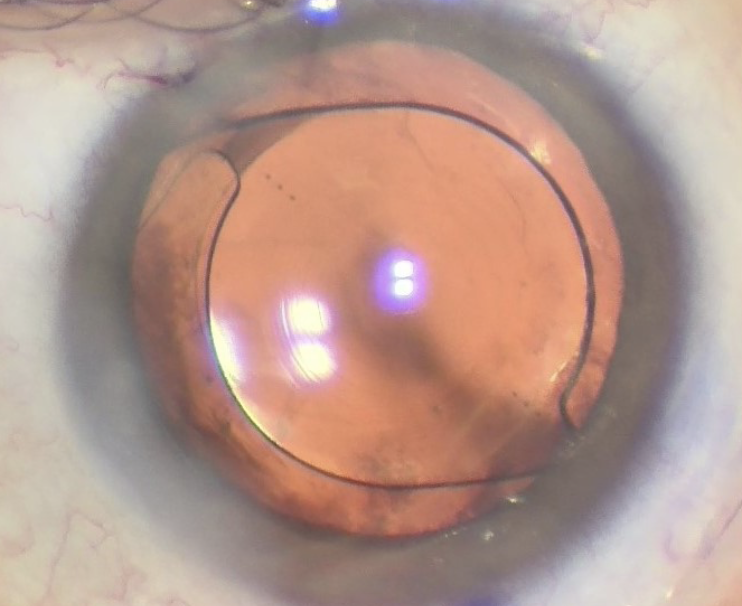 |
| Surgeons avoid implanting diffractive optics such as this trifocal in particular patients. Photo: John Berdahl, MD. |
Personality matters a great deal with selecting a lens for a patient because it’s a good indication of how well they’ll tolerate photic phenomena or be willing to sacrifice some visual quality in exchange for spectacle independence, experts say.
“When we talk about patient personality, we want to know things like whether the patient is anxious or whether they can tolerate a certain amount of uncertainty such as not knowing exactly what distance their vision will be in focus for their activities,” says Y. Ralph Chu, MD, founder and medical director of Chu Vision Institute and Chu Surgery Center in Bloomington, Minnesota. “Can they adapt and accommodate change? Do they really understand what the limitations of each of the technologies presented to them are?”
Easygoing patients are often said to have more lens options than demanding or particular patients because they may potentially tolerate visual side effects better, but Dr. Chu points out that these stereotypes aren’t always true. “When you get really into it, it may not be the patients you think who can’t tolerate a certain technology,” he says. “The stereotypically uptight, demanding patients may understand their needs really well, as well as the limitations of the technology. Many seemingly easygoing patients don’t fully understand the technology. Don’t fall into the trap of stereotyping. Be sure to get to know each individual patient.”
Nevertheless, surgeons say they generally prefer not to implant diffractive optics in particular patients, those with great attention to detail, who notice all their symptoms or who can draw out their different focal points. “These patients will notice all the small decreases and increases in visual quality associated with multifocals,” says Brian M. Shafer, MD, of Chester County Eye Care Associates in Malvern, Pennsylvania. “They’re also likely to be bothered by dysphotopsias such as glare and halo.”
Near, Far, Wherever You Are
In addition to personality, experts say the patient’s visual goals are key for selecting the appropriate optics. How will they prioritize seeing at distance, intermediate and/or near? Do they want full spectacle independence or are they okay with wearing glasses for some activities? “We try to understand how patients want to use their eyes, and the best way to do this is by learning what the patient’s daily life is like and what they want out of their vision,” says John Berdahl, MD, of Vance Thompson Vision in Sioux Falls, South Dakota.
Dr. Shafer says that in general, hobbies are what people derive their happiness from, so prioritizing patients’ abilities to exist most comfortably during their hobbies is important. “While there’s no wrong choice for patients, there are better choices based on their hobbies and interests, so that helps us narrow it down to particular lenses,” he says.
Here are some ways surgeons match patients’ visual goals with IOLs:
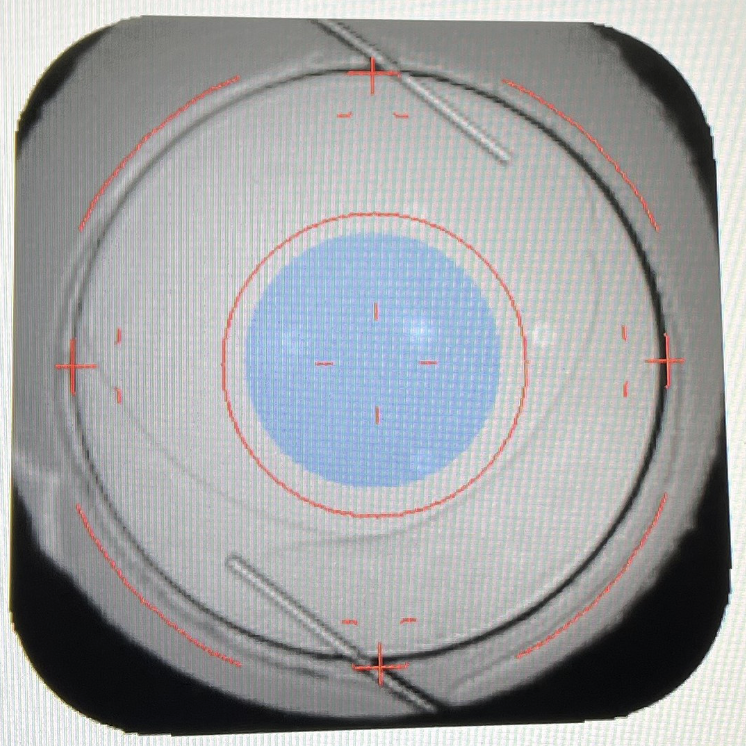 |
| The Light Adjustable Lens is a good option for post-refractive surgery patients because it can be fine-tuned once the eye has healed, surgeons say. Photo: John Berdahl, MD. |
Monofocal IOLs. Monofocal IOLs—including the Light Adjustable Lens and enhanced monofocals such as Eyhance and RayOne EMV—are designed to provide the highest quality vision at a single distance. They have the lowest side effect profile since they don’t split light.
“Patients who want the best possible distance vision, such as those who enjoy hiking and taking in the views, are good candidates for a monofocal IOL targeting distance,” Dr. Shafer says. “These patients will require glasses for near vision. Patients whose hobbies exist in the near range, such as reading or jewelry making, will do well with a monofocal lens targeted for near vision, especially if they’re okay with wearing glasses for driving or watching TV. These patients would prefer not to wear glasses when doing near work.”
Monovision is another visual strategy for certain patients that can provide some increased range of vision, though Dr. Berdahl points out that “it’s one of the trickiest approaches for refractive surgery. With monovision, you’re heavily dependent on the quality of vision in each eye to have a happy patient. We don’t get the forgiveness that comes with both eyes targeted at the same focal point.” He adds that the Light Adjustable Lens is helpful for achieving monovision since the second eye’s target refraction can be adjusted and fine-tuned very precisely after the surgery.
“I’ve had good results using the Eyhance in a mini-monovision strategy,” says Marjan Farid, MD, a clinical professor of ophthalmology and director of the cornea, cataract and refractive surgery program and the ocular surface disease program at UC Irvine School of Medicine. “Though it’s not a presbyopia-correcting IOL, Eyhance can achieve a pretty nice range of vision with few to no side effects.”
Multifocal IOLs. For patients interested in more spectacle independence and a greater range of vision than monofocals, multifocal IOLs such as the Synergy multifocal/EDOF hybrid or the PanOptix trifocal may be suitable. However, gaining sharp vision at multiple distances has its trade-offs due to the splitting of light.
“Because trifocals split light three ways, these lenses come with the expectation of glare and halos,” Dr. Shafer says. “These lenses should be used sparingly in particular patients and those who are more likely to find those dysphotopsias bothersome. Trifocals are better suited for low-key individuals whose hobbies include looking into the distance and near work, such as a fly fisherman who needs both ranges of vision for fishing and tying flies up close.”
Extended-depth-of-focus IOLs. EDOF lenses such as the Symfony OptiBlue and the non-diffractive Vivity create one elongated focal point to enhance a patient’s range of vision. These lenses offer strong intermediate and distance vision, good near vision and few visual side effects.
Reducing visual side effects is an important innovation in lenses that offer greater range of vision. Vivity’s non-diffractive optics stretch light to avoid light splitting, and the Symfony OptiBlue uses InteliLight technology, which is a combination of a violet-light filter, an echelette design and achromatic design. The violet-light filter blocks wavelengths that create the most light scatter to minimize visual disturbances; the echelette design reduces light scatter and halo intensity for easier digital screen viewing; and the achromatic technology corrects chromatic aberration for better contrast during the day and at night, the company says.1
Dr. Berdahl says EDOFs are good options for patients who want to decrease but not eliminate the need for readers and are interested in seeing at multiple distances, such as for watching sports on TV and in a stadium.
Sometimes two different IOLs is the best choice for a patient. Mixing and matching complementary multifocals or EDOFs may improve range of functional vision and decrease visual side effects. Combinations often include a low-add EDOF in the dominant eye and a high-add EDOF in the non-dominant eye; or an EDOF and a multifocal in the dominant and non-dominant eye, respectively.
“I’ve had a lot of success recently using the Symfony OptiBlue with InteliLight in the dominant eye and the Synergy in the non-dominant eye for patients who want excellent distance vision with full range,” says Dr. Farid. “In general, I avoid mixing a diffractive with a non-diffractive optic.”
Accommodating IOLs. In theory, lenses such as Crystalens AO and Trulign adjust as your eye moves, mimicking the natural crystalline lens. Dr. Chu says that these lenses offer some extended range of vision for patients who are okay with wearing a thin pair of readers to read fine print. “Accommodating lenses may be suitable for patients who may not tolerate the risk of nighttime dysphotopsias or who just don’t want to take that visual side effect risk,” he adds.
Dr. Farid says she doesn’t often implant accommodating lenses because the final near point may be unpredictable. “Sometimes these lenses accommodate a little early in the eye and then you don’t get as much range of accommodation,” she explains. “I have more success with fixed multifocal EDOF lenses than the current accommodating lens. But though accommodating lenses aren’t my primary choice, I’d consider one if a patient already had one implanted successfully in their eye; I’d match the lens in the other eye.”
 |
| Photo: Brian M. Shafer, MD. |
Value Determination
A patient’s ideal implant for their visual goals isn’t always a feasible option. While monofocal IOLs are usually covered with the cataract surgery by the patient’s insurance, premium lenses are an out-of-pocket expense.
When finances present an obstacle, the choice of lens becomes a value determination, says Dr. Berdahl. “Patients must consider how much these lenses cost, and how much they’re willing to pay for the additional freedom that comes from less dependence on glasses,” he says. “In studies, quality of life has been shown to improve dramatically in patients who are less dependent on glasses and contact lenses after surgery. Patients’ understanding of the value proposition is important. There’s the cost of the procedure and sometimes the cost of the lens to consider.”
Dr. Chu agrees: “Patients must understand that there’s an elective portion to this as well as a medical portion. The more patients understand before surgery, the more empowered they are to make their own decisions and feel like they’re part of the process.”
Reading Point
Dr. Farid says she considers a patient’s height when choosing an IOL. “The patient’s stature indicates where their reading point will be,” Dr. Farid explains. “A very tall patient’s reading point will be farther out, so that patient might do better with an EDOF lens, as opposed to a very short patient, whose reading distance will be much closer. A shorter patient may do better with a multifocal lens to achieve better near vision.”
Preop Refractive Error
“One of the major factors to consider in IOL selection, besides personality, is the patient’s preoperative refractive error,” Dr. Shafer says. “If you have a hyperopic patient, they typically appreciate any type of lens you put in there, because they’re depending on glasses for things far away and up close.
“Moderate myopes (between -2 and -4 D) are used to taking off their glasses and being able to see up close,” he continues. “They’ve basically got a telescope built into their eyeball. If you take away these patients’ near vision, they’ll be very upset with you because they’re used to that superpower of not needing glasses to read.
“On the other hand, high myopes tend to wear glasses all the time unless they want to hold something about an inch in front of their eyes,” Dr. Shafer says. “These patients tend to do well with different lens choices such as a monofocal set for near; an EDOF set for -1 D to give them a little bit of distance blur but more range up close; or a trifocal set for plano where they’ll still get that 20/20 distance and near vision.”
Young Patients
When faced with a young cataract patient or young refractive lens exchange patient, Dr. Shafer says he thinks about what might happen in the next 20 or 40 years of the patient’s life when he selects an IOL.
“I implant many more EDOFs than diffractive multifocals for a number of reasons,” he says. “My patient population tends to be very observant and therefore doesn’t enjoy the glare and halos associated with diffractive optics.
“I also do a decent number of secondary IOLs for dislocated lenses, and some of these lenses are in patients who are 40 years out from cataract surgery,” he continues. “I think a lot about what happens when we’re doing cataract surgery on younger patients—what if their lenses dislocate? Well, if they have a diffractive multifocal lens that dislocates more than a millimeter, you’re in big trouble. That patient isn’t going to see nearly as well. But, if an EDOF dislocates a little bit, there’s more wiggle room.
“Refractive lens exchange patients may have a perfectly healthy eye at the time,” he adds, “but we don’t know what their eye will look like 20 years from now. They may go on to develop an epiretinal membrane or macular edema or diabetic retinopathy. We shouldn’t use diffractive lenses in patients with those conditions. If the patient were to develop one of those conditions, I’d feel a little responsible for having put a diffractive multifocal in their eye. Such a patient would still be able to function fairly well with an EDOF—particularly a non-diffractive one—even if they developed some posterior pathology.”
Ocular Comorbidities
“Intraocular lenses work best in pristine eyes, but many eyes simply aren’t,” says Dr. Berdahl. “It’s incumbent on the surgeon to make sure that the patient knows their eye isn’t perfect and that that’ll limit their lens options.”
Surgeons says that when they assess ocular health for IOL suitability, some of the problems they look for include ocular surface dryness or meibomian gland debris; astigmatism, corneal dystrophies or corneal irregularities due to scarring or trauma; and diseases such as glaucoma, macular degeneration or epiretinal membrane in the posterior segment.
“If the eye is healthy, the patient has many lens choices, but having corneal or retinal pathology really puts a patient in the monofocal lens category right off the bat,” Dr. Farid points out. “Multifocality is sensitive to any comorbidity or irregularity, so it’s best to avoid these lenses in eyes with pathology.”
Dr. Shafer agrees, noting that regardless of the ocular condition, patients can still have their astigmatism managed. He points out that “patients with retinal pathology inherently have less activity of the photoreceptors and therefore the photoreceptors are already starving a little for light. Implanting a lens that splits light into multiple focal points means there’s less light for each focal point, and that’s not ideal.
“I don’t put diffractive lenses in patients who have any sort of posterior pathology or any prior retinal detachment,” he says. “That being said, patients with posterior pathology do just fine with a monofocal lens and generally do pretty well with an EDOF lens as well.”
In terms of corneal pathology, Dr. Shafer says this is tricky to manage because the corneal pathology scatters the light before it even hits the IOL. “Then, you have poor-quality light hitting the lens and poor-quality light coming out of the lens,” he says. “It’s like ‘garbage in, garbage out.’ I approach patients with corneal pathology different than those with posterior pathology, because when you have posterior pathology, the retina isn’t sensing the light properly. With corneal pathology, the light isn’t focused properly. I tend towards monofocal IOLs for patients with corneal pathology.”
Experts say some of the most challenging cases are patients with ocular surface instability and those with pathology but who also strongly desire spectacle independence. “When patients have ocular surface disease, we have to take our time and ensure we’ve stabilized the ocular surface and tear film before taking measurements and finalizing our IOL choice,” Dr. Farid says. “Ocular surface disease can really impact biometry and topography. The more the preoperative biometry and topography measurements match, the more confident we are in the lens selection; the less they match, the more inconsistent they are, the trickier it is to select the lens power.
“For these cases, I’ll put the surgery on hold to make sure the patients are getting the proper treatment for tear film dysfunction and ocular surface disease,” she says. “We might bring them back twice or even three times to make sure their measurements are making sense and their ocular surface is clear. We’ll get better outcomes and better patient satisfaction this way.”
“I find the trickiest IOL selections are patients who hate wearing glasses and want full spectacle independence but also have pathology,” Dr. Shafer says. “These patients require extra chair time and additional preoperative visits to determine 1) whether they can tolerate the loss of near vision and be okay with the fact that they can’t see up close as well as they used to; 2) whether they could possibly tolerate a little bit of monovision; and 3) whether they could potentially tolerate both eyes being set for -1 D and having a slight distance blur but still have their full range of close vision. These are really tricky conditions because of all the preoperative counseling and because the patient has to sacrifice something. There’s no perfect lens out there.”
Previous Refractive Surgery
“What surgeons are mainly concerned about is that a surgical procedure on the cornea such as LASIK or RK can change the shape of the cornea and lead to a small loss of contrast sensitivity that may not have been measurable when the patient was younger and had just had corneal refractive surgery,” says Dr. Chu. “When we add a lens implant that has multifocality but also decreases quality of vision or contrast sensitivity, the two stacked together can cause a situation where the patient is unhappy with their lens implant results.”
Dr. Shafer says post-refractive surgery patients fall into two categories: those who have normal topography (where there’s no reason to believe their eyes won’t focus light properly) and those who have irregular astigmatism (whose eyes won’t refract light properly). “The patients in the latter category with irregular astigmatism fall into the same category as the patients with corneal pathology,” he explains. “No matter what type of lens the light hits, it’s going to come out wrong.”
For post-refractive patients who can still refract light normally, Dr. Shafer says he prefers to use the Light Adjustable Lens. “The reason I prefer the Light Adjustable Lens is because we can fine-tune it,” he says. “Almost all of our formulas for measuring IOL power assume the patient hasn’t had refractive surgery. Now there are newer formulas that do, but they’re not perfect—and even on our best days, we can only be within half a diopter of our targeted spherical equivalents in post-refractive eyes 60 percent of the time. The other 40 percent of time, we get it wrong.”
“The Light Adjustable Lens is the only lens where I can guarantee patients a certain outcome because we can make fine adjustments on both the astigmatism and the range of vision,” Dr. Farid notes. “I like to do these surgeries bilateral, same day. Patients do very well with a bit of mini monovision, as there is a degree of extended range of focus that the IOL has, especially after the first adjustment.”
Dr. Chu also uses the Light Adjustable Lens in patients whose refractive outcomes are unpredictable due to past corneal refractive surgery. “This lens works well in patients who want precise vision and some extended depth of focus. To be a candidate for the Light Adjustable Lens, patients must have an adequate pupil size of about 6 mm or more. Having adequate pupil size with the light adjustable lens is important for adjusting the entire surface area of the lens, in our experience,” he says. “We assess the patient beforehand to ensure their pupils dilate sufficiently.”
He says that pupil size is important for multifocal and aperture-type lenses as well. “If the pupil is smaller than the central zone of the optic, the patient may not get as much effect from the IOL’s multifocality, depending on the type of lens,” he notes. “Understanding pupil size in relation to a lens is key for determining patient suitability for a lens in the decision-making process.”
“My approach is to ask the patient if they were happy with their vision right after their refractive surgery,” says Dr. Berdahl. “If they were, then it’s likely their quality of vision is good. If the patient has irregular astigmatism on topography, a gas-permeable over-refraction as part of the cataract workup is very helpful. If the vision improves with gas-permeable over-refraction, then the cornea is contributing to the issue and good uncorrected vision may not be possible.
“My go-to lens in post-refractive surgery patients is the Light Adjustable Lens because of the inherent unpredictability associated with prior refractive surgery,” he continues. “The LAL is adjusted after the patient heals from surgery, so the treatment is based on the manifest refraction after the patient’s healed. We do use multifocal and EDOF lenses in post-refractive patients, however these patients need to be counseled because it’s more likely that they may not get the intended target, they may have visual disturbances or their lenses have a higher likelihood needing to be removed. Also, it can be more difficult to perform a refractive surgery enhancement on top of prior RK, LASIK or PRK.”
New Technology
Some surgeons say they’re looking forward to offering patients two new lenses:
 |
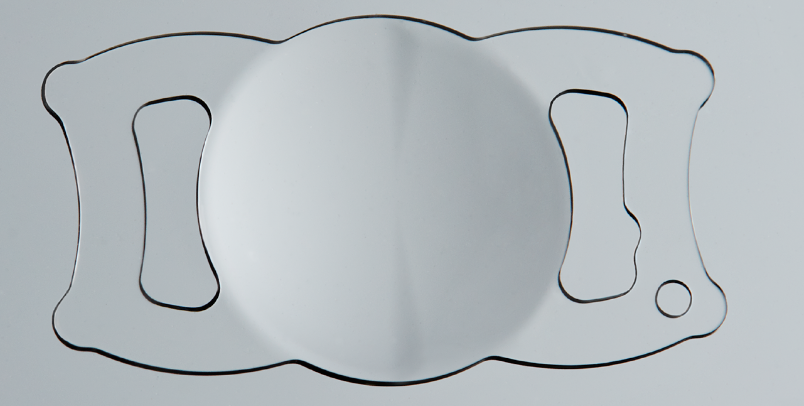
| Some surgeons say they’re looking forward to offering the small-aperture IC-8 Apthera to their patients with irregular corneas. Photo: Y. Ralph Chu, MD. |
IC-8 Apthera. FDA-approved in July 2022, this small-aperture lens from AcuFocus uses pinhole technology to achieve an extended depth of focus by filtering out peripheral defocused light and aberrated light.2 It’s suitable for patients with as much as 1.5 D of corneal astigmatism. Experts note that one trade-off with pinhole optics is a reduction in monocular contrast sensitivity.
In the U.S. Investigational Device Exemption study, 453 subjects received either the Apthera in one eye and a monofocal or monofocal toric IOL in the fellow eye (n=343); or monofocal or monofocal toric IOLs in both eyes (n=110). According to the study, Apthera-treated eyes maintained 2 D of extended depth of focus and provided 0.91 D of additional range of vision over the control group at a 0.2-logMAR threshold, which AcuFocus notes exceeds the 0.5 ANSI criterion for EDOF IOLs. Compared with the control group, the treatment group demonstrated equivalent UDVA; statistically better intermediate and near vision; and comparable binocular contrast sensitivity in photopic and mesopic conditions.2
“This approval opens up a lot of potential for enhanced mini monovision in patients, where we’d implant a monofocal lens set for distance in the dominant eye and a pinhole optic in the non-dominant eye to offer extended depth of range,” Dr. Farid says. “We’re looking forward to offering this option to our patients for presbyopia correction but also for irregular corneas.”
Dr. Shafer agrees, noting that though the Apthera is approved for presbyopia correction, “the majority of us aren’t looking at the lens in that light. We’re looking forward to having this lens available for our patients with highly aberrated corneas. As I mentioned before, with these corneas, it’s ‘garbage in, garbage out.’ But a pinhole optic will take the garbage that comes in, focus it through a small aperture, and allow only that already focused light to make its way through to the retina. So, this is a great option for patients who are post-RK, post-penetrating keratoplasty or have active keratoconus or other forms of ectasia. I have a couple of patients already who are waiting for me to call them as soon as I have access to this lens.”
 |
|
The ClearView 3 segmented IOL can be rotated to reduce dysphotopsias while maintaining distance and reading vision, says Y. Ralph Chu, MD. Photo: Y. Ralph Chu, MD. |
ClearView 3. Dr. Chu was a clinical investigator for the Apthera as well as another new addition to cataract surgeons’ armamentarium: the recently rebranded ClearView 3 asymmetric segmented multifocal lens (formerly the SBL-3) from Lenstec, which was also FDA approved in July 2022. The lens is available in 0.25-D power increments and features “a true 3 D sector-shaped add with a seamless transition zone between the distance and near segments,” according to Lenstec.3
In the FDA clinical trial, 495 patients received either a conventional monofocal IOL or the ClearView multifocal in at least one eye. The ClearView provided improved near visual acuity and comparable intermediate and distance vision at six and 12 months after surgery. According to patient questionnaires, those who received the ClearView IOL reported lower usage of readers or near-vision contact lenses than those who received monofocal IOLs.4
“We’re still learning the best patient profile to offer these bifocal segmented lenses,” says Dr. Chu. “But an advantage is that patients already understand the distance and reading segments of bifocals. The ClearView offers the range of focus of a multifocal lens with a little less dysphotopsia, as well as the ability to potentially reduce this without having to do an explant. If a patient has dysphotopsias, the segmented lens can be rotated, and oftentimes that will reduce or eliminate dysphotopsias and still preserve the ability of the lens to give distance and reading vision. So, that’s an exciting option to have.”
Dr. Berdahl is a consultant for Alcon, Johnson & Johnson Vision, RxSight and Zeiss. Dr. Chu is a clinical investigator for AcuFocus and Lenstec, and a consultant for Bausch + Lomb and RxSight. Dr. Shafer is a consultant and speaker for Alcon. Dr. Farid is a consultant for AcuFocus, Alcon, Bausch + Lomb, Johnson & Johnson Vision and Zeiss.
1. Johnson & Johnson Vision Introduces all purpose EDOF, Tecnis Symfony OptiBlue IOL, the latest pc-iol powered by InteliLight Technology. https://www.jjvision.com/press-release/johnson-johnson-vision-introduces-all-purpose-edof-tecnis-symfony-optiblue-iol-latest. Accessed December 12, 2022.
2. Acufocus announces FDA approval for the IC-8 Apthera intraocular lens, the first and only small aperture lens for cataract surgery. https://acufocus.com/press/aptheraiolfdaapproval. Accessed December 8, 2022.
3. ClearView 3 multifocal IOL. https://www.lenstec.com/clearview3.html. Accessed December 8, 2022.
4. SBL-3 multifocal intraocular lens – P200020. https://www.fda.gov/medical-devices/recently-approved-devices/sbl-3-multifocal-intraocular-lens-p200020. Accessed December 8, 2022.





