The FDA LASIK Study
In 2009 the Food and Drug Administration, National Eye Institute and Department of Defense began a study aimed at better understanding the risk for severe complications after LASIK. The effort, known as the LASIK Quality of Life Collaboration Project, consisted of surveys administered to military personnel receiving LASIK (n: 262) as well as to civilians undergoing the surgery at five U.S. sites (n: 312). The follow-up was three months.
In the military arm, called Patient Reported Outcomes with LASIK-1, the mean preop spherical equivalent error in the myopic eyes was -2.9 D. The mean in hyperopes was +2.5 D. In the civilian study group, designated PROWL-2, the mean SE in myopes was -4 D, and the mean in the hyperopic eyes was +2 D.
At three months, looking at both groups, at least 95 percent of patients saw 20/20 or better. Only one eye (in PROWL-1) lost two or more lines of best-corrected vision.
Patient satisfaction results were high in both arms of the study. “In PROWL-1, 99 percent of patients were satisfied with their outcome and in PROWL-2, 96 percent were satisfied,” avers Edward Manche, MD, a PROWL-2 investigator and the director of cornea and refractive surgery at the Stanford University Eye Laser Center. “There’s been some meta-analysis in the literature and this really goes along with what that analysis has found.”
 |
In presenting the study, two of the organizers’ focal points were visual symptoms, such as glare and halo, and dry-eye disease. Though the prevalence of visual symptoms overall didn’t increase postoperatively, a percentage of a small sub-group of patients who had no symptoms preop reported them at three months (31/71 patients in PROWL-2 and 31/69 in PROWL-2). In terms of dry eye, at three months, 23 percent of patients without preoperative dry-eye symptoms developed mild dry eye, 5 percent developed moderate dry eye and 4 percent reported experiencing severe dry eye.
Dr. Manche notes, however, that a possible shortcoming in the study is that these patients were only followed for three months, and that a longer follow-up, and the potential use of enhancement procedures, would improve the results. “I’ve done many studies looking at LASIK outcomes and I’ve found that the incidence of the signs and symptoms of dry eye are most pronounced between one to three months, and then improve markedly at six to 12 months,” he says. “This also applies to glare, halo and starbursts. These symptoms are more pronounced in the early postop period and then tend to subside at six to 12 months. Plus, if you look at the whole study group rather than these small subgroups, the prevalence of visual symptoms did not increase. As a matter of fact, the incidence of every single one of them went down. Interestingly, the Navy’s PROWL-1 study reported that there were more patients with resolution of the visual symptoms that they had preoperatively than patients who developed new ones.
“Another thing that needs to be taken into account is that no enhancements were done,” Dr. Manche adds. “One of the most common causes of glare and halo is residual refractive error, so it’s quite possible that if you enhanced patients who also happened to complain of halo and glare that most of them would improve.”
To view the study results, visit http://tinyurl.com/olqxout.
LASIK vs. the Alternatives
Indianapolis surgeon Francis Price Jr., and his wife Marianne Price, PhD, decided to conduct a prospective, multicenter, longitudinal survey study of LASIK patient satisfaction, but wanted to do it differently than it’s been done in the past by including a control group. To accomplish this, they introduced a group consisting of contact lens wearers.
The initial online surveys of 2,000 patients were conducted at 22 U.S. practices and three international sites, and patients are going to be followed for three years. Fifty-nine percent of the patients underwent LASIK and the remainder continued wearing their contact lenses.
Dr. Frank Price says a control group helps researchers avoid assigning blame erroneously. “If you’re going to look at patients’ subjective opinions about how their vision is and how they function, you really need a control group,” he says. “This is because there’s a tendency to assume that any patient-reported problems after a procedure were caused by the procedure.”
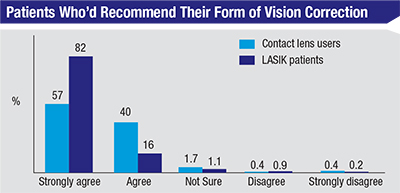
In terms of overall satisfaction, 98 percent of the LASIK patients and 97 percent of the contact lens patients “agree” or “strongly agree” that they’d recommend their vision correction method to a friend or family member. (See graph, above) Interestingly, and highlighting the usefulness of a control group, only 40 percent of the glasses and contact lens wearers reported no difficulty with night driving, and just around 10 percent reported moderate difficulty. These proportions didn’t change significantly at one and two years in patients who continued in contact lenses. In the patients who had LASIK, however, the proportion who said they had no difficulty driving at night due to vision difficulties actually improved postoperatively to 60 percent. This result was maintained at two years.
On the dry-eye front, at one year 30 percent of the contact lens group reported not having any dry-eye symptoms in the past week, and 15 percent said they had some symptoms at least half the time. These results stayed relatively stable through two years.
In the LASIK group, the percentage reporting never having feelings of dry eye (45 percent in both the LASIK group who had worn contacts previously and the LASIK group who had worn glasses previously) decreased at the first-year mark (down to 40 percent in contacts-to-LASIK; 26 percent in glasses-to-LASIK). This result began to improve at two years, with 46 percent of the contacts-to-LASIK group reporting no dry-eye problems and 38 percent in the glasses-to-LASIK group having no difficulties.
“In the patients who had worn glasses before their LASIK, there was a noticeable increase in the prevalence of dry eyes at one year,” says Dr. Marianne Price. “We suspect a lot of the glasses wearers are contact lens intolerant. On the survey, we asked them if they had ever tried contact lenses, and if so, why they discontinued them, and it turned out that 75 percent had tried them, and the most common reason for discontinuing them was discomfort or dry eyes.”
Dr. Frank Price says the study helped show that neither patients, nor the vision correction options they choose, are perfect. “A huge surprise was the amount of difficulty glasses wearers were having with night driving due to their vision,” he says. “This was a huge surprise, especially in light of how regulatory agencies view eye-surgery studies. They tend to assume that when you wear glasses, everything is perfect. But that’s not real life.” REVIEW
The Prices note that their research receives no corporate funding, so any tax-deductible donations to their organization, The Cornea Research Foundation, will help them complete the three-year study.