 |
In May, when the last of thousands of shuttered ambulatory surgery centers reopened following COVID-19 shutdowns, popular wisdom suggested that refractive surgery procedures would be few and far between. Surgeons spoke of working the phones to get cataract patients back in the chair, mindful of the virus’ potential to keep the elderly away unless they were motivated by worsening of cloudy vision. With sudden unemployment and a plummeting economy taking a toll on personal finances, patients weren’t expected to pay from their pockets for such elective procedures as LASIK, SMILE and PRK.
Indications suggest that the opposite might be true, however.
“Because each state executed an individual response plan with differing restrictions, naturally the return to refractive practice has been uneven from a national perspective,” says Jim Wachtman, chairman of the American Refractive Surgery Council, composed of industry representatives and medical professionals with expertise in developing, researching and using the technologies and techniques behind advanced refractive—or vision correcting—surgical procedures. “That said, early indications relating to procedure volume are encouraging. Whether or not that is from pent-up patient demand from the shutdown is yet to be determined. However, a preliminary analysis of our consumer data shows interest among prospective refractive patients which may support an uptick in procedures.”
Of the six surgeons contacted for this article—hailing from California to India—all but one report unanticipated demand for surgical correction of vision among their patients. The one exception, Bryan Lee, MD, JD, who’s in private practice at Altos Eye Physicians in Los Altos, California, and an adjunct clinical assistant professor of ophthalmology at Stanford University, has noticed neither increased nor decreased demand. “But refractive is a small percentage of my practice,” he adds.
Meanwhile, Eric Donnenfeld, MD, of OCLI Vision, who operates at Island Eye Surgicenter in Westbury, New York, says the number of LASIK and PRK procedures has increased by 10 to 20 percent at OCLI since he and his colleagues reopened. “For these patients, I think having their vision rehabilitated gives them a sense of control that they need in today’s environment,” he says. “They’ve lost control over a lot of their lives. And this is one thing that they can do to make their lives better and more in control.”
In this report, surgeons who have experienced recent success in this segment of their practices offer advice on how to identify and meet changing needs in your patient population.
Why More Interest?
Surgeons cite a number of theories on why more patients are electing to undergo refractive surgery now. Below are some trends surgeons have noticed, plus advice on how you might tap into them.
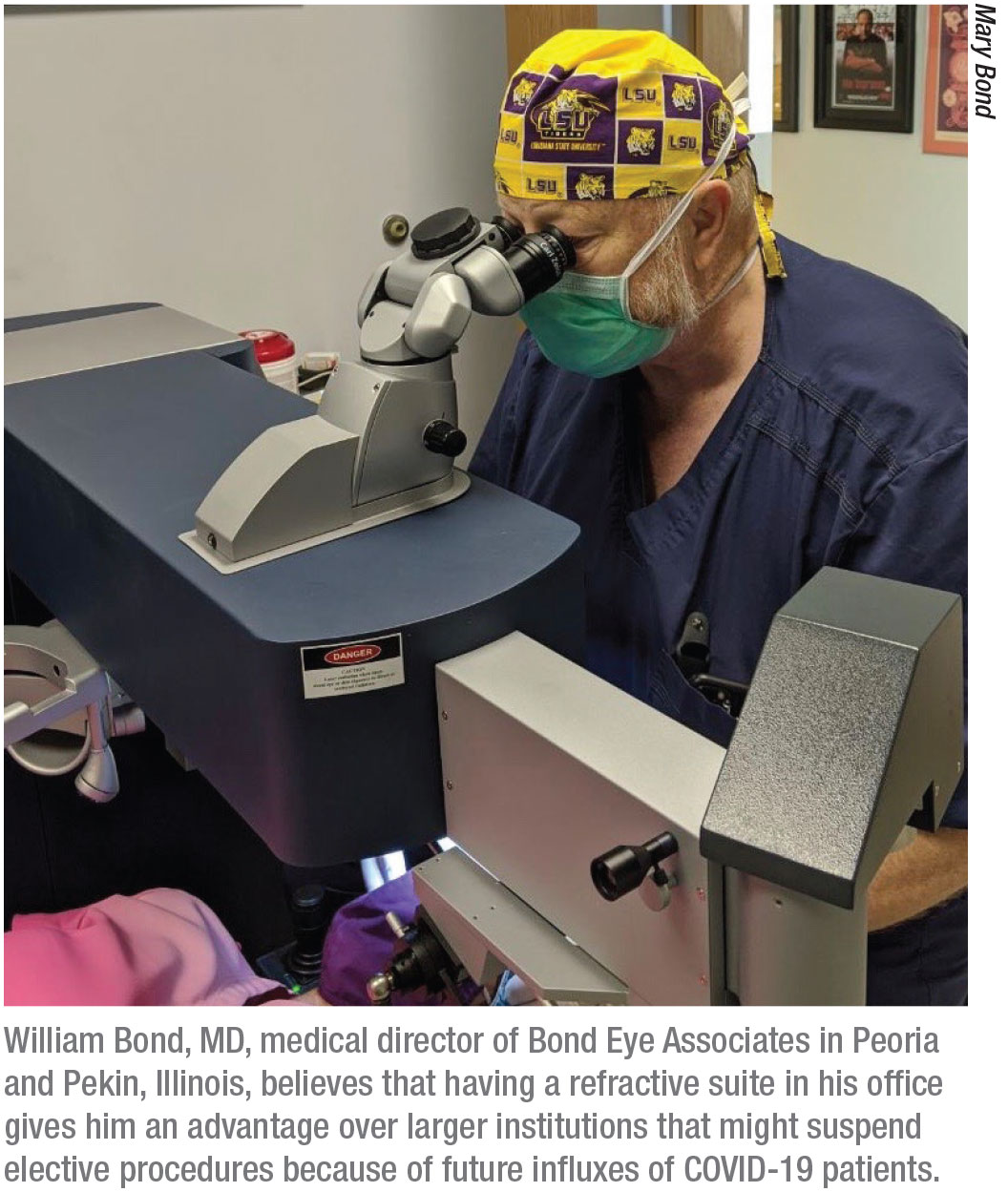
• It’s “now or never.” Patients frustrated by being shut in during the spring may have grown concerned that future lockdowns will block their access to vision correction during the next year or so. William Bond, MD, FASC, medical director of Bond Eye Associates in Peoria and Pekin, Illinois, recommends asking patients how the lockdown has affected them, specifically how it’s affected their vision. “A lot of patients think about getting LASIK but don’t get around to making a decision,” he says. “This environment has given them a little push. I’ve certainly seen it in my practice. For a lot of people, this is like thinking about buying a car. You think about it and you think about it and then, all of a sudden, you do it. This seems to be a time when patients are making those kinds of decisions.”
• Eliminating glasses and contact lenses. David R. Hardten, MD, FACS, in private practice at Minnesota Eye Consultants in Minneapolis, sees more patients than usual who are fed up with their spectacles. “They’re experiencing increased frustration from having to wear masks and shields at work and everywhere else they go,” he says. “They’re dealing with the fogging of their glasses and the tendency of others to concentrate more on their eyes (potentially making these patients more self-conscious). Overall, patients are dealing with a sense of loss of control that they want to avoid.”
Contact lenses may also be a concern for patients worried about infection spread, surgeons say. Eliminating the need to insert, adjust and remove lenses could motivate them to consider a surgical alternative. “Refractive surgery demand during the COVID-19 pandemic doesn’t seem to be waning in Minnesota,” asserts Dr. Hardten.
• Not everyone is broke. Surgeons note that many patients have more cash in their pockets from government grants and expanded unemployment benefits. “When they were laid off, some people ended up making more money than what they were earning when they were working,” notes Dr. Donnenfeld. “Some people have also seen their expenses reduced. No money is going out for childcare, gasoline for the car, eating at restaurants or other activities.”
Demographic Needs
Surgeons have also succeeded by responding to the special needs of patients. For example, Yuri McKee, MD, MS, a corneal and refractive surgeon at East Valley Ophthalmology in Mesa, Arizona, notes that he was spreading himself too thin by offering corneal refractive procedures in Mesa, populated by a high concentration of senior citizens.
“I wasn’t doing a lot of corneal refractive surgery because I was doing a lot of cataract/refractive surgery,” says Dr. McKee. “But the pandemic has kind of pushed me over the edge. Just about all I’m doing now is cataract-refractive procedures.”
The only pure refractive procedures he performs now are natural lens exchanges for occasional severe hyperopes who want to get rid of their thick glasses. The rest of his surgical base now consists entirely of cataract patients. COVID-19 has compelled him to reduce surgery from an average of four cases to two cases per hour, he says. COVID-related paperwork, mandatory COVID-19 testing in Arizona and infection control measures have slowed down the flow. He can only operate on Mondays because of all the pathology he has to manage on the other days. Nonetheless, he is satisfied with the transition to cataract-refractive surgery only.
“We made some good changes,” Dr. McKee says. “My premium conversion rate has vastly improved. I don’t know why people are choosing these options—perhaps, at a time like this, they realize that life is short and they might as well live happily.”
Dr. Yuri’s presentation has made a difference. “I don’t let any astigmatism go unnoticed by patients. I tell them: ‘Here’s your astigmatism. You can see it right here. You’re going to need to fix it one way or another. You have to fix it. The question is: How will you fix it? With glasses, contact lenses, LASIK or during cataract surgery?” He gives them a week to consider the options and asks them what their preference might be when they return for testing. “We never hard-sell,” he points out. “But now I’m implanting more torics than regular IOLs.”
Part of his success has made been possible by the Lensar femtosecond laser, which he uses for all patients at no charge during the capsulotomy and the first half of surgery; for an extra fee he also completes the surgery with the laser.
“There seems to be no end to the demand for these procedures,” he says. “Our only limitations now are limitations imposed by COVID-19, available surgery time and capacity. But it’s going very well for us.”
 |
Rohit Shetty, MD, PhD, FRCS, vice chairman of Narayana Nethralaya Eye Institute in Bangalore, Karnataka, India, says he has noticed a decided shift in motivation among patients who are seeking refractive surgery at his practice. “I ask every patient why they want to undergo refractive surgery,” he says, noting that the percentage of patients choosing refractive surgery has grown by 18 to 21 percent in his practice during the past two to three months. “In the past, the reasons were related to lifestyle changes. Now I hear from just about every one of these patients that they’re making this choice because they’re working at home all the time, and many more hours, sometimes in poor lighting, always indoors, and not always in the best environments for work. They are tired of using contact lenses and spectacles, and they instead want the best vision they can get.”
Dr. Shetty says he expects this trend to continue. “COVID-19 and the constant work at home has been a wake-up call for these patients,” he says. “It’s as if they’re thinking that they don’t know what’s going to happen next, not even tomorrow, and that this uncertain time is when they should undergo a procedure that they’ve been thinking about for a long time. As long as we can tell the patient that this type of surgery is safe in the COVID-19 environment, we should see more refractive surgery procedures than we’ve ever seen before, despite the economic decline. Safety is a very important concern, however.”
More on Safety
Above all, busier-than-expected surgeons in the United States, echoing Dr. Shetty, recommend you stick to two essential priorities:
• assuring patients that they will be safe in your surgical suite; and
• ensuring that they really will be safe, by keeping up to date on how the virus is being transmitted in different settings.
Waiting-room chairs have been significantly reduced. Patients are not moved from room to room for testing as much. Every touch point is sanitized, and surgery is practiced under as pristine conditions as possible. “We have the patient wearing a mask, which makes me happy,” says Dr. McKee. He says he has mixed feelings about the pandemic-related administrative burden associated with every patient. Unlike most states, Arizona requires ophthalmologists and other surgeons to have their patients test negative for COVID-19 before undergoing elective procedures. “We’re certainty taking every precaution,” says Dr. McKee. “It can take seven days to get the results, so it’s been a bit of a challenge for our surgery scheduler. We’re still waiting for the delivery of a COVID-19 testing machine we ordered when the pandemic started. That will reduce testing to 15 minutes in our office.”
Dr. Hardten says helping patients find better solutions for their vision makes the use of precautions very important to him, his colleagues and staff. “We do screening for COVID-19 with a symptom list and by taking temperatures before patients enter the clinic and the laser suite,” he says. “Taping the patient’s mask to reduce fogging of any optics during the surgery is also important. Continued universal precautions, as with any surgery, are also important. So even in this time of COVID-19 spreading through our communities, we can continue to help these patients reduce their dependence on glasses and contacts.”
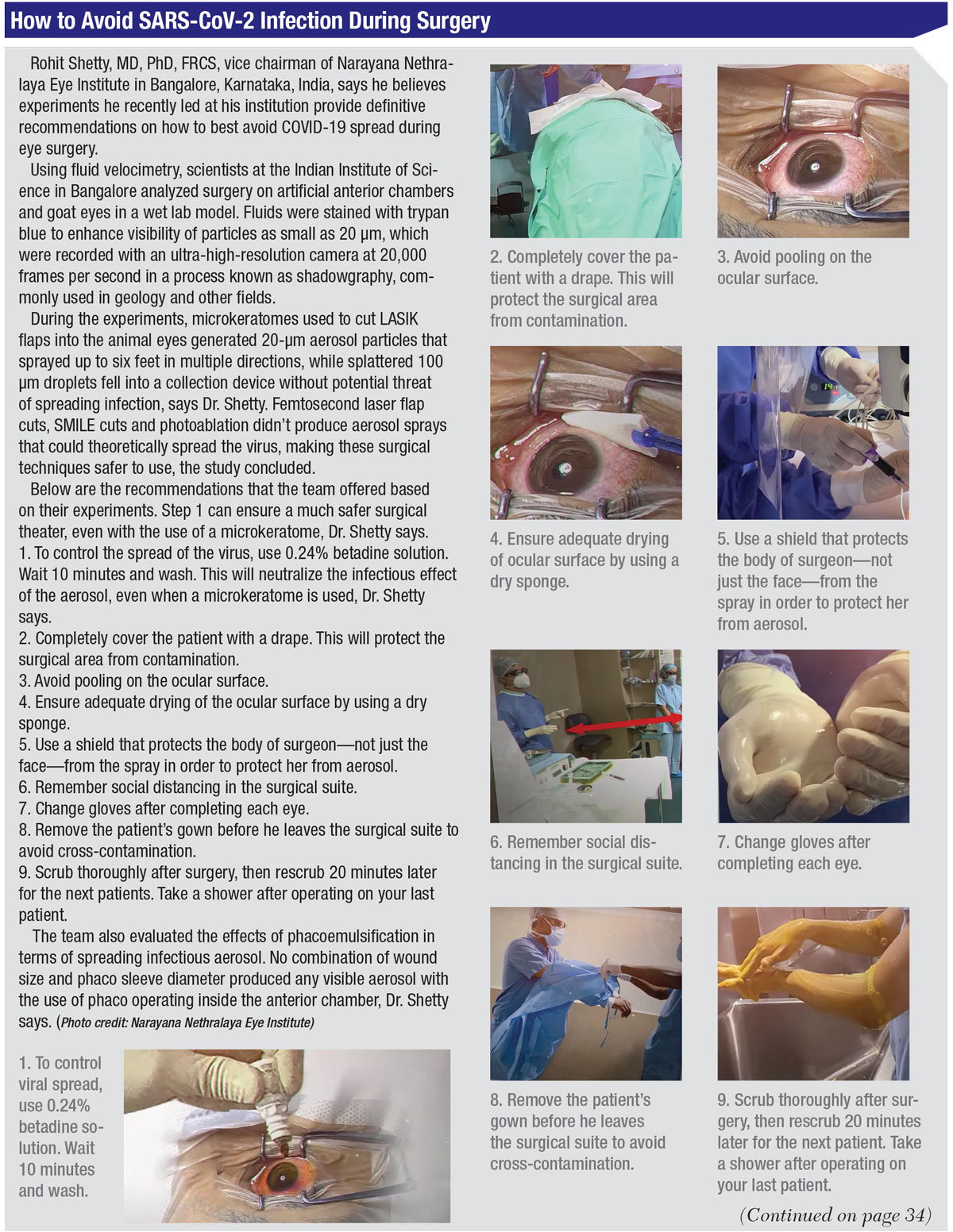
Exactly what measures should be taken to ensure safety has been a topic of discussion and debate among some surgeons. Dr. Shetty says he believes experiments he recently led at his institution provide definitive recommendations on how to best avoid COVID-19 spread during ophthalmic surgery. He notes that the findings of his team were validated by the Institute of Science, Department of Mechanical Engineeering in Bangalore and that they match recommendations published by the World Health Organization on July 9, “Transmission of SARS-CoV-2: implications for infection prevention precautions,” which can be found at: who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions.
Dr. Shetty says he’s looking forward to the publication of a paper on his team’s findings that was recently accepted for publication by a research journal. (See “How to Avoid COVID-19 Infection During Surgery” below.)
 |
Will This Apparent Uptick Last?
No one is certain how long the success that some refractive surgeons are reporting will last. Refractive surgery procedures have been on the decline in recent times, and some believe this trend will continue in the long term. Market Scope, a leading source for market data, independent perspective, and objective analysis in today’s health-care marketplace, reports that 746,000 laser vision correction procedures were performed in 2019, down slightly from 2018. “We expect 2020 volumes to decrease further, although the magnitude of this decrease is still yet to be determined,” says Kristen Harmon Ingenito, vice president and director of ophthalmics at Market Scope.
Meanwhile, at the practice level, at least some surgeons remain optimistic. During the recent lockdown amid the first wave of the pandemic, some surgeons were forced to stay closed for up to 10 weeks. Most don’t expect that scenario to recur, meaning that ophthalmologists will have a basis of differentiation when explaining the availability of their procedures in the months ahead, even in regions where the number of COVID-19 cases may be spiking and elective procedures are put on hold in hospitals.
Dr. Bond, whose office has a Wavelight Allegretto laser in the surgical suite, believes his operations can continue in a business-as-usual fashion—with hopes that it will be a good time for business in the months ahead.
“I think we have reason to feel confident about our immediate future,” he says. REVIEW
Drs. Donnenfeld, Bond, McKee, Hardten and Shetty have no financial interest in any of the products discussed.



