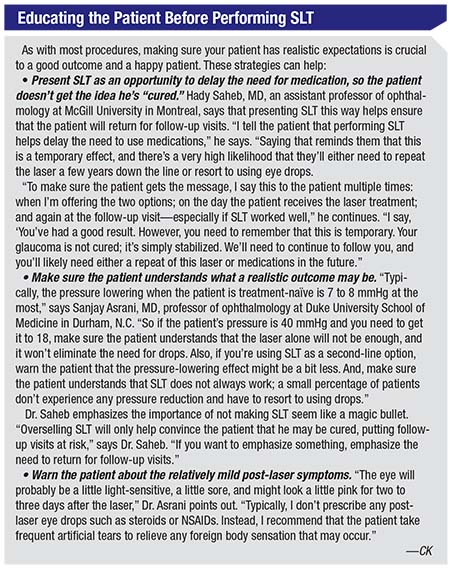
“That sequence is ingrained in many of our ophthalmology colleagues,” says Hady Saheb, MD, MPH, an assistant professor of ophthalmology and director of resident research at McGill University in Montreal. “However, I think there’s enough evidence supporting primary SLT that it’s an option we can justifiably offer to our patients.”1,2
Shan C. Lin, MD, professor of clinical ophthalmology and director of the Glaucoma Service at the University of California at San Francisco, notes that the main reason SLT is not utilized more often is that its efficacy is often mild. “It usually achieves about 20-percent IOP lowering, about the amount of one eye drop, and then its efficacy wanes over time,” he says. “By one year, you have a number of failures; by two years 50 percent of patients or more have had their pressures go back up. By three or four years, almost everyone’s pressures are back up. Of course, that limitation is counterbalanced by the fact that you can repeat the procedure.”
How many doctors are offering first-line SLT to their glaucoma patients? “When I give talks on this to American audiences and ask for a show of hands, about 10 or 15 percent of ophthalmologists appear to be strong advocates of doing SLT first,” says Dr. Lin. “I suspect the vast majority of us will mention it as an option, but not necessarily advocate it; we tend to use medications first. That’s conservative and safe, and in my experience most patients prefer it, because when they hear about laser or surgery they’re often a bit scared and concerned.”
Dr. Lin notes, however, that there’s a certain irony to ophthalmologists not recommending first-line SLT more often. “When I ask the same audience of doctors which they would prefer to start with if they themselves were diagnosed with glaucoma today, half of them usually raise their hands to indicate they’d choose SLT,” he says. “I don’t think it’s that we’re not advocating for our patients as we would for ourselves; I think it’s simply easier to start with eye drops.”
Why Try SLT First?
There’s no question that not having to put in a drop every day—or at least having to put in fewer drops—would be seen as a benefit by nearly every patient successfully treated with SLT. But there are numerous other reasons to consider offering it to your patients as well. Those include:
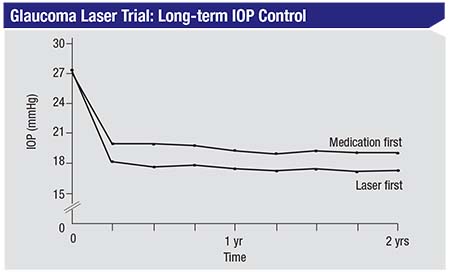 |
| The Glaucoma Laser Trial conducted in the 1980s and ’90s compared primary argon laser trabeculoplasty to primary topical timolol. The laser showed better long-term IOP control.3 |
• Studies support the use of laser before medications. Dr. Lin notes that an early study known as the Glaucoma Laser Trial comparing the use of argon laser trabeculoplasty to medications as a first-line treatment, sponsored by the National Institutes of Health, found that patients starting with ALT had better long-term outcomes than patients starting with medications.3 “This study found that eyes that received ALT first had lower IOP at the long-term follow-up,” he says. “They also had better cup-to-disc ratio scores and visual field scores, and their medication use was lower. Some of the ALT-treated eyes needed to go on medication after ALT, because the laser by itself couldn’t lower the pressure enough in every patient; but at least those patients were using fewer medications at the end of follow-up.
“That study showed that even using the older argon laser, patients were better off doing the laser first,” he says. “And today we can get the same effect using a better laser that’s just as effective as the argon laser, one that doesn’t cause the histological damage to the trabecular meshwork seen with the argon laser, and is repeatable.”
• Doing SLT first may avoid the side effects of topical medications, including dry eye. “Doing SLT first avoids any issues with dry eye, which may be exacerbated by preservatives in the drops, especially in the age group we normally deal with,” notes Sanjay Asrani, MD, professor of ophthalmology at Duke University School of Medicine, director of the Duke Eye Center of Cary and head of the Duke Glaucoma OCT Reading Center in Cary, N.C. “That’s one of the issues that I have in the back of my mind when I suggest trying the laser first.”
• Poor drop compliance puts the patient at risk. “Some studies have found that patients only use their drops about 50 percent as often as prescribed,” notes Dr. Lin. “Other studies have found the number to be closer to 75 percent, but we want patients to use their drops 100 percent of the time. Furthermore, even when patients are trying to use the drops they often fail to get them into the eye, so the compliance studies could even be considered to be optimistic. At least when SLT is done the compliance is 100 percent.”
Dr. Asrani says that if the patient is eligible for SLT or drops and asks for his opinion about which to start with, he tells them his preference would be to opt for the laser first. “Patients using drops occasionally go without the drops for a day or more,” he says. “Whatever the reason, this can lead to a fluctuation of pressure that’s not healthy. It can also stress patients out psychologically, feeling guilty or worrying about the consequences for their eyes. If they have the laser, this isn’t an issue.”
• SLT doesn’t make the patient see himself as sick. “Using drops acts as a daily reminder for the patient that he or she has an eye disease,” says Dr. Saheb. “I think being able to relieve patients of that burden does have some psychological benefit when you start by using SLT instead of drops.”
At the same time, Dr. Saheb notes that this is a double-edged sword. “That also can have a downside,” he notes. “The patient could end up believing that the laser cured his glaucoma—that he no longer needs to be followed.”
• SLT is more effective when used first-line. Dr. Lin points out that—ironically—studies have found that the efficacy of SLT goes down as the number of medications the patient is already on increases. “SLT will be most effective in a virgin eye that has not received any medications yet,” he says. “That’s where you may see 25-percent IOP lowering, possibly more. If you’re on maximal medications, which is the typical scenario in which many ophthalmologists consider performing SLT, it usually doesn’t work well at all, or it has a minimal effect. You’ve already suppressed aqueous production and enhanced outflow so much through medications that the additive effect of SLT is reduced.
“If we follow the recommendation of the studies, including the big NIH study mentioned earlier, we should be offering it to our patients first-line—maybe even encouraging it, because it’s so safe that you have practically nothing to lose,” he says. “Furthermore, it seems to be more effective in the long run when used first-line, even if you have to add medications later on.”
• SLT has a documented contralateral effect.4 “Almost every doctor who does this procedure will tell you that when the patient comes back, a large percentage of the time, the other eye’s pressure is also lower,” notes Dr. Lin. “We don’t really know why, but that’s not a bad thing.”
The Case for First-line Drops
On the other hand, there are a number of arguments for starting glaucoma treatment with topical drops:
• Efficacy. Dr. Lin notes that some of the relative advantages of starting with medications have grown in recent years because of the more potent drugs now available. “Back when the Glaucoma Laser Trial was conducted, the options were not as effective at lowering IOP as today’s prostaglandins, which on average will be more effective than SLT,” he says. “Latanoprost usually lowers IOP about 30 percent. With laser trabeculoplasty, we’re talking about more on the order of 20 to 25 percent IOP lowering, which is more typical for the second-line drugs like timolol, brimonidine and dorzolamide.”
• No risk of a postoperative pressure spike. “Although SLT is very safe, there still is a risk of a pressure spike after the procedure,” says Dr. Saheb. “Certain conditions are particularly at risk for this pressure spike—most importantly, pigment dispersion glaucoma. In those patients, SLT should be used with caution. In other types of glaucoma, a post-procedure pressure spike is a rare complication, but it’s still one that patients and physicians need to be aware of. Reactivating uveitis is also a possibility if the patient has uveitic glaucoma.”
• Patient fears. Clearly, one reason surgeons often favor starting with drops is that many patients are put off by the idea of using a laser on their eyes. “In my experience, most patients will say that the laser sounds ‘a little dangerous,’ ” says Dr. Lin. “That’s ironic, because it’s one of the safest things we can do.”
• Patients are more motivated to return. “Some patients may disappear if they haven’t been educated about their condition and their expected laser outcomes,” notes Dr. Asrani. “If they don’t seem to understand why they’re getting the laser and the nature of the disease, I’d be quite hesitant to proceed with laser as the first-line treatment.”
“If a patient truly has no preference and asks what I’d recommend, I’ll say I have a slight preference for the topical medications,” says Dr. Saheb. “I’m still a little concerned that the patient may be less motivated to return after successful primary SLT, even though I
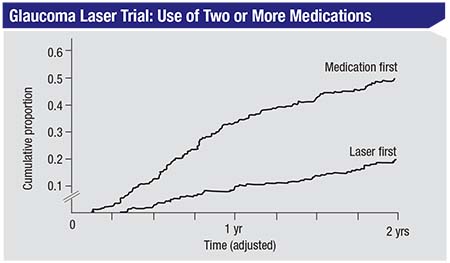 |
| The Glaucoma Laser Trial found that patients who were treated with primary ALT were using fewer medications long-term than those whose primary treatment was timolol.3 |
• SLT doesn’t always work—and if it doesn’t work, the patient may blame the doctor. “Even if the laser was done perfectly there will still be a 10 to 25 percent nonresponse rate,” says Dr. Asrani. “The nonresponding patients may perceive this as surgeon incompetence. On the other hand, if patients don’t respond to a drug, they usually don’t think it has anything to do with the competence of the physician. This might influence some surgeons to just offer drops as primary treatment.”
“In general, this is more likely to be an issue if you’re seeing a patient for the first time,” he adds. “If a patient has been with you for a while, not getting any effect is less likely to be seen as your fault.”
Which Patients Choose SLT?
Although he’s well aware of the advantages of using SLT as a first-line treatment, Dr. Lin says his patients only start with SLT about 10 percent of the time. “I usually do offer first-line SLT to my glaucoma patients,” he says, “especially to younger ones who are busier and don’t like the idea of using eye drops or anything artificial. They’re working individuals who are more concerned about the advantages and disadvantages of the different treatment options. They go online and find that the drops may affect their heart or the color of their iris. They figure out that SLT is just about the safest thing we can do, so they’re much more open to trying it.
“Older patients tend to be more conservative,” he continues. “When you tell them they have to have a laser procedure or surgery—and they tend to equate the laser with surgery—they think of all the bad things that could happen. In contrast, younger people are more in tune with changing technology. Perhaps it’s just because we’re located in the San Francisco area, but our younger patients also seem to be more interested in being holistic. They try to avoid putting anything ‘artificial’ into their bodies, including medications. And of course, they like the convenience of not having to use eye drops.”
Dr. Asrani says that in his experience, two types of patients are most likely to prefer SLT as a primary treatment option. “The first group is young patients who are not used to taking medications on a daily basis,” he says. “They’d rather not take any if they can avoid them. The second group is the aged and infirm patients who are on so many medications they can barely keep up with them, and who may have a tough time getting drops into the eye.”
Dr. Saheb says only a minority of his patients are fearful of the laser. “I make sure to call it a procedure, not a surgery,” he says. “If a patient is still worried, I try to provide a little more information about the nature of SLT so the patient can make an informed decision. I point out that there are no blades or injections or needles, no sterile technique or operating room. However, there definitely is a subgroup of patients who are averse to any kind of procedure. I see no reason to try to persuade those patients, given that we have great medical options.”
Pearls for Patient Selection
One of the caveats for using SLT at any point in your protocol is that not every patient may be an ideal candidate. A few things to keep in mind:
• Be cautious about using SLT in pigmentary glaucoma. “Several studies have shown a paradoxical postoperative spike in IOP with these patients,” says Dr. Lin.6 “We’re not sure why this happens. Maybe the greater pigment in the angle absorbs the laser energy more and causes actual scarring of the trabecular meshwork. Whatever the explanation, some of those patients end up needing surgery, so doctors should avoid using SLT in those patients.”
However, Dr. Asrani believes that pigmentary glaucoma isn’t necessarily a contraindication. “If you can titrate the power when treating pigmentary glaucoma you can avoid a pressure spike and get fairly good pressure lowering,” he says. “In the past I was hesitant to do this, but no longer. Done at very low power, you’ll avoid a post-laser spike and get an effective result.”
• SLT is effective in pseudoexfoliation glaucoma, but watch out for the risk of an IOP spike. “SLT does work in these patients, but they may experience a postoperative pressure spike,” says Dr. Lin.7,8 “That may be related to the release of pigment, which also happens in pigmentary glaucoma.”
• Avoid patients whose glaucoma is associated with inflammation. “This calls for caution on the part of the doctor, because sometimes a patient who has glaucoma that’s associated with inflammation may present without any evidence of inflammation at the time of your evaluation,” says Dr. Asrani. “For that reason, one has to be very careful when taking the history before performing SLT. Be sure to ask if the patient has ever had a red, painful, light-sensitive eye for days on end, is familiar with the words iritis or uveitis, or has taken steroids in the past for what may have been considered an infection by a doctor or by the patient. Also, look for telltale signs of inflammation when performing gonioscopy, such as any cell or flare in the anterior chamber.
“If the patient does have any underlying inflammation, SLT may stir it up,” he continues. “In that situation the patient’s eye pressure can become uncontrolled very quickly—in many cases enough that the patient will need incisional surgery right away. Therefore, it’s vital to avoid treating patients who have inflammation as the cause of their glaucoma.
“If I’m not 110-percent sure that the patient is inflammation-free, I’ll start the patient on a prostaglandin as kind of a litmus test,” he says. “If the patient says the eye drop caused quite a bit of light sensitivity and severe redness and he just can’t tolerate it, then I may be more concerned about the possibility of iritis. This trial is also useful as a way to determine whether the patient is able to manage a drop and remember to take it, and whether the drop has noticeable side effects. Finally, when the patient returns for the laser treatment, I ask if the patient is OK with taking the drop. Does she want to continue with the drop, or just do the laser and stop using the drop?”
• SLT can be useful in primary angle closure after a laser peripheral iridotomy. “Studies have shown that after you’ve opened a closed angle with a laser peripheral iridotomy, SLT will still cause a reduction in IOP,” says Dr. Lin.9 “Don’t be afraid to consider using it in these patients.”
• Don’t underestimate the benefit of reducing IOP fluctuation. “Robert Weinreb’s group, and others, have shown that diurnal fluctuation across 24 hours is dampened after SLT,” notes Dr. Lin.10 “Reducing 24-hour fluctuation in IOP has been associated with less glaucoma progression. So SLT may help the patient even if the pressure doesn’t go down that much.”
• SLT’s pressure-lowering isn’t as great in normal-tension glaucoma patients, but it may still make a difference. “Most doctors will tell you that SLT doesn’t lower the pressure very much in normal-tension glaucoma patients,” says Dr. Lin. “That’s true; according to a number of studies, it lowers IOP 10 or 15 percent, compared to 20 to 25 percent with standard glaucoma.11,12 However, it’s still a statistically significant reduction. The doctor has to decide whether 10 or 15 percent is worthwhile for a given patient. Remember that the patient may also benefit from a reduction in the diurnal pressure curve.”
• Don’t worry about patients minding the need for repeat treatment. Dr. Asrani says in his experience, the laser typically works for at least two years. “For some patients, it lasts 18 months,” he says. “For others, it’s three to four years. In any case, I try to underpromise and overdeliver, so I tell my patients that we may have to repeat it in 18 to 24 months. Once patients have undergone the procedure, they realize it’s relatively simple; it’s just a lens being held on the eye for a minute, without much discomfort, and there are no post-laser precautions or restrictions. So they don’t hesitate if it needs to be repeated.”
Pearls for Using SLT
When performing SLT, keep these strategies in mind:
• Treat 360 degrees, not 180 degrees. “Treating 360 degrees is more effective than partial treatment,” notes Dr. Lin.13 “Some doctors will only do half of the circle; they may come back later and do the other 180 degrees. Papers have shown that treating 360 degrees at one sitting is more effective than treating 180 degrees.”
• Be certain you’re lasering the correct target. Dr. Asrani notes that this is a common surgical error. “Intra-operatively, it’s crucial to make sure you’re lasering the trabecular meshwork, not Schwalbe’s line, which sometimes is pigmented,” he says. “You also must avoid lasering the ciliary body band, which sometimes can be mistaken for the trabecular meshwork.
 |
“This kind of surgeon error may be more common than we realize,” he continues. “This happens mainly to patients who have a very lightly pigmented trabecular meshwork. So, when doing this laser procedure you want to have good gonioscopy skills and be very conversant with the landmarks. Always be sure you’ve identified the correct target before you start the laser.
“Thankfully,” he adds, “if you laser Schwalbe’s line, which is pigmented, you won’t cause any side effects. But again, the treatment will be completely ineffective.”
• Change the angle of the mirror when lasering the nasal and temporal quadrants. “When you’re lasering the superior and inferior quadrants, the laser hits the trabecular meshwork end-on,” Dr. Asrani points out. “However, when lasering the nasal and temporal quadrants, you have to angle the mirror so the beam of the laser hits the trabecular meshwork perpendicularly, not at an angle. If it hits at an angle, you’re effectively only doing 180 degrees of SLT, not 360 degrees, because the lateral sides are barely skimmed with the laser. Moving the mirror and angling it is vitally important.” Dr. Asrani adds that this is why surgeons should take a course or work with an experienced surgeon before attempting SLT.
• Be on the lookout for a postoperative pressure spike. Dr. Asrani explains that there are two different types of pressure spike that can sometimes happen after SLT. “The first kind of post-laser spike happens randomly to about 15 or 20 percent of SLT laser patients,” he notes. “It’s usually short-lived, and we have no way of predicting who’s going to spike. For that reason we typically make every patient wait in the office after their SLT to confirm that there’s no pressure spike. If there is, we bring the pressure back down before we let the patient go home.
“The other category of pressure spike is the kind in which the pressure goes very high within about a week,” he adds. “Those patients—typically cases of uveitis-associated glaucoma that we missed—will have a bad headache and haloes around lights because the pressure has gone into the 50s and 60s. Those eyes will need incisional surgery. However, this is quite rare.”
• Don’t worry about diminished efficacy if you’re adding SLT to a prostaglandin. “There’s some concern about the efficacy of SLT when patients are already on prostaglandin monotherapy, because prostaglandins and SLT appear to work through a similar mechanism of action—increasing outflow—and perhaps through similar molecular mechanisms as well,” says Dr. Lin. “However, at least one study found that SLT’s efficacy is similar to initial therapy in this situation.14 So having a prostaglandin on board—the most common first drop in the U.S.—does not appear to reduce the benefit of SLT.”
• Be cautious about using steroid drops postoperatively. “In theory, steroid treatment after SLT may reduce its efficacy,” says Dr. Lin. “I just use one steroid eye drop immediately after the procedure, as opposed to continuing it for several days. However, at least one study found that postoperative steroid drops didn’t affect the efficacy of the procedure.”15
• Consider offering SLT as a second option. “SLT acceptance among glaucoma patients is very high when it’s offered in place of a second eye drop,” notes Dr. Asrani. “Typically, the first-line drops are prostaglandins that are dosed once a day. A second eye drop will give you at least an additional 20-percent drop in pressure, but it’s typically taken two to three times a day, which is not very practical for most people. So that’s the point at which many patients are willing to try SLT, if they haven’t already done it as the first-line treatment. I would definitely recommend trying it before advancing to a second eye drop.”
Dr. Saheb agrees, noting that some patients may also be more receptive to the laser as a result of having taken a drop. “The first time you suggest treatment is always the biggest shock,” he says. “I do find that some patients who start with medications and need further treatment are more open to laser treatment after a year or two of accepting their disease than they are upon initial diagnosis. Plus, they know how inconvenient drops can be. If the patient is having difficulty remembering to take a drop once a day, the idea of taking one bottle once a day and a second bottle twice a day can be overwhelming. Furthermore, every time you add another drop, the likelihood of the patient remaining compliant and adherent goes down. And of course, SLT as a second treatment will avoid any side effects and preservatives that would be associated with additional medications.”
Looking Ahead
Dr. Asrani notes that new SLT techniques are being developed that may make it easier to apply the treatment without gonioscopic skill and may cause even less post-treatment discomfort. “A recent paper from Michael Belkin, MD, in Israel, tested the efficacy of applying SLT externally to the sclera of the eye,” he says.16 “This approach was nearly as effective as the standard technique, and it might be more appealing to surgeons because it doesn’t require gonioscopy skills. Of course, the popularity of SLT may also be affected by the advent of new, more effective drops, and new drug delivery techniques that might eliminate many of the downsides of using today’s drops.”
Dr. Lin adds that new drug options will also have an impact. “We’re soon going to have options such as latanoprostene bunod, which is a modification of latanoprost, and rho kinase inhibitors like the one under FDA consideration from Aerie Pharmaceuticals,” he says. “I think both of those will be approved this year, and they’ll change the landscape. Studies show that latanoprostene bunod works even better than latanoprost.17 Previously, if latanoprost didn’t work, you might move on to SLT. Now you’ll have another tool on the medication side that might lower pressure 33 to 35 percent. The patient doesn’t do any more work if you switch drops; she’s still using one drop a day, but she may get more efficacy from the same effort. So SLT’s role may be modified as these new drugs become available.” REVIEW
Dr. Saheb is a consultant for Alcon Novartis, Allergan, Bausch + Lomb, Johnson & Johnson Vision, Glaukos and Zeiss, and has research grants with Ivantis and Aerie Pharmaceuticals. Dr. Lin is a consultant for Allergan, Aerie, Eyenovia, AlEyeGN and Iridex. Dr. Asrani has no financial ties to any product discussed.
1. Li X, Wang W, Zhang X. Metaanalysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol 2015;15:107.
2. Wong MO, Lee JW, et al. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol 2015;60:1:36-50.
3. The Glaucoma Laser Trial (GLT) and glaucoma laser trial follow-up study: 7. Results. Glaucoma Laser Trial Research Group. [No authors listed] Am J Ophthalmol 1995;120:6:718-31.
4. Rhodes KM, Weinstein R, et al. Intraocular pressure reduction in the untreated fellow eye after selective laser trabeculoplasty. Curr Med Res Opin 2009;25:787-96.
5. Fea AM, Ahmed II, Lavia C, et al. Hydrus microstent compared to selective laser trabeculoplasty in primary open angle glaucoma: one year results. Clin Exp Ophthalmol 2017;45:2:120-127.
6. Harasymowycz PJ, Papamatheakis DG, et al. Selective laser trabeculoplasty (SLT) complicated by intraocular pressure elevation in eyes with heavily pigmented trabecular meshworks. Am J Ophthalmol 2005;139:1110-3.
7. Kent SS, Hutnik CM, et al. A randomized clinical trial of selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with pseudoexfoliation. J Glaucoma 2015;24:5:344-7.
8. Bettis DI, Whitehead JJ, et al. Intraocular pressure spike and corneal decompensation following selective laser trabeculoplasty in patients with exfoliation glaucoma. J Glaucoma
, 2015;25:4, e433-e437.
9. Ho CL, Lai JS, Aquino MV, et al. Selective laser trabeculoplasty for primary angle closure with persistently elevated intraocular pressure after iridotomy. J Glaucoma 2009;18:563-6.
10. Kóthy P, Tóth M, Holló G. Influence of selective laser trabeculoplasty on 24-hour diurnal intraocular pressure fluctuation in primary open-angle glaucoma: a pilot study. Oph Surg Laser Imaging 2010;41:342-7.
11. Lee JW, Liu CC, Chan JC, Lai JS. Predictors of success in selective laser trabeculoplasty for Chinese open-angle glaucoma. J Glaucoma 2014;23:5:321-5.
12. Tojo N, Oka M, et al. Comparison of fluctuations of intraocular pressure before and after selective laser trabeculoplasty in normal-tension glaucoma patients. J Glaucoma 2014;23:8:e138-43.
13. Prasad N, Murthy S, Dagianis JJ, Latina MA. A comparison of the intervisit intraocular pressure fluctuation after 180 and 360 degrees of selective laser trabeculoplasty (SLT) as a primary therapy in primary open angle glaucoma and ocular hypertension. J Glaucoma 2009;18:157-60.
14. Singh D, Coote MA, et al. Topical prostaglandin analogues do not affect selective laser trabeculoplasty outcomes. Eye 2009;23:2194-9.
15. Realini T, Charlton J, Hettlinger M. The impact of anti-inflammatory therapy on intraocular pressure reduction following selective laser trabeculoplasty. Oph Surg Laser Imaging 2010;41:100-3.
16. Geffen N, Ofir S, Belkin A, et al. Transscleral selective laser trabeculoplasty without a gonioscopy lens. J Glaucoma 2017;26:3:201-207.
17. Weinreb RN, Ong T, Scassellati Sforzolini B, et al; VOYAGER study group. A randomised, controlled comparison of latanoprostene bunod and latanoprost 0.005% in the treatment of ocular hypertension and open angle glaucoma: The VOYAGER study. Br J Ophthalmol 2015;99:6:738-45.



