Even as patients have more options than ever to correct symptoms of presbyopia, whether with newly approved drops or IOLs, their satisfaction with monovision LASIK hasn’t waned. The procedure is as popular as ever with patients, provided they meet the right criteria. Experts say that patient selection is critical for successful outcomes.
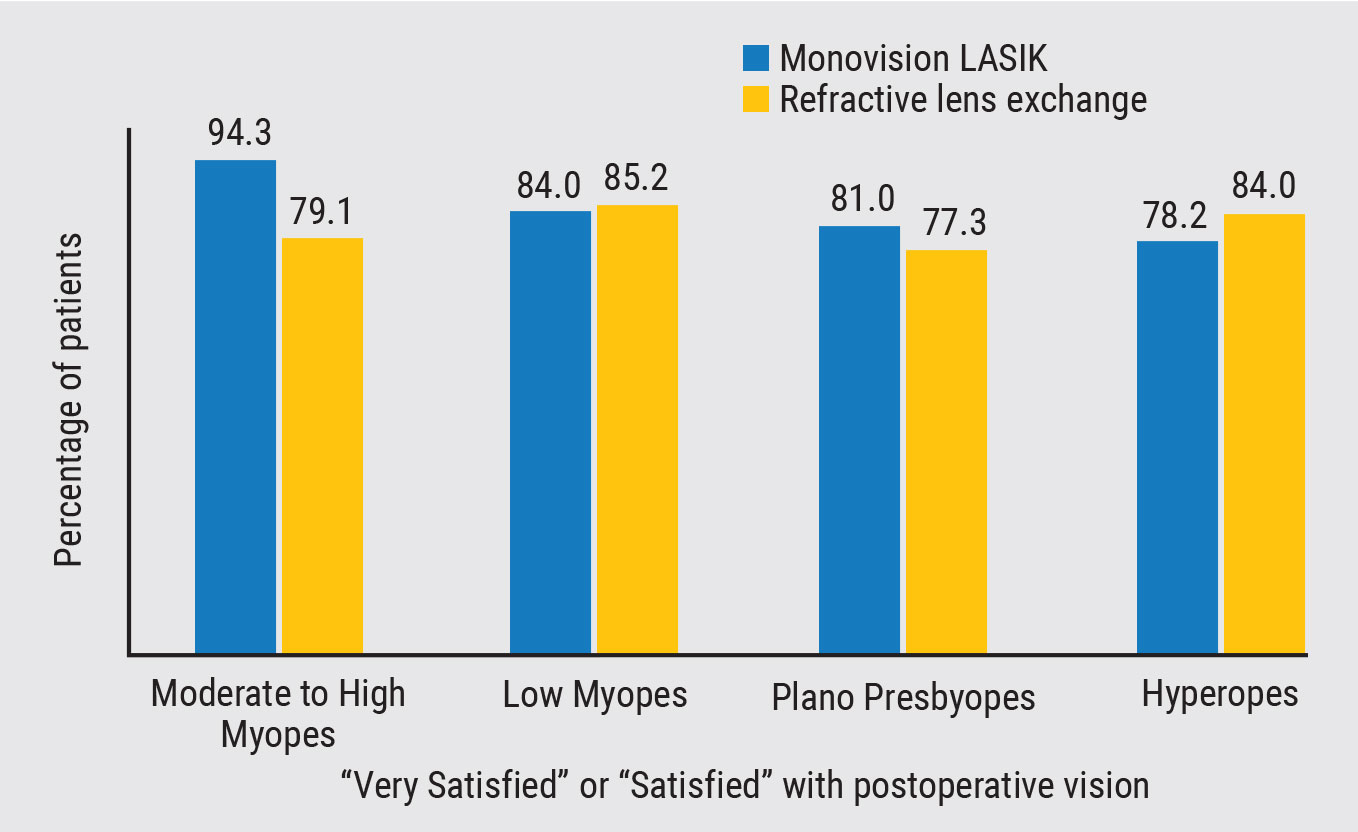
A study of 590 patients with refractive lens exchange and 609 patients with monovision LASIK,1 showed a significant statistical difference in patient satisfaction, depending on their level of myopia. More than 94 percent of those with moderate to high myopia favored monovision LASIK, versus 79.1 percent for refractive lens exchange. The study showed that there was no significant difference in patient satisfaction within the other refractive categories.
Chair time and preoperative expectations are not to be overlooked, and we spoke with some veteran refractive surgeons who offered their insight on patient selection, targets and outcomes.
Prepping the Patient
 |
|
Figure 1. Monovision LASIK continues to have high patient satisfaction rates in the right candidates.1 |
Discussions about presbyopia treatment may begin as early as a patient’s late 30s, according to Kathryn M. Hatch, MD, director of refractive surgery at Mass Eye & Ear, and an assistant professor of ophthalmology at Harvard Medical School.
“I start talking about presbyopia with patients who may be approaching it in the coming decade. It’s good for all patients to know what it is because in general, presbyopia is a different issue from other refractive errors like myopia, astigmatism and hyperopia,” Dr. Hatch says. “Certainly, patients in their 40s and older who already need some sort of reading correction are finding out their options.”
J. Bradley Randleman, MD, a professor of ophthalmology at the Cole Eye Institute of the Cleveland Clinic Foundation, says anyone over age 40 is a potential candidate for monovision LASIK. “By that point, a vast majority of us need near, or at least intermediate and distance vision, interchangeably most of the time,” he says. “Short of restoring accommodation—which we just can’t do currently, and may never be able to do—we’re going to have a vast majority of the population who needs something for multiple distances, and that’s the starting criteria.”
There are some sets of patients that can be eliminated early on in the screening process, he continues. “People who don’t have optimal equal vision in both eyes may not be candidates, so someone with amblyopia doesn’t tend to do as well with monovision,” says Dr. Randleman. “We also make sure to screen for any history of strabismus or some sort of -phoria or -tropia where dissociating their refractive error would increase the risk of them developing double vision.”
A person’s occupation and daily activities may also make them think twice about the procedure. “Pilots, commercial drivers, athletes—they all need a certain level of acuity while doing their jobs. That doesn’t mean they can’t have monovision, but they would need to have it partially, if not fully, corrected,” Dr. Randleman advises. “Somebody who’s doing real near tasks all the time isn’t going to tolerate even a small amount of undercorrection or a small amount of monovision, but somebody who’s doing primarily distance-related activities, may not really notice a big change in their functional near vision until a little bit later.”
The most obvious group of patients eligible for monovision LASIK would be those who already have some level of monovision in their contact lenses, says Dr. Hatch. “Someone who is already undercorrecting their myopia and over the age of 45 would be the ideal person to get monovision LASIK immediately.”
Discussing expectations and putting the patient in a contact lens trial can influence the treatment plan.
“It’s important for people to understand that having LASIK, even with monovision LASIK, sometimes pushes patients into readers a little bit earlier,” Dr. Hatch says. “Someone who might be a low myope and only wears glasses for distance correction might not necessarily understand right away that if we correct both eyes for distance they’ll need reading glasses immediately. There has to be some significant discussion with those patients, because it can be very disconcerting for a low myope to suddenly need correction to see their watch or their phone.”
Dr. Randleman says every procedure has its inherent trade-offs. “That’s just the reality as we age. The better we make your distance vision the worse we make your near, and vice versa. By definition, the eye that we leave myopic isn’t going to see quite as well as the other eye now,” he says. “If their distance vision feels blurred all of the time, then they’re not tolerating monovision. Nighttime vision may be a little more impaired, so a good monovision patient might have a light pair of glasses in the car that they wear occasionally. Same goes for near. We want you to be able to pick up a menu and read it, but if you’re going to sit down and read a novel, you may end up wanting both eyes to be clear for that, so you might have a pair of readers that you use for specific activities.”
These scenarios lead to a trial period of the monovision in contact lenses. “For a monovision trial, we’ll typically send them home with their homework assignment, if you will, because we really want to see how this option will work in their environment, not just in our office or on our eye chart,” Dr. Randleman says.
Dr. Hatch says she likes her patients to undergo the trial for at least a week to see how they tolerate it. “Some patients love it and others say they couldn’t get used to it, but even in those patients, I come up with ways to adjust the targets that’ll work for them,” she says.
Mini-monovision is the New Normal
Vision needs have evolved with the advent of handheld devices, and as a result, the refractive targets for monovision LASIK procedures have also changed.
“We really have three or more ranges of vision: distance; intermediate; and true near,” says Dr. Randleman. “Most of our world now is in the distance and intermediate categories. Computer screens, smartphones and menus tend to be intermediate, and refractive surgeons don’t do quite as much true monovision anymore—when one eye is set for real, functional near and the other is set for distance. Much more commonly we’re doing a distance target and an intermediate target.
“When I started in the early 2000s, a true monovision target was more like a -2.5 D,” Dr. Randleman continues. “I can’t remember the last time I targeted a patient with that much myopia. Now, the average person in their 40s is going to be around -0.75 D in the near target, unless their specific needs or profession dictates otherwise. Patients in their 50s will generally push up to potentially a -1.5 D. Usually, somewhere between -0.75 D and -1.25 D is more than adequate.”
These ranges were typically referred to as “mini-monovision” or “micro-monovision,” he says, but are the norm for monovision procedures currently.
Dr. Hatch has been targeting mini-monovision for patients who say they don’t want monovision LASIK. “I’ve had many patients over the years say they didn’t want the procedure, and then they end up with full correction in both eyes,” she says, recalling a 48-year-old patient who didn’t like the feeling of having one eye undercorrected. “I suggested we do a full correction but in the non-dominant eye we would do a slight undercorrection, a -0.25 D to -0.50 D, so it wouldn’t be enough to notice a huge difference with both eyes open. At least she would see her watch, dashboard and basic things at intermediate level, although ultimately she’d need reading glasses.”
Dr. Hatch says she refers to this as a “slight age adjustment” with patients. “I’ll tell people I’m going to do a slight age adjustment in their non-dominant eye to ensure they don’t end up overcorrected,” she says. “They may not have a crisp 20/20 for distance, they might be 20/25, but their other eye is 20/20. They really can tolerate that very well. Even though some patients say they don’t want monovision, I’m doing this age adjustment, because who wants to put on glasses to look at their watch?”
Enhancements may be common with certain patients undergoing monovision, Dr. Hatch continues. “If you end up not nailing the distance eye, then you have two eyes undercorrected, so you may need to be prepared for enhancements, especially if you’re dealing with higher myopes,” she says. “Achieving your refractive target is extra important.”
Refractive surgeons may even want to consider doing one eye at a time, particularly in low myopes. “You treat the dominant eye first to get the distance and let people try it,” Dr. Hatch says. “I’d much rather do the eyes separately than be in a situation where patients feel regretful and then I have to do some sort of reversal laser procedure.”
Dr. Randleman agrees. “In patients who are hyperopic, we have to overtreat them. Then, if they don’t like monovision, we have to essentially undo that with a different type of ablation, so I’m much more keen on really making certain we like that strategy before doing those surgeries,” he says, which further emphasizes the importance of testing and trials.
“Every patient is so different, it’s literally impossible to predict ahead of time,” Dr. Randleman avers. “We have these broad ranges, but we refine them based on how much difference between the two eyes the patient can tolerate.”
Outcomes and Patient Satisfaction
 |
|
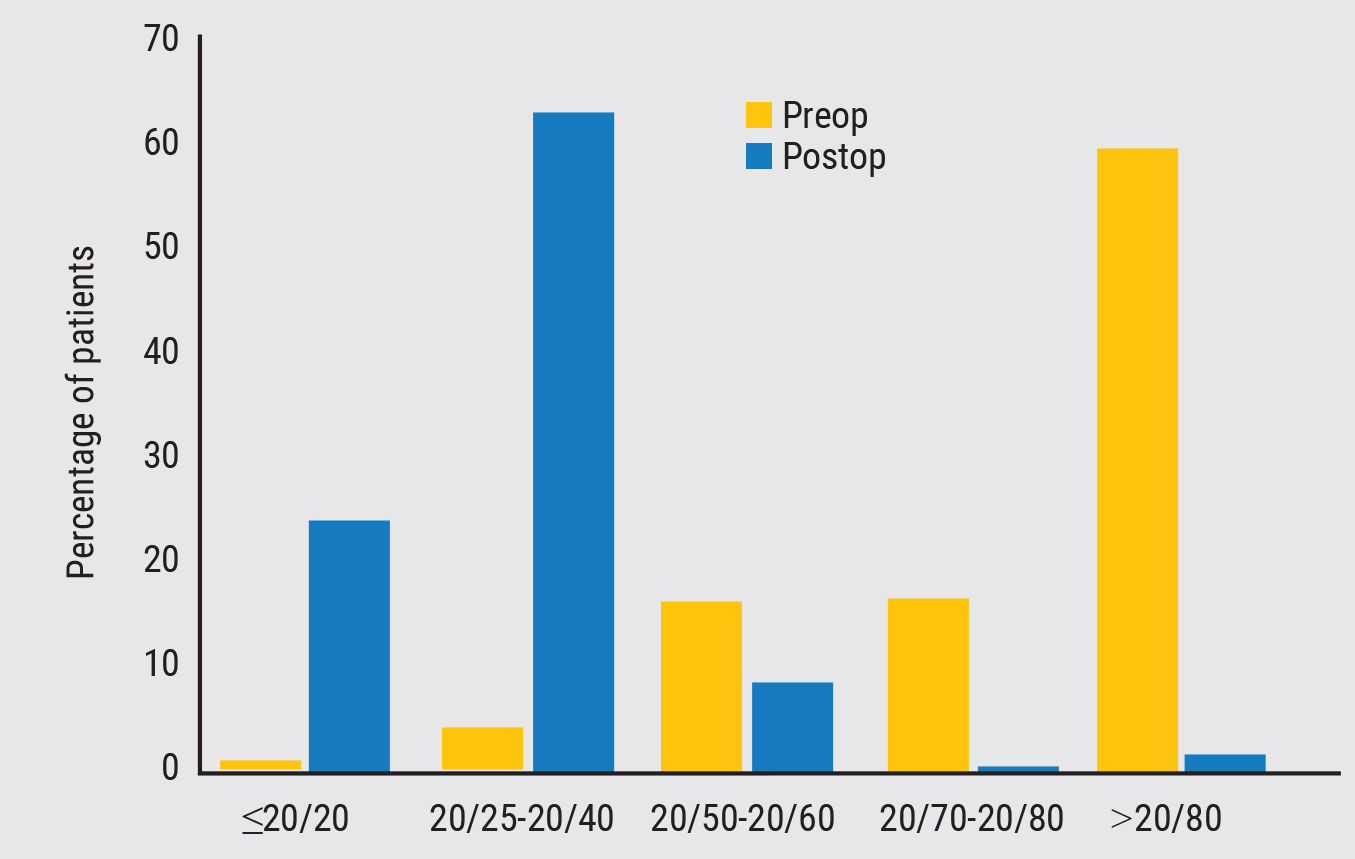
Figure 2. One study showed near acuity improved to 20/40 or better in more than 88 percent of patients who underwent monovision LASIK.3 |
Postoperatively, patients will experience many of the initial side effects that are common with any LASIK procedure, says Dr. Randleman, including increased glare and halos at night or in dark situations. Side effects have been shown to be more prevalent in monovision hyperopes.2 “Patients can also have a little bit of dryness early on, and that will take away some of the crispness of the vision until it recovers. When you add monovision, you need to give it a little bit of time to figure out which of those factors is really an issue and which ones are just part of early healing,” he says.
Monovision will take a bit longer to adjust to, he continues. “It’s not uncommon for people to be aware of the fact that they’re seeing distance with one eye and near with the other, but the ultimate goal is for that to become integrated to the point where they’re just seeing,” says Dr. Randleman. “We don’t want patients to be particularly mindful of which eye is functioning at which distance in the long term. It’s an unconscious process that just has to happen.”
Some patients can be fully recovered within one week, while others may be slower. “If they’re still noticing some differences at three months, but they recognize it’s getting better week after week, then they’re just on the slow side of recovery. That’s not unheard of,” Dr. Randleman says. “But if it’s still awful with no improvement, then we may be looking at reversing the monovision.”
He recommends another contact lens trial in this situation to determine if it’s really the monovision causing the issues.
Monovision LASIK continues to show positive results in patients. One study of presbyopic emmetropic patients showed near acuity improved to 20/40 or better in 88.9 percent of patients with recorded postoperative near reading acuity, and the UCDVA in the distant eye was 20/20 or better in 89.8 percent and 20/25 or better in 98.3 percent.2
Dr. Randleman says the number of patients who like this procedure is quite high. “Other options, such as a multifocal contact or progressive glasses, can still be a little distorting optically,” he says. “They all change the optics a bit more than monovision. Monovision is simply your normal optical process, but with a specific focal point, so you’re not changing anything about the function of the eye.
“Secondly, it’s much easier in my estimation for someone to work around a part-time need for glasses or contacts, as opposed to working around tolerance issues with multifocality,” Dr. Randleman adds. “That’s why I think monovision will continue to be often used.”
Dr. Randleman and Dr. Hatch report no relevant financial disclosures
1. Schallhorn SC, Teenan D, Venter JA, Schallhorn JM, Hettinger KA, Hannan SJ, Pelouskova M. Monovision LASIK versus presbyopia-correcting IOLs: comparison of clinical and patient-reported outcomes. J Refract Surg 2017;1;33:11:749-758.
2. Goldberg, DB. Comparison of myopes and hyperopes after laser in situ keratomileusis monovision. J Cataract Refract Surg 2003;Sep;29:9:1695-701.
3. Peng MY, Hannan S, Teenan D, Schallhorn SJ, Schallhorn JM. Monovision LASIK in emmetropic presbyopic patients. Clin Ophthalmol 2018;12:1665-1671.