Presentation
 |
A 35-year-old Hispanic male with a history of polysubstance abuse presented to an outside emergency room with right eye pain, redness, swelling and vision loss after a presumed alkali chemical exposure the day before. The patient reported that someone accidentally sprayed him from several feet away with a mixture of “cocaine, heroin, fentanyl, meth and dirty water” from a syringe. He then injected these same substances intravenously. His recollection of subsequent events was admittedly suboptimal, stating that he “passed out for multiple hours” shortly after the alleged exposure. He awoke the following morning with the above presenting symptoms, leading him to seek care later that day at an emergency room.
At the ER, the pH of the patient’s right eye was 9 but improved to 7 after irrigation with 10 L of normal saline. In the right eye, vision was hand motion, intraocular pressure was 23 mmHg, and motility was globally limited in all gazes. The right pupil was minimally reactive and miotic, and the ER physicians were unsure of the presence of a relative afferent pupillary defect. Examination of the left eye was within normal limits.
Bedside examination of the right eye with a 20-D lens revealed extensive 3+ conjunctival injection, subconjunctival hemorrhage and chemosis with mild edema and erythema of the upper and lower lids (Figure 1). The cornea demonstrated mild, diffuse haze without epithelial defects, symblepharon or limbal whitening. The lens appeared clear, and the view to the posterior segment was limited secondary to cooperation and miosis. Examination of the left eye was normal.
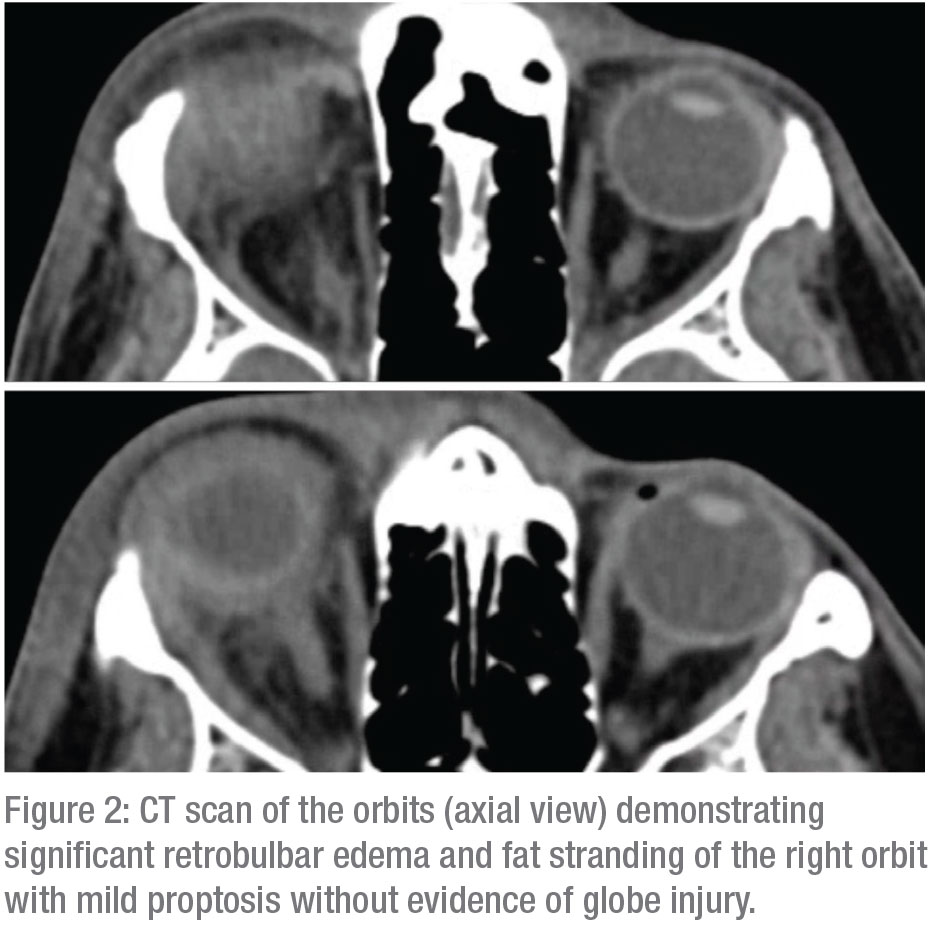 |
CT scan of the orbits demonstrated significant retrobulbar edema, fat stranding and mild proptosis without evidence of globe injury (Figure 2). Bedside ultrasound revealed choroidal thickening with a positive T-sign and mild vitritis. No retinal detachment or obvious penetrating globe injury was noted. CT angiogram of the head and neck, and transthoracic echocardiogram were unremarkable. Laboratory investigation was within normal limits and included a complete blood count, complete metabolic panel, angiotensin-converting enzyme, rapid plasma reagin, anti-neutrophil cytoplasmic antibody, rheumatoid factor, quantiferon-TB gold and Lyme titers.
The patient was admitted for inpatient observation and initiated on aggressive lubrication with preservative free artificial tears and erythromycin ointment, as well as topical ofloxacin, prednisolone acetate, cyclopentolate drops, oral vitamin C and intravenous vancomycin, piperacillin/tazobactam and methylprednisolone. Over the next four days, his vision decreased to light perception in the right eye despite improving chemosis and a grossly clear cornea. At this time, the providers were concerned for etiologies separate from chemical exposure causing vision loss, and he was transferred to Wills Eye Hospital for further evaluation.
Medical History
Past history: polysubstance abuse of alcohol, marijuana, cocaine, opiates and amphetamines; and a history of intravenous drug use. No prior ocular history. No systemic or ocular medications at presentation.
Examination
Ocular examination at Wills demonstrated visual acuity of bare light perception in the right eye and 20/20 in the left. The right pupil was pharmacologically dilated with a 3+ RAPD by reverse; the left pupil was round and briskly reactive. IOP was 7 mmHg in the right eye and 13 mmHg in the left. There was improved, but still limited, motility in all gazes on the right with full motility on the left.
Anterior slit lamp examination of the right eye revealed improving 1-2+ injection and trace chemosis without any limbal whitening or symblepharon. The cornea had dense superficial punctate keratitis, mild edema and a few Descemet’s folds. There was a white cataract with pigment on the anterior lens capsule in an annular distribution and scattered broken posterior synechiae (Figure 3). There was no view to the posterior segment. Anterior and posterior segment exam of the left eye was within normal limits. B-scan ultrasound of the right eye revealed vitritis, a shallow serous choroidal detachment, choroidal thickening and a positive T-sign without retinal detachment.
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



